As a novel infectious disease, COVID-19 is caused by SARS-COV-2, spreading rapidly worldwide. ENT specialists have faced this challenging disease in various ways since the emergence of the COVID-19 pandemic. We are currently facing an increase in cases referred due to sinonasal mucormycosis which is a rare but invasive, rapidly progressive, and life-threatening infection. We provide an overview of this disease's incidence rate and clinical features.
MethodsThis descriptive cross-sectional study was conducted on 46 sinonasal mucormycosis patients who were histopathologically confirmed after sinonasal endoscopic surgery in our educational therapeutic hospital during 2 years of the COVID-19 pandemic from March 20, 2020, to March 20, 2022.
ResultsThere was an increase in the incidence of mucormycosis more than twice as much as before. All patients had a history of COVID-19 and 69.6% were diabetic. The median time to symptom onset from COVID-19 detection was 3.3 weeks. A total of 60.9% received steroids while 85.7% were prescribed during COVID-19 treatment. The most common manifestation was orbital involvement (80.4%). Of the 46 study cases, unfortunately, 17 (37%) died. An exciting point in our study was the incidence of peripheral facial palsy which is associated involvement of multiple other cranial nerves (II, III, IV, V, VI) considered to be the likely occurrence of a rare phenomenon called Garcin's syndrome.
ConclusionBased on the results of this study, during 2 years of the COVID -19 pandemic, there was an increase in the incidence of sinonasal mucormycosis more than twice as much as before.
La enfermedad infecciosa COVID-19, causada por el SARS.COV-2 se ha extendido rápidamente por el mundo. Como otorrinolaringólogos, nos hemos enfrentado a esta enfermedad de diversas maneras durante el periodo de pandemia. Actualmente evidenciamos a un aumento de casos de mucormicosis nasosinusal, infección rara pero invasiva, rápidamente progresiva y amenazante para la vida. Presentamos una descripción general de la incidencia de esta enfermedad, así como sus características clínicas.
MétodosEstudio descriptivo transversal de 46 pacientes con mucormicosis nasosinusal confirmados histopatológicamente en un hospital universitario de Irán desde el 20 marzo de 2020 hasta el 20 de marzo de 2022.
ResultadosEl aumento en la incidencia de mucormicosis ha sido más del doble en comparación con el pasado. Los pacientes todos tenían antecedentes de COVID-19, y el 69.6 % de ellos eran diabéticos. El plazo promedio de aparición de los síntomas ha sido 3.3 semanas desde la detección del COVID-19. Un total de 60.9% de pacientes recibieron esteroides mientras que el 85.7% fueron recetados durante el tratamiento contra el COVID-19. La manifestación más frecuente fue la afectación orbitaria (80.4%). De los 46 casos de estudio, lamentablemente, 17 (37%) fallecieron. Un punto emocionante en nuestro estudio fue la incidencia de parálisis facial periférica que está afectada y asociada con la participación de muchos otros nervios craneales (II, III, IV, V, VI) que se considera que es la probable ocurrencia de un fenómeno raro llamado síndrome de Garcin.
