To test when intentional decisions enhance retention in health-promotion interventions, we analyzed the rate of return of 278 clients of HIV-prevention counseling at a state health department in Florida. Specifically, the role of intentions as a facilitator of returns was analyzed as a function of busyness (more children and work hours), while demographic and health factors that also influenced returns were controlled for. Consistent with the notion that actions depend on ability, intentions predicted the behavior of the less busy participants but failed to facilitate retention when participants were occupied with children and work. These findings suggest the efficacy of different retention strategies –one emphasizing explicit intention formation, and the other either attracting clients to counseling on the spot or using more ubiquitous technologies.
Para poner a prueba cuándo las decisiones intencionales promueven la retención dentro de las intervenciones de promoción de salud, se analizó la proporción en que 278 usuarios de consejería de prevención de VIH regresaban al departamendo de salud estatal de Florida. Específicamente, el rol de las intenciones como facilitador de los retornos fue analizado como una función de trabajo (más hijos y más horas laborales), mientras que los factores demográficos y de salud que también tenían influencia fueron controlados. Consistente con la noción de que las acciones dependen de la habilidad, las intenciones predijeron la conducta de los usuarios menos ocupados y no predijeron en los casos de usuarios con mayor carga de trabajo e hijos. Estos hallazgos sugieren la eficancia de diferentes estrategias de retención –una enfatizando la formación explícita de intenciones, y otra ya sea atrayendo clientes a consejería sobre la marcha, o utilizando tecnología más ubicuas.
Enrollment and retention are critical components of the effectiveness of HIV-prevention interventions in real-world conditions (e.g., ordinary health promotion programs without payments for participation) (Albarracín, Durantini, Earl, Gunnoe, & Leeper, 2008; Noguchi et al., 2007). Without enrollment, HIV-prevention interventions cannot impact public health (Albarracín et al., 2008; Holtgrave & Curran, 2006; Noguchi, Durantini, Albarracin, & Glasman, 2007), and without high retention, HIV-prevention interventions have less impact on behavior. An analysis of interventions tested without using payments or other incentives show that retention rates have positive associations with increases in knowledge and motivation to engage in HIV-safe behavior (rs = .67 and .40; Albarracín, Gillette, Earl, Glasman, Durantini, & Ho, 2005). Moreover, recently estimated associations for behavior change show that interventions with less than 50% retention produce a long-term decrease in HIV-safe behavior (d = ─0.29) vs. an increase in HIV-safe behavior (d = 0.41) for 100% retention (Johnson et al., 2007). In this paper, we investigated the role of return intentions as a psychological mechanism underlying retention in these interventions.
Increasing retention is vital for public health because multi-session behavioral interventions to reduce HIV risk are often more efficacious than single-session ones (Albarracín, et al., 2005; Johnson et al., 2007). For example, the positive behavior change elicited by HIV-prevention interventions for clients of STI clinics is d = 0.33 for multi-session programs vs. 0.06 for single-session programs (analyses of the data from Albarracín et al., 2005). However, when tested under conditions similar to the ones that are likely during actual implementation (e.g., lack of payments or other incentives), these multi-session interventions show relatively low retention (Noguchi et al., 2007). Specifically, with the exception of interventions with captive audiences (prisons, inpatients), which show 100% completion, experimental interventions without payments show a rate of completion of around 50% for initially enrolled participants (Branson, Peterman, Cannon, Ransom, & Zaidi,1998; McMahon, Malow, Jennings, & Gómez, 2001). As these worrisome findings indicate, research on retention in HIV-prevention interventions matters tremendously. We believe that it is our responsibility to understand retention in existing HIV-prevention programs.
In this work, we investigated the role of intentions to return to upcoming sessions as a determinant of return rates. Retention was measured in a CDC recommended, client-centered, cost-effective HIV-prevention counseling model (Holtgrave, Valdiserri, Gerber, & Hinman, 1993) shown to significantly reduce STIs in large multi-site studies (Kamb et al., 1998; Metcalf et al., 2005). The program provides information, identifies risk behaviors, negotiates explicit steps to change risky behavior, and encourages behavioral skills that allow for safer behaviors. This model usually involves more than one session, with each session lasting at least 20 minutes. Retention was observed over two follow-up session taking place approximately one and two weeks after the first session. Return intentions were measured immediately after the first session.
