The COVID-19 pandemic has brought about changes in the management of urology patients, especially those with prostate cancer.
The aim of this work is to show the changes in the ambulatory care practices by individualized telematic care for each patient profile.
Materials and methodsArticles published from March 2020 to January 2021 were reviewed. We selected those that provided the highest levels of evidence regarding risk in different aspects: screening, diagnosis, treatment and follow-up of prostate cancer.
ResultsWe developed a classification system based on priorities, at different stages of the disease (screening, diagnosis, treatment and follow-up) to which the type of care given, in-person or telephone visits, was adapted. We established 4 options, as follows: in priority A or low, care will be given by telephone in all cases; in priority B or intermediate, if patients are considered subsidiary of an in-person visit after telephone consultation, they will be scheduled within 3 months; in priority C or high, patients will be seen in person within a margin from 1 to 3 months and in priority D or very high, patients must always be seen in person within a margin of up to 48 h and considered very preferential.
ConclusionsTelematic care in prostate cancer offers an opportunity to develop new performance and follow-up protocols, which should be thoroughly analyzed in future studies, in order to create a safe environment and guarantee oncologic outcomes for patients.
La pandemia por COVID-19 ha supuesto un cambio en la atención a pacientes en el ámbito urológico, especialmente con cáncer de próstata.
El objetivo de este trabajo es mostrar los cambios en el manejo a nivel ambulatorio individualizando para cada perfil de paciente la atención telemática.
Materiales y métodosSe han revisado artículos publicados desde marzo del 2020 hasta enero del 2021. Se han seleccionado aquellos que aportaban los mayores niveles de evidencia en cuanto al riesgo en distintos aspectos: cribado, diagnóstico, tratamiento y seguimiento del cáncer de próstata.
ResultadosDesarrollamos una clasificación según prioridades, en diferentes etapas de la enfermedad (cribado, diagnóstico, tratamiento y seguimiento) adaptando a esta el tipo de control: presencial o telefónico. Establecemos 4 opciones: prioridad A o baja, en la que la atención será telefónica en todos los casos; prioridad B o intermedia, en la que si el paciente valorado telefónicamente se considera subsidiario de visita presencial, esta se citará dentro de los 3 meses posteriores; prioridad C o alta, el paciente será visto presencial con un margen para la visita de 1 a 3 meses, y prioridad D o muy alta, la visita deberá ser siempre presencial con un margen de hasta 48 h y considerada muy preferente.
ConclusionesLa atención telemática en cáncer de próstata representa una oportunidad para desarrollar nuevos protocolos de actuación y seguimiento que deberán ser analizados exhaustivamente en futuros trabajos con el fin de conformar un entorno seguro y garantizar resultados oncológicos para los pacientes.
The COVID-19 pandemic (disease caused by coronavirus in the year 2019) has brought about changes in the approach to urological care in general, and particularly, regarding oncology patients. The alarm generated, and the need to protect the population and health care workers from exposure to the virus has changed the conception of care we had until now regarding surgical and ambulatory care settings.
Concerning diagnosis, treatment and follow-up care planning, prostate cancer (PC) allows a time-frame which facilitates the design of an oncologically safe roadmap based on screening and priority selection.
The work in urologic oncology units such as ours is based on a specific outpatient clinic that provides comprehensive care to PC patients. The multidisciplinary approach turns individualized care into a transversal, more comprehensive care, in which patients are evaluated by different specialties according to their own needs. And, in the same way as surgical treatments have had to adapt during the pandemic, face to face care (consultations) has also gone through changes.
The World Health Organization declared that the outbreak caused by the new coronavirus (SARS-CoV-2 or severe acute respiratory syndrome caused by coronavirus type 2) constituted a Public Health Emergency of International Concern (PHEIC) on January 30, 2020. On February 11, 2020, it designated the disease caused by the virus as COVID-19 and declared a global pandemic situation on March 11, 2020.
SARS-CoV-2 has a very high transmission and infection capacity, manifesting as pneumonia that can cause severe respiratory problems that require, in some cases, assisted ventilation and intensive care. Overloaded hospitals, the social alarm and the need to protect the most vulnerable groups have changed the practice patterns within urology units.
Healthcare institutions have been occupied either entirely or partially by patients with SARS-CoV-2, which has made it impossible to maintain regular health care, resulting in delayed consultations, tests, diagnoses and treatments. Treatment for PC has been the main focal point in this pandemic. However, a survey-based research carried out to examine the global impact of COVID-19 on urological care showed a delay of more than 8 weeks reported in 28% of consultations, 30% of ambulatory procedures and 31% of urological surgeries.1 This has radically affected patient care. The impact of these changes has determined the need for adaptation almost on a daily basis and has resulted in the development of new guidelines. Prioritization protocols, mainly surgical, have been created, and telematic care has been implemented,2–4 although there are few publications in this regard. We have not found heterogenous protocols in the literature reviewed, therefore we have developed our own recommendations for the management of patients with PC.