ConclusiónEn base a los resultados de este estudio podemos concluir que la incidencia de mucormicosis nasosinusal se duplicó en Irán durante el periodo de pandemia
Coronavirus disease 2019 (COVID-19) is a novel infectious disease caused by SARS-COV-2, which is rapidly spreading throughout the world.1 The disease is associated with a wide spectrum of manifestation, from mild fever and cough to life-threatening pneumonia. It can also lead to a variety of complications, including anosmia, taste disorders, diarrhea, generalized lethargy, cardiovascular problems, neurologic disease and secondary infections. ENT specialists have faced this challenging disease in various ways since the emergence of the COVID-19 pandemic, initiating with a nasopharyngeal diagnostic test, then with anosmia as a typical marker of the disease, or the presence of a virus in the middle ear.2,3 We are currently facing another link between ENT and COVID-19; Invasive fungal rhinosinusitis following COVID-19 that is a dangerous and potentially deadly consequence. COVID-19 leads to overexpression of inflammatory cytokines, and all the sufferers develop cellular immunodeficiency due to decreased CD4 + and CD8 + T cell counts.4,5 On the other hand, the widespread use of corticosteroids in the treatment of COVID-19 can lead to immune suppression in these patients. Altogether, proliferation of opportunistic infections, including mucormycosis, can occur in the sufferers.6 Mucormycosis is a rare but invasive, rapidly progressive, and life-threatening infection. Before COVID-19 pandemic, the incidence rate of mucormycosis was 0.005–1.7 per million7 with a global mortality of about 46%.8 A definitive diagnosis of mucormycosis can be achieved only through histological examination. Early diagnosis of mucormycosis is so important given that a delay of diagnosis from 6 to 30 days can increase the mortality from 35% to 66%.9 The most common site of involvement is the paranasal sinuses (39%), followed by lungs (24%), skin (19%), brain (9%), gastrointestinal tract (7%), and disseminated type (6%) involvement.10–12 Mucormycosis typically affects immunocompromised individuals including uncontrolled diabetes mellitus, iatrogenic immunosuppression and haematological malignancies, and those who have undergone organ transplantation. Despite rapid diagnosis and treatment of the underlying disease and invasive surgical and medical interventions, the rapid spread of infection often leads to the death of the patient.13 Since the onset of COVID-19 pandemic along with the increase in cases, we have seen increase in cases referred due to sinonasal mucormycosis. Due to prominence of early diagnosis and the high mortality and morbidity of this disease, we decided to investigate the incidence rate and clinical features of this disease during these 2 years of COVID-19 pandemic.