We hypothesized that intentions would predict retention more strongly when participants have control over their time than when they are burdened with work and family responsibilities. The importance of actual control over behavior has been emphasized in past work (Ajzen & Fishbein, 2005; Fishbein & Ajzen, 2010) and intentions are likely to influence behavior (for a recent demonstration, see Ajzen & Klobas, 2013) more when behavior is under conscious control (Neal & Wood, 2009). In contrast, actual counseling attendance may depend entirely on time availability or family responsibilities, thus decreasing the predictive power of intentions in those conditions. Importantly, highlighting this dynamic should demonstrate some of the conditions under which retention is in fact under the control of the individual, even in a sample that is vulnerable and relatively resource-deprived. The analyses we conducted entailed predicting return rates from return intentions and determining the degree to which busyness, measured by the number of hours participants worked and the number of children they had, moderates the intention-behavior relation.
MethodOverview and DesignThe present study is part of a larger study on retention in HIV-prevention counseling conducted with community members who were at risk for HIV and other STIs in North Florida. Prospective participants were asked several questions to determine eligibility, and only those considered eligible were scheduled to attend an initial study appointment. During the first appointment, which took place at the Duval County Health Department in Jacksonville, FL, the research assistant administered a baseline questionnaire, which included measures of socio-demographics and HIV risk factors. After completing the baseline questionnaire, participants received their first HIV-prevention counseling session. Approximately half of the sample then completed a questionnaire assessing return intentions. This paper is based on the measures available for this sample. Participants scheduled follow-up counseling sessions at the end of the first appointment and their attendance at these appointments was recorded.
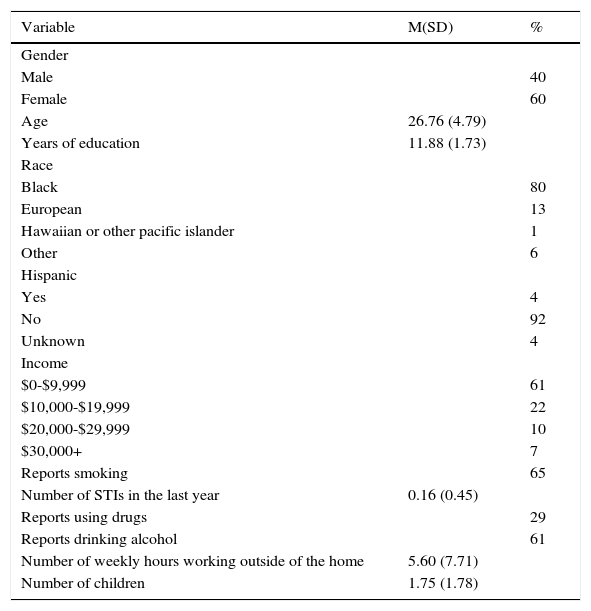
ParticipantsFive hundred and eighty-one eligible study participants attended the initial counseling session. Participants that were randomly assigned to complete or not complete the questionnaire at the end of the session were selected for our analyses. Thus, our analyses included data from 278 clients who completed the measures of return intentions. A description of the sample appears in Table 1 and indicates a predominantly African American, low-income, at-risk population.
Description of the sample
| Variable | M(SD) | % |
|---|---|---|
| Gender | ||
| Male | 40 | |
| Female | 60 | |
| Age | 26.76 (4.79) | |
| Years of education | 11.88 (1.73) | |
| Race | ||
| Black | 80 | |
| European | 13 | |
| Hawaiian or other pacific islander | 1 | |
| Other | 6 | |
| Hispanic | ||
| Yes | 4 | |
| No | 92 | |
| Unknown | 4 | |
| Income | ||
| $0-$9,999 | 61 | |
| $10,000-$19,999 | 22 | |
| $20,000-$29,999 | 10 | |
| $30,000+ | 7 | |
| Reports smoking | 65 | |
| Number of STIs in the last year | 0.16 (0.45) | |
| Reports using drugs | 29 | |
| Reports drinking alcohol | 61 | |
| Number of weekly hours working outside of the home | 5.60 (7.71) | |
| Number of children | 1.75 (1.78) |
Some clients were recruited through flyers placed in the community (e.g., bus stations, employment agencies, shopping centers) and throughout clinics at the Duval County Health Department. Others were recruited from direct referrals from health department staff and members of the community (e.g., staff at community agencies, former participants). To reduce self-selection, the flyers and instructions for direct referrals described the study as related to “health promotion counseling” and made no reference to either HIV or condom use.
Individuals who were interested in participating in the study called a designated number. The research assistant provided an overview of the study and obtained preliminary oral consent for a brief prescreening questionnaire. To be eligible, individuals had to be between the ages of 18 and 35, report having sexual activity (defined as having had vaginal or anal sex) in the past three months, and report using condoms “never” or “occasionally” in the past three months. Recruiters excluded those who planned to move from the Jacksonville area in the next six months, were HIV-positive, had concomitant knowledge of the study, or were trying to get pregnant or had a partner who was trying to get pregnant. Eligible participants were scheduled for their first study appointment. Individuals who were not eligible to participate were debriefed and thanked for their time.
To ensure initial enrollment, intervention recipients were paid $35 for attending the first session, which included baseline measurements plus the first counseling session. They were paid $15 each for attendance at the second and third sessions. The study was approved by the Institutional Review Boards (IRBs) of the University of Illinois, the University of Pennsylvania, and the State of Florida’s Department of Health. Written informed consent was provided to participate in a study described as examining health behavior and involving answering questions about current health practices and participation in counseling. Participants were reassured that their confidentiality would be carefully guarded and that participation was entirely voluntary.
The Counseling ProgramParticipants in the study agreed to participate in HIV-prevention counseling and received appointments for three sessions. The counseling model entailed a one-on-one, client-centered, cost-effective HIV-prevention counseling intervention (Holtgrave et al., 1993; Kamb et al., 1998). Sessions were scheduled one week apart, spread over at least three weeks. Participants received a reminder call the day before their scheduled appointment. In the event of an absence, they were called once in an attempt to reschedule the missed appointment as is usual practice in HIV-prevention services. This accounts partially for the high rate of return.
The first session delivered information regarding HIV transmission and prevention, performed personalized risk assessments, helped the client identify and commit to risk-reduction steps, and ended with a 20-minute video that included a reminder to attend the second session. The second and third sessions explored the success or failure of the steps agreed on during the previous counseling session, and adjusted goals to the participant’s achievements. In addition, the counselor addressed other emotional and instrumental needs, such as unemployment, housing, violence in the home, medical concerns, emotional/mental health, and financial difficulties. Thus, goals and referrals pertaining to these needs were also set during follow-up sessions.
MeasuresThe baseline questionnaire assessed socio-demographic variables including gender, age, education, income, and ethnicity. It also included questions asking whether participants had a main partner and whether they had had a sexual partner they did not consider their main partner in the last three months. We also included items assessing various health perceptions, drug and alcohol use, hours working outside the home, and number of children, in addition to measures of intentions, attitudes, norms, and perceived control.
Retention. The main outcome variable in this study was a dichotomous measure of return to the second session, scored as 1 (return) or 0 (lack of return). For this measure, reports from both the counselor and the research assistant were recorded to ensure reliability. Reliability between the counselor and research assistant observations of counseling retention was high, κ = 1.00, p < .001.
Intentions to return. Participants were asked “How strong is your intention to return to the next session?” and answered this question on a 1 (not at all) to 4 (extremely) scale.
Busyness. We used the average of number of hours working outside the home and number of children, each standardized, as a measure of busyness.