The aim of this study is to expose the impact of the SARS-CoV-2 pandemic on the management of patients with PC and to determine the best adaptation possible, individualized for each patient profile, especially in the ambulatory setting, a scenario in which telephone clinics have acquired a relevant role.
Evidence acquisitionArticles published in Spanish and English language journals from March 2020 to January 2021 were reviewed. We selected those that provided the highest levels of evidence regarding risk in each field: screening, diagnosis, treatment and follow-up of PC.
Evidence synthesisIn relation to the initial diagnosis of PC, Bakouny et al.5 analyzed the potential impact of delayed screening and diagnosis on patients in the oncology setting. The authors report significantly reduced screening tests and number of PC diagnoses during the pandemic period. The percentage of PSA positivity appeared to be higher during the pandemic period compared to the control periods (preceding 3 months and same period of the previous year), 22.7% vs. 9.9–13.2%, which may reflect prioritization of patients with high suspicion of PC. However, the percentage reductions in diagnoses compared to controls were also significant, ranging from −60 to −82%, according to the tests analyzed in different oncology settings, not only regarding PC.
Percentage reductions in diagnoses resulting from cancer screening tests were also evident (−19% to −78%). They conclude that if the same number of patients had been screened during the pandemic period as in the previous 3 months, approximately 1,438 suspected diagnoses would not have been missed during the first 3 months of the pandemic period. Along the same lines, an analysis by de Vincentiis et al. evaluates cancer diagnosis rates during the pandemic period, finding that these fell in 2020 by 39% compared with the average number recorded in 2018 and 2019. Prostate cancer had a decrease of 75%, although the study highlights that the decrease of high-risk diagnoses (ISUP 4–5) was irrelevant, emphasizing that the delay had more impact on low- and intermediate-risk cancer.6
In terms of PC, the consequences do not seem to be as major when compared to other urologic cancers. However, precise data on the impact of delayed radical prostatectomy (RP) on progression and mortality remains unknown.
There is no clear consensus on the individualization of the decision to perform prostate biopsy (PBx). The European Society of Urology (EAU)7 recommends delaying PBx, with its performance before 3 months only in cases with PSA ≥ 10 ng/mL or abnormal digital rectal examination (DRE) without magnetic resonance. PBx would be indicated with a higher priority only in cases of locally advanced or symptomatic disease. If there are symptoms of metastasis, staging imaging tests should be performed with high priority, and androgen deprivation therapy (ADT) should be recommended if there is evidence of metastatic spread. In these cases, biopsy could be postponed. In active surveillance (AS), confirmatory biopsy can be delayed for up to 6 months and PSA monitoring for a maximum of 6 months. For its part, the Urological Society of Australia and New Zealand (USANZ) advocates that the PIRADS 4/5 classification should be handled according to standard practice.8
A Spanish multicenter study has drawn up a series of recommendations on the management of PC, including screening and treatment, using a color code and categories: emergency, urgent, urgent elective, elective and deferrable.9 Obek et al. make recommendations with relation to early detection, advocating its delay until the end of the pandemic period if the patient is asymptomatic, since a delay of 6–12 months should not have any negative impact on most PCs. PBx should only be considered in patients with PSA > 10−20 ng/mL and abnormal DRE. Concerning the indication for initiation of systemic therapy, in case of metastases, they recommend postponing biopsy and start ADT.10
Regarding the scope of treatment, a retrospective study on 513 patients by Meunier et al. based on the risk of biochemical recurrence (BCR) determines that there appears to be no time threshold for treating patients with tumors of Gleason score (GS) 6, this would be 90 days for GS 7 and 60 days for GS ≥ 8.11 Gravas et al., evaluating the clinical practice adapted to the pandemic, ratify this by analyzing the level of adaptation to guidelines, finding that RP is the oncologic intervention that received the lowest priority except only for high risk, with a score between 4 and 5, with 1 being the lowest priority and 10 the highest.12
The underlying idea is that postponing treatments for low- and intermediate-risk PC could be safe, considering the likely low clinical impact that this entails. However, there is more controversy regarding high-risk disease.8
Authors such as Ficarra et al. categorize surgeries according to priority, in the following way:
- ‐
Non-deferrable surgeries, in which a delay could seriously affect oncologic outcomes. This would be the case of high-risk or locally advanced PC patients who are not receiving radiotherapy (RT).
- ‐
Semi-non-deferrable surgeries depending on the level of COVID-19 diffusion in each region. This category includes patients with intermediate-risk disease.
- ‐