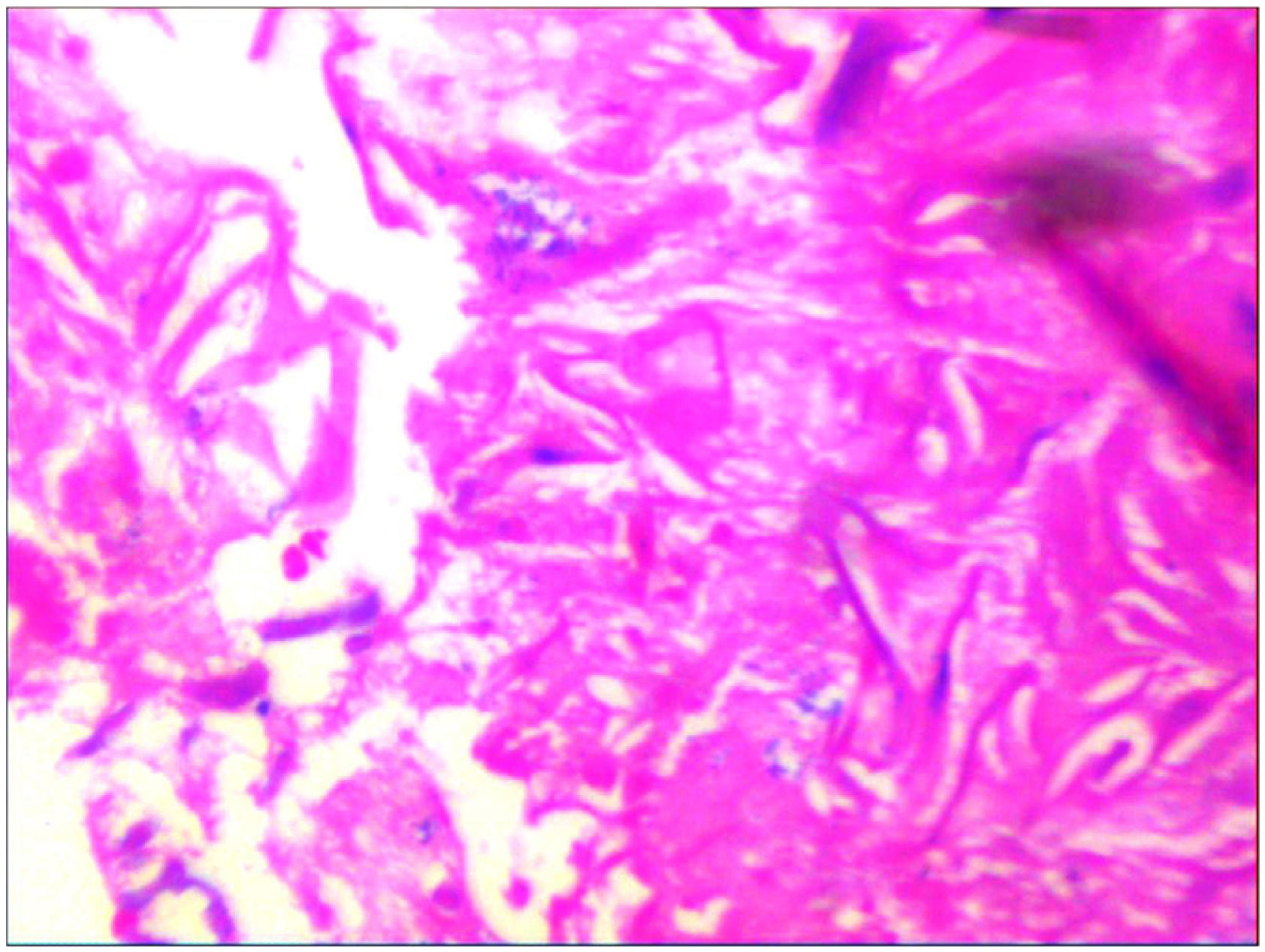
Material and methodsAfter approval by the local Ethics Committee and obtaining written informed consent, this descriptive cross-sectional study was conducted on all sinonasal mucormycosis patients who presented fungal infection of mucormycosis based on histopathological findings (according to the EORTC/MSGERC, 2020, Definitions of Invasive Fungal Diseases; observation of the non-septate, ribbon-like, wide hyphae with right-angle branching in the sterile specimen) (Fig. 1). Patients were definitively confirmed after sinonasal endoscopic surgery in our training hospital during 2 years of COVID-19 pandemic from March 20, 2020 to March 20, 2022. Our institution is the only referral center for ophthalmology and ears, nose and throat (ENT) care in Yazd province. Also patients from different parts of the surrounding provinces are mostly referred to this hospital for the diagnosis and treatment of ophthalmologic and otolaryngologic problems. Patients who were recognized out of this date, patients whose histopathological findings were confirmed as other fungal infections, or cases with incomplete medical records were excluded. During this periode, 70 suspected cases of sinonasal mucormycosis had sinonasal endoscopic surgery indication, but unfortunately, 12 cases before the surgery died due to deteriorating general condition. Of the 70 suspected cases, 11 that were no fungal related on histopathological findings and one that was diagnosed of invasive aspergillosis) were excluded. Therefore this study included 46 definitive cases of sinonasal mucormycosis. We collected patient data (from hospital medical information systems) including: patient demographics; underlying conditions, (diabetes mellitus, malignancy, and usage of corticosteroids); COVID-19 PCR test result at the time of mucormycosis diagnosis; past history of COVID-19 infection and interval between the diagnosis of COVID-19 and the onset of symptoms suspected to be mucormycosis. Patient data about clinical features were also collected including several signs and symptoms such as facial numbness or pain, peripheral facial palsy, mucosal necrotic lesions, orbital involvement and information of exenteration surgery during admission, intracranial involvement based on radiological reports and neurological consultation, involvement of paranasal sinuses separately based on radiological evidence, evidence of black scar during endoscopic surgery and the mortality rate before discharge from the hospital. Data analysis was performed using SPSS (version 25) and Pearson's chi-squared test was used to determining statistically significant differences between variables. P-value <0.05 considered as significant level.
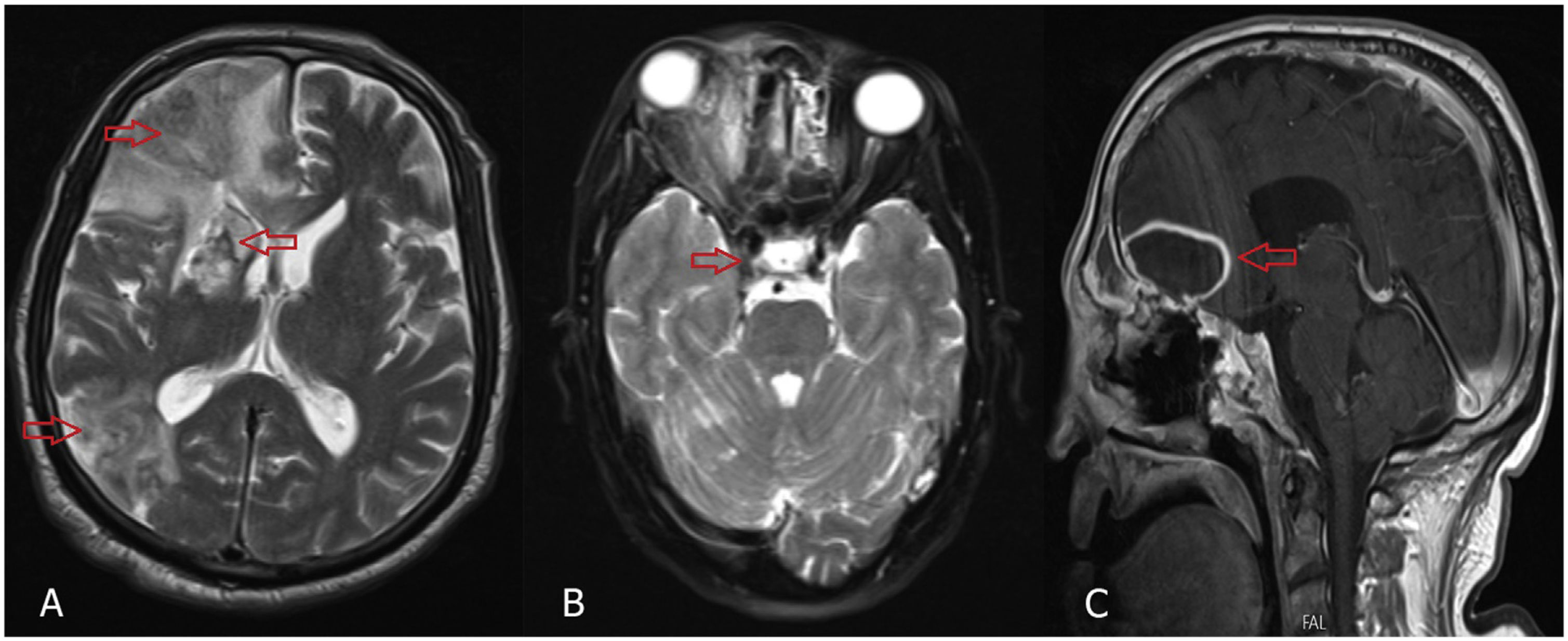
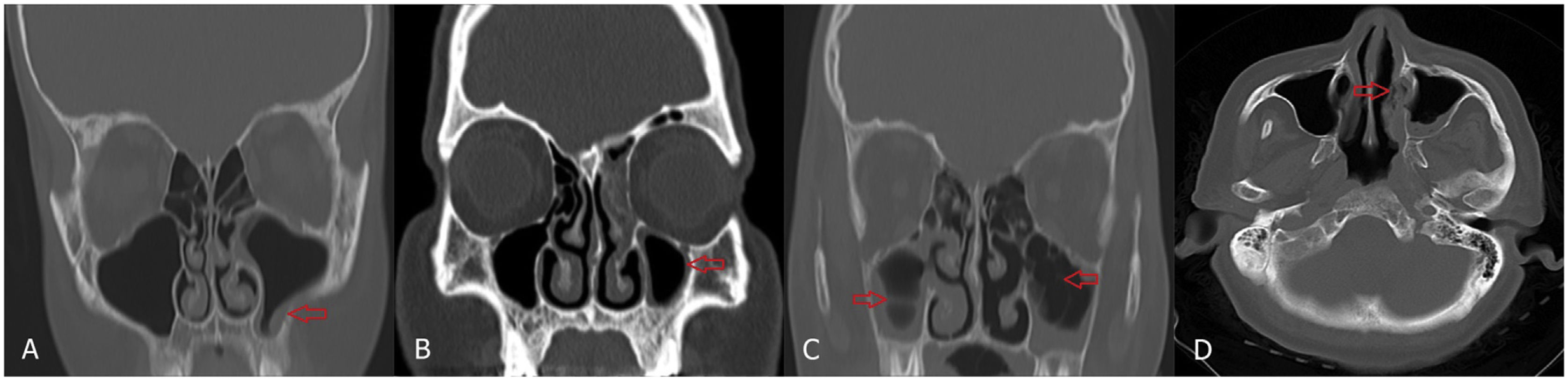
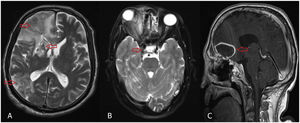
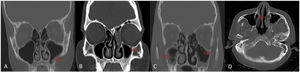
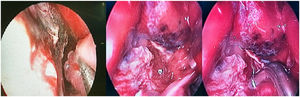
ResultsIn this descriptive cross-sectional study, 46 cases with definitive diagnosis of mucormycosis based on histopathological findings were included. Of the 46 study cases 24 (52.5%) were male and 22 (47.8%) were female with the minimum and maximum ages of 5 and 82 years and the mean age was 52.7 years. All patients had history of COVID-19 infection. At the time of mucormycosis diagnosis COVID-19 PCR test of 71.7% were negative. The time interval between COVID-19 diagnosis and beginning of mucormycosis symptoms was estimated to be 3.3 weeks on average. 69.6% of cases had history of diabetes mellitus. 60.9% of patients had history of corticosteroids usage, which 85.7% were prescribed during COVID-19 treatment. Thirteen percent suffered from malignancy, being the hematologic type the most common (83.3%). In the evaluation of clinical features, the most common manifestation was orbital involvement (80.4%) which was unilateral in all patients. Periorbital pain and edema were the most prevalent symptoms (78.3%). Reduction of visual acuity was repoted in 71.7% of our patients. Nineteen cases (41.3%) completely lost the unilateral eye vision and 17 cases of them also had also a Frozen Eye in examination (Fig. 2). After ocular involvement, facial pain (78.3%), facial numbness (63%) and peripheral facial palsy (26.1%) were the more frequent symptoms. Oral necrotic lesion was seen in 23.9% of patients (Fig. 3). The results showed that 6 patients (13%) had intracranial involvement. There were evidences of cerebritis and acute infarction on radiological findings in 3 cases who presented as a stroke. In 2 cases there were evidences of cerebritis and cavernous sinus thrombosis and in one case a cystic lesion in the frontal lobe suspicious of brain abscess was reported. Fungal abscess caused by mucormycosis was confirmed by histopathological findings (Fig. 4). According to radiological findings of nasosinusal CT before sinonasal surgery, there were a wide range of radiological evidences from mild mucosal thickening to mucosal necrosis and acute rhinosinusitis. Maxillary sinus involvement was the most common among paranasal sinuses (89.1%) (Fig. 5). During endoscopic sinus surgery in 67.4% of patients, black scar of mucosa and even bone was clearly observed. Of the 46 study cases, 17 (37%) died before discharge and the mean duration of admission in our study was 4 weeks. Amphotericin B/liposomal amphotericin B in combination with aggressive surgical debridement were used as the first-line treatment and continued with daily examination and debridement if necessary. Eight of our patients underwent exenteration surgery. There was no mortality before discharge between them. According to Chi-Square test, exenteration surgery significantly reduced mortality (P-value = 0.027). In this study, the presence of oral necrotic lesions significantly increased mortality (P-value = 0.036). There was no significant relationship between mortality rate and intracranial involvement and previous malignancy (P-value >0.05). Endoscopic images with necrotic hyphae are presented in (Fig. 6)
Orbital involvement, (A) Periorbital erythema and swelling, (B) Conjunctival chemosis, (C) Periorbital and lacrimal sac swelling, (D) Proptosis and fixed mydriatic pupill of right eye, (E) Left peripheral facial palsy. Written informed consent was obtained from the participant of the study.
Radiological findings of intracranial involvement, (A) T2-weighted magnetic resonance images (MRIs) of brain showing cerebritis and infarction (red arrow). (B) T2-weighted MRI of brain showing cavernous sinus thrombosis (red arrow). (C) Postcontrast T1-weighted MRI of brain showing mucormycosis cerebral abscess in frontal lobe. Proptosis and inflammation extending to the orbital apex effacing the right optic nerve can also be seen.