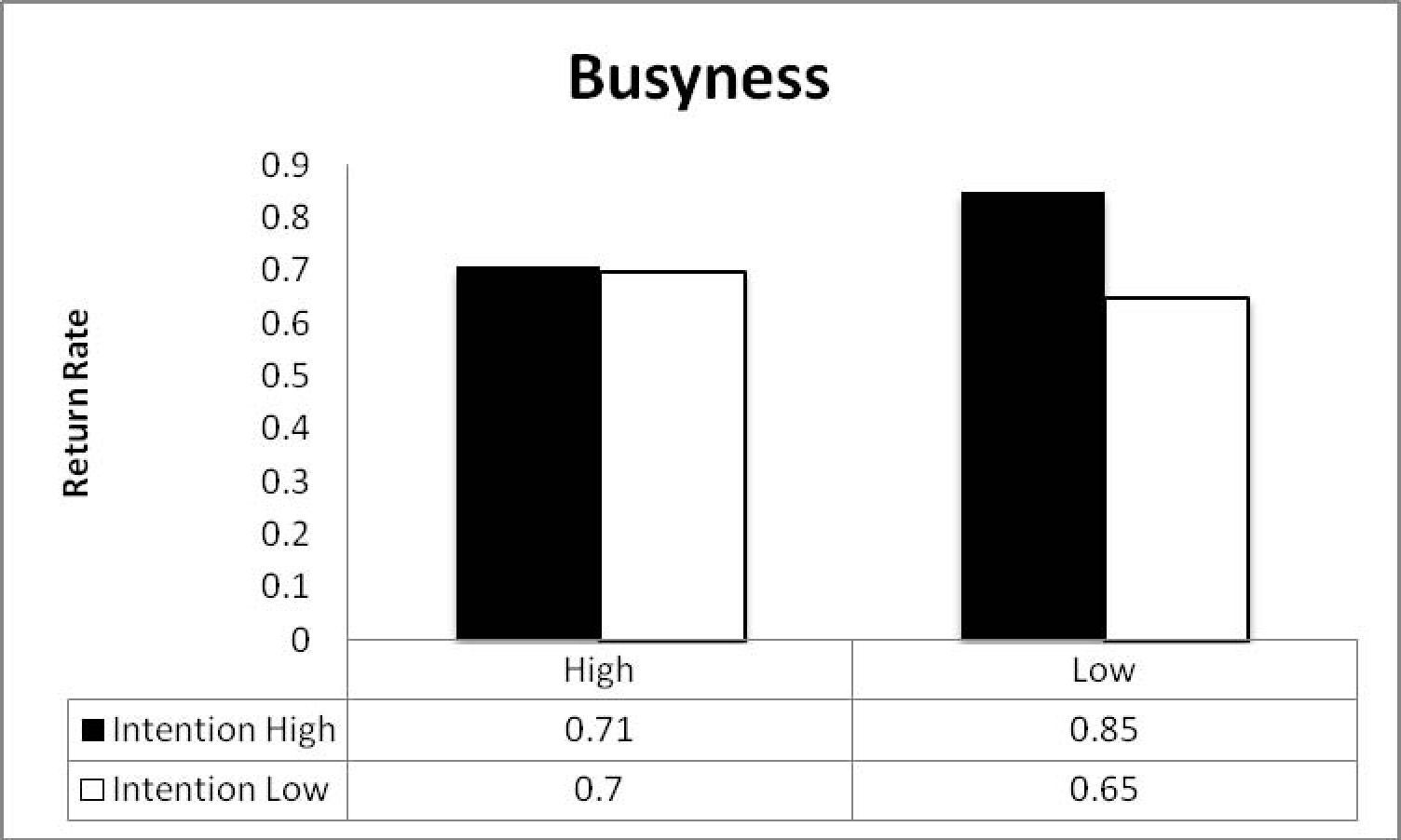
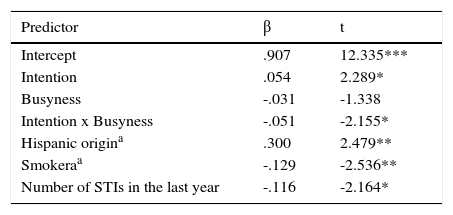
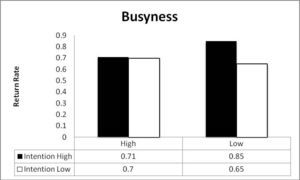
ResultsTo test our predictions of different effects of busyness, the proportion of returns over the two follow up sessions was analyzed as a function of intentions, busyness, the interactions between intentions and busyness, and control variables. The coefficients associated with this analysis appear in Table 2, and the estimated return means at a standard deviation above and below the means for intentions and busyness appear in Figure 1. As shown in Table 2, intentions had an overall positive association with retention but also interacted with busyness. Specifically, intentions predicted behavior when participants were less busy, but did not predict behavior among busy participants.
DiscussionThis results from this study revealed that returning to the follow-up sessions of an HIV-prevention counseling program is sometimes under intentional control. Even in a sample with limited resources, poverty, and racial segregation, return rates did depend on a decision for those clients who had fewer work and family commitments. This finding remained after controlling for variables that also influenced returned rate, such as Hispanic ethnicity.
A number of interventions have been produced to change behaviors that put people at risk for HIV (Albarracín et al., 2005; CDC, 2007b). These interventions are typically tested under conditions that ensure the validity of the outcome assessments (Cook & Campbell, 1979). Thus, researchers try to involve community members to see if a particular intervention works for them. Social networks are called upon to recruit these participants and numerous incentives and facilitators are used to ensure the desired sample of exposed participants as well as low attrition (Exner, Hoffman, Parikin, Leu, & Erhardt, 2002; Lauby et al., 1996; Rabinowitz, 2002; Linnan et al., 2002; Raj et al. 2001; Roffman, Picciano, Bolan, & Kalichman, 1997; Schilling & Sachs, 1993; Schweitzer, 1997; Tobias, Wood, & Drainoni, 2006). Although these procedures are necessary to determine if a program works for an exposed population (efficacy trial), they remove the reluctance to participate that is present when the intervention is implemented (Catania, Gibson, Chitwood, & Coates, 1990; Lauby et al., 1996). In contrast, contemporary research must concern the fundamental scientific problem of variability in exposure to behavioral interventions.
Despite the above-mentioned method of removing selection and attrition during experimental tests of intervention efficacy, in real-world conditions, people can choose to take part in preventive interventions (Albarracín et al., 2008; Condelli, Koch, & Fletcher, 2000; DiFrancesco et al., 1998; Hennessy, Mercier, Williams, & Arno, 2002; Noguchi et al., 2007; Rutledge, Roffman, Picciano, Kalichman, & Berghius, 2002; Veach, Ramley, Kippers, & Sorg, 2000). Given that interventions need to fully reach vulnerable audiences, not just willing ones, it is imperative to develop and test procedures that increase participation by these populations (Albarracín et al., 2008). Procedures can be designed to change an audience’s behavior with respect to the preventive interventions themselves, including enrollment and retention. These procedures, termed meta-interventions, entail a standardized introduction or context change (e.g., delivery setting) intended to increase exposure to a behavioral intervention (Albarracín et al., 2008; Albarracín et al., 2007). The current results suggest the need to strengthen intentions to complete a program for the less time-burdened populations, while structural modifications are put into place for the more burdened groups. Offering HIV services right at the time when a client makes contact with the health system is a promising solution (Phillips & Fernyak, 2000; Weis et al., 2009), as is the use of in-home services and technologies that can reach individuals who are busy with other responsibilities. Recent years have generated both types of services (Chi & Stringer, 2010; Swendeman & Rotheram-Borus, 2010; van Velthoven, Brusamento, Majeed, & Car, 2013; McFarlane, Ross, & Elford, 2004; Muessig, Pike, LeGrand, & Hightow-Weidman, 2013; Kalichman et al., 2005; Horvath et al., 2009), and our findings support the continuation of these efforts.