The main aim of the study was to establish the oncological safety of the laparoscopic approach to radical cystectomy for high-risk, non-organ-confined urothelial tumours.
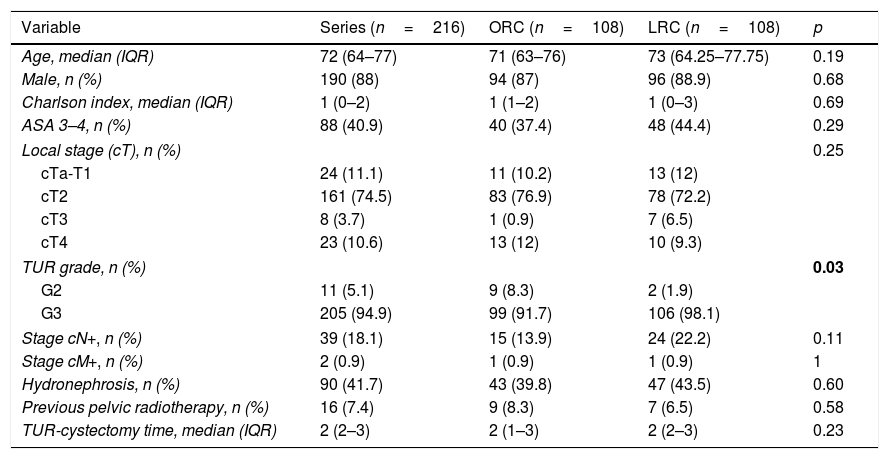
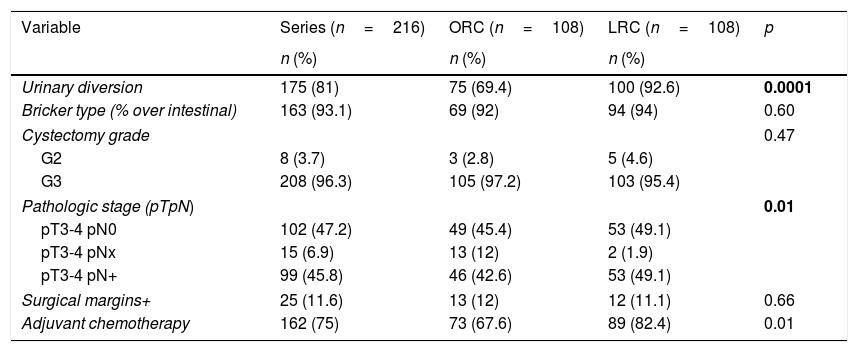
Material and methodsA retrospective cohort study of 216 stage pT3-4 cystectomies operated between 2003 and 2016; using an open approach (ORC, n=108), and using a laparoscopic approach (LRC, n=108).
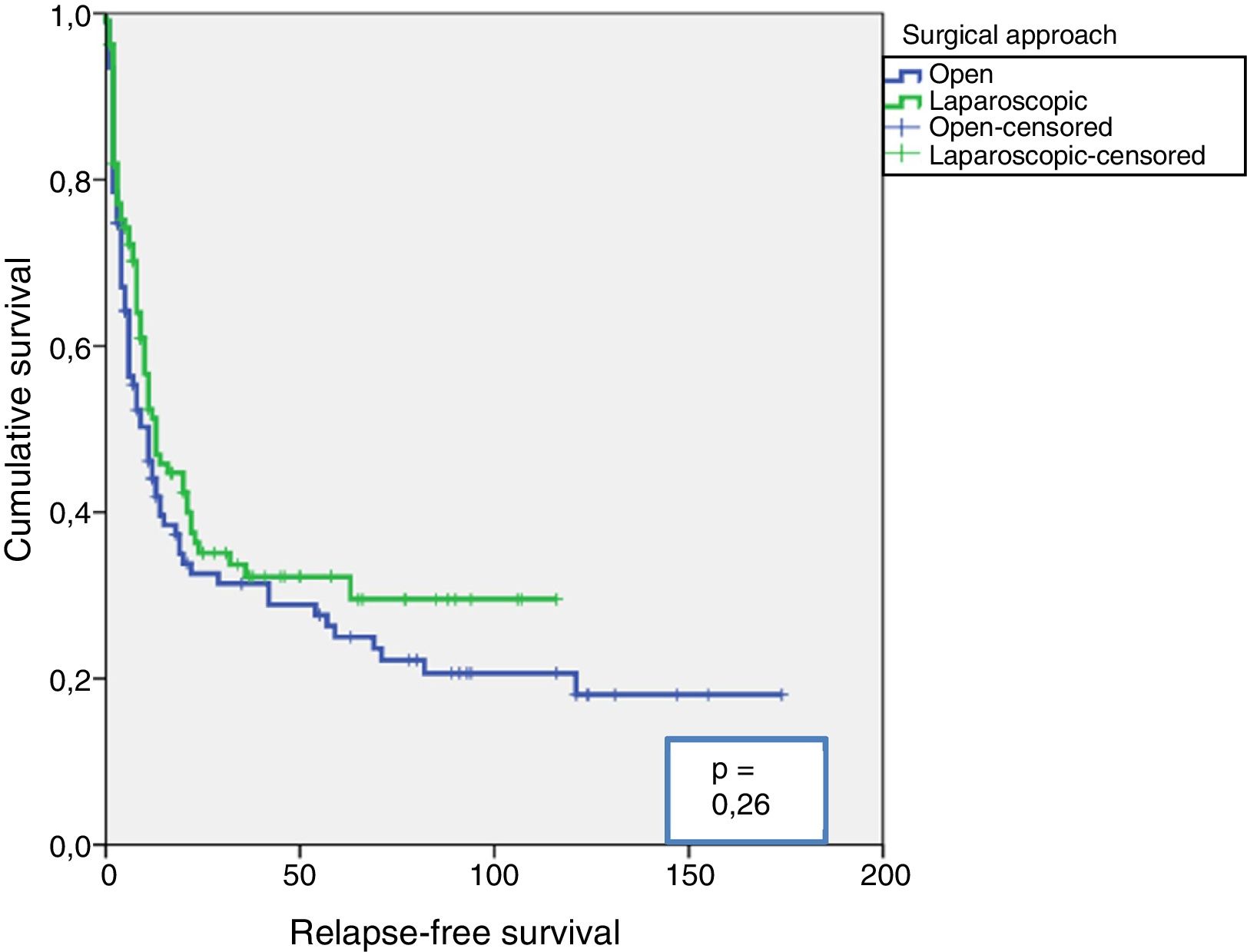
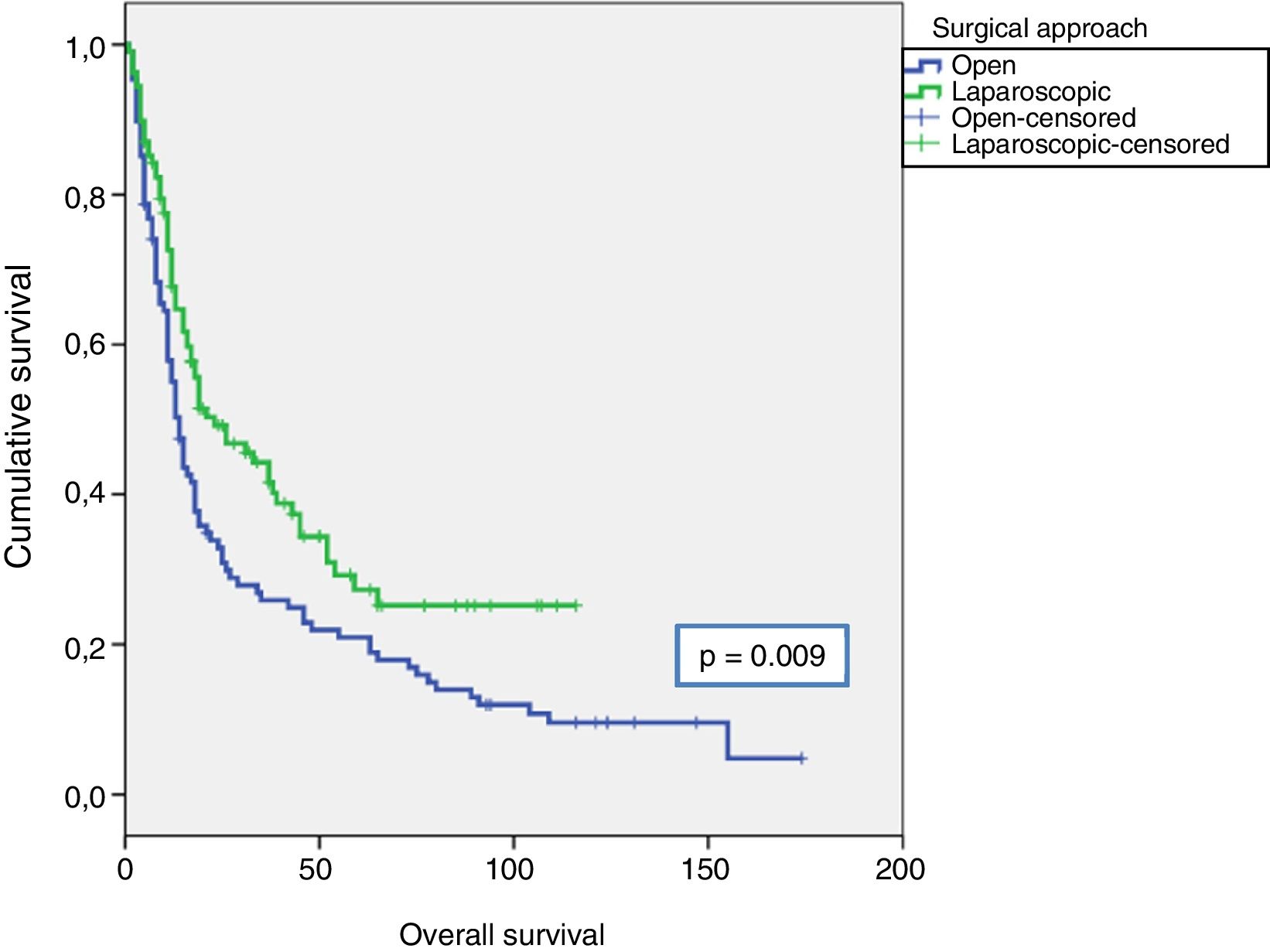
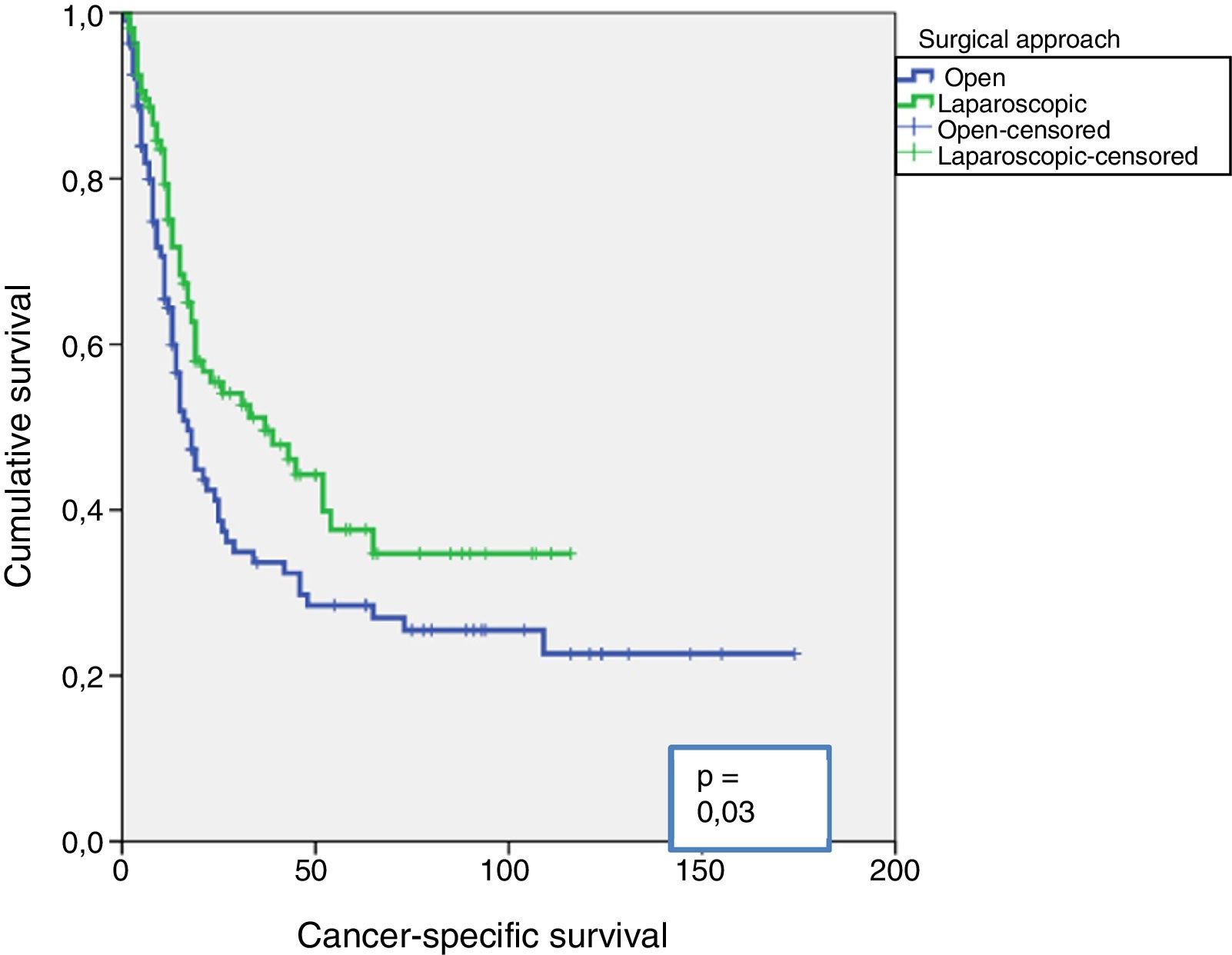
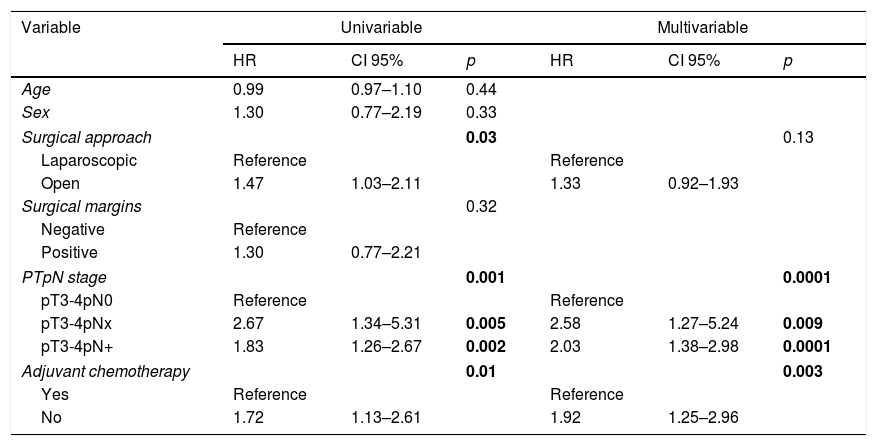
ResultsBoth groups have similar pathological features except, in G3 TUR, there were more lyphadenectomies and greater pN+, and more adjuvant chemotherapies using the LRC. The median follow-up of the series was 15 (IQR: 8–10.5) months. Sixty-eight point one percent of the series relapsed, with no