(A through C) Coronal computed tomography (CT) scans of paranasal sinus, (A and B) showing mild mucosal thickening (red arrow) and (C) air fluid level and air bubbles within fluid level (red arrow). (D) Axial CT scan of paranasal sinus showing mucosal necrosis of the left inferior turbinate (red arrow).
COVID-19 as a novel infectious disease is caused by SARS-COV-2 and is spreading rapidly around the world.1 The virus, due to developing cytokine storm and decreasing T cell counts, causes severe acute respiratory syndrome, and has so far led to more than 6 million deaths worldwide.14 In response to this disease, increase of antibiotic usage among COVID-19 patients in different countries has been noted.15 On the other hand, according to the existing guidelines, the use of systemic corticosteroids is still strongly recommended in the treatment of patients with severe COVID-19 continuing to be one of the main treatments.16 Excessive use of corticosteroids and antibiotics can change the normal flora. Steroids function mainly by causing defects in the function of macrophages and neutrophils thereby leading to immunosuppression. Barrier function of the nasal mucosa also modulated by the colonizing normal flora therefore excessive use of corticosteroids and antibiotics can eliminate the barrier against opportunistic fungal and bacterial infections.15 According to studies, the most common risk factor of mucormycosis is diabetes mellitus. India, with 62 million diabetic people, has reported an increase in mucormycosis cases during the COVID-19 pandemic.15,17–19 For example, Samir Joshi et al., in a similar study to ours, reported that there were 3–8 cases of mucormycosis from 2016 to 2020, but 160 cases of mucormycosis were diagnosed in their training hospital during one month in 2021.20 In our country, Avateffazeli et al., reported increase in the number of patients with COVID-19-associated rhino-orbital mucormycosis who were admitted to Kermanshah training hospital. In their study, from October 12 st, 2020 to November 18th, 2020, 12 patients suffering from COVID-19 associated-mucormycosis (CAM) were reported.21 Before the pandemic, Dolatabadi et al., through a cross-national research study conducted in collaboration with medical universities, studied the prevalence of mucormycosis in Iran from 2008 to 2014. In the aforementioned study, based on surgical biopsy and FNA, 208 cases of mucormycosis were reported from all over the country, most of whom were women (51%) with the mean age of 50 years. In their study, it was revealed that the prevalence of mucormycosis in the country increased from 20 cases in 2008 to 50 ones in 2013. The most common site of involvement was the paranasal sinuses (86%), followed by lungs, kidney, skin, and brain. Diabetes mellitus was the most common underlying disease (75%).22 Our study was conducted at an ENT subspecialty training department, Yazd, which serves as a referral center for cases with sinonasal mucormycosis in the center region of Iran. Yazd province ranks first in the country in terms of the prevalence of diabetes mellitus. In this regard, Mirzaei et al., showed that the prevalence of diabetes mellitus in this province was 14.1% in 2020.23 The present cross-sectional study was performed over two years from March 20, 2020 to March 20, 2022, which was during the COVID-19 pandemic. Based on the histopathological findings, 46 cases with definitive diagnosis of mucormycosis were included in the study. According to a study conducted before COVID-19 pandemic by Meybodian et al., at our department, there were 19 cases of sino-robital mucormycosis from 2017 to 2019.24 Based on these findings, with the onset of the pandemic, we have seen increase in the incidence of mucormycosis more than twice as much as before in our training department. In our study, age range was 5-82 years, mean age was 53 years and 52% of the patients were male. All patients had history of current or previous COVID-19 (100%). At the time of diagnosis, in only 28% of patients COVID-19 PCR test was positive and in most of them (72%) was negative. Diabetes mellitus was the most frequent disease (70%) after COVID-19. About 61% had history of corticosteroid usage (85% during COVID-19 treatment). Regarding frequency of 13% had malignancy, of which hematologic malignancy was the most frequent (83%). Samir Joshi et al., conducted a similar study in Pune, India. From March 1, 2020 to June 5, 2021, during 15 months. They reported 178 patients with mucormycosis who referred to their ENT training department, all of whom developed the disease after undergoing COVID-19 treatment.20 In their study, a much larger number of cases of mucormycosis were reported in less time than in our study (15 months vs. 24 months and 178 patients vs. 46 patients). Comparing the results reported by both studies, all patients had a history of COVID-19 and most patients were in the age group of 45–65 years. The prevalence of diabetes mellitus in patients in Samir Joshi's study was higher than ours (74.2% vs. 69.6%). In contrast, in our study, corticosteroid usage was higher (60.9% vs. 52.8%). In Samir Joshi's study, facial pain was the most common symptom (74%), but orbital involvement was more frequent in our patients (80.4%) as it was the decrease in visual acuity (71.7 vs. 37%). In our study, the interval between the diagnosis of COVID-19 and the onset of mucormycosis was 3.3 weeks and in Samir Joshi's study it was 28 days (4 weeks). Intracranial involvement was slightly more frequent in our study (13% vs 12%) the mortality rate of patients before discharge from hospital was more than twice (37 vs. 15%). In our study, orbital involvement was the most common clinical manifestation (80%), which was unilateral in all cases. In addition, periorbital pain and edema were the most common orbital involvement symptoms in our patients (78%). Pakdel et al., also examined 15 patients during six months of 2020. In their study, periorbital pain and edema as well as eyelid ptosis were the most common clinical signs. In the aforementioned study, 5 cases underwent exenterating surgery.25 In a study by Sharma et al., 23 cases of sinonasal mucormycosis were referred to their ENT department during four months of 2020, all of whom had history of COVID-19. In their study, diabetes mellitus was the most common underlying disease but only 43% of cases had orbital involvement, and none lost their vision or were exenterated.26 However, in our study, 72% of patients had visual impairment and 19 patients (41%) had lost unilateral eye vision completely, 17 of who were also frozen eye. Eight patients underwent unilateral exenteration surgery. Based on these findings, decreased visual acuity and NLP (No Light Perception) were more frequent in our patients. Another common symptom in our patients was hemifacial pain (78%) and hemifacial numbness (63%) also these symptoms were ipsilateral in all cases and in some cases led to long-term morbidity. Intracranial involvement was present in our 6 cases while in the study by Dolatabadi et al., the same number was reported in a period of 6 years before the pandemic.22 An interesting point in our study was the incidence of peripheral facial palsy in 12 cases (26%), which were all unilateral. In these 12 patients facial pain and numbness were presented on the same side. Decreased vision and ophthalmoplegia were also seen in 10 of them. Therefore, despite the involvement of multiple cranial nerves (II, III, IV, V, VI, VII) in these 10 patients, these findings could indicate the occurrence of a rare phenomenon called Garcin syndrome. Garcin syndrome is a rare clinical phenomenon involving multiple cranial nerves in the context of invasive mucormycosis. This syndrome usually occurs in immunocompromised patients and greatly increases mortality in these patients (42.85%). Symptoms occur step by step and progressively, involving at least 7 cranial nerves or sometimes the entire cranial nerve of one side without existence of intracranial space-occupying lesion. This syndrome is found in skull base tumors and is very rare in invasive rhinocerebral mucormycosis.27
ConclusionBased on the results of this study, during 2 years of the COVID -19 pandemic, there was increase in the incidence of sinonasal mucormycosis more than twice as much as before. Given that mucormycosis has a high mortality and morbidity rate and its complications can be prevented only through a strong clinical suspicion and early diagnosis, it seems that physicians need to be aware of the high risk of developing mucormycosis in COVD-19 patients with diabetes mellitus, even after recovery from COVID-19. An interesting point in our study was the incidence of Garcin's syndrome. Due to the fact that this syndrome greatly increases mortality in these patients, clinical suspicion of this syndrome is also necessary for early diagnosis.
Compliance with ethical standardsStudy protocol was in accordance with the latest Declaration of Helsinki for medical research involving human subjects and was approved by the local ethics committee.
This article does not contain any studies with animals performed by any of the authors.
Informed consent was obtained from all participants of the study.
Conflict of interestAuthors have no conflicts of interest.