differences between either group (p=0.11). The estimated differences for cancer-specific survival was greater in the LRC group (p=0.03), as was overall survival (p=0.009). There were no differences between either group in estimated recurrence-free survival (p=0.26). The type of surgical approach (p=0.03), pTpN stage (p=0.0001), and administration of adjuvant chemotherapy (p=0.003) were related to cancer-specific mortality (CSM) in the univariate analysis. Only the pTpN stage (p=0.0001), and not giving adjuvant chemotherapy (p=0.003) behaved as independent predictive factors of CSM.
ConclusionThe type of surgical approach to cystectomy (ORC vs. LRC) did not influence CSM. Lymph node involvement and not giving adjuvant chemotherapy were identified as predictive factors of CSM. Our study supports the oncological safety of the laparascopic approach for cystectomy in patients with locally advanced muscle-invasive bladder tumours.
El principal objetivo del estudio fue establecer la seguridad oncológica del abordaje laparoscópico en la cistectomía radical de tumores uroteliales de alto riesgo no órgano-confinados.
Material y métodosEstudio de cohortes retrospectivo de 216 cistectomías estadio patológico pT3-4 intervenidos entre 2003 y 2016; con acceso abierto (CRA, n=108) y laparoscópico (CRL, n=108).
ResultadosAmbos grupos tuvieron similares características patológicas, excepto en grado G3 de la RTU, mayor número de linfadenectomías y con mayor pN+, y mayor número de quimioterapia adyuvante en el grupo de CRL. La mediana de seguimiento de la serie fue de 15 (IQR: 8-10,5) meses. Recidivó el 68,1% de la serie, sin diferencias entre ambos grupos (p=0,11). La estimación de las diferencias para la supervivencia cáncer específica fue mayor en el grupo de CRL (p=0,03), al igual que la supervivencia global (p=0,009). No existieron diferencias entre ambos grupos en estimación de supervivencia libre de recidiva (p=0,26). El tipo de acceso quirúrgico (p=0,03), el estadio pTpN (p=0,0001) y la administración de quimioterapia adyuvante (p=0,003) se relacionaron con la mortalidad cáncer específica (MCE) en el análisis univariante. Solo el estadio pTpN (p=0,0001) y la no administración de quimioterapia adyuvante (p=0,003) se comportaron como factores predictores independientes de MCE.
ConclusiónEl tipo de acceso quirúrgico a la cistectomía (CRA vs. CRL) no influyó en la MCE. La afectación ganglionar y la ausencia de quimioterapia adyuvante se identificaron como factores predictores de MCE. Nuestro estudio avala la seguridad oncológica del abordaje laparoscópico de la cistectomía en los pacientes con tumores vesicales musculoinvasivos localmente avanzados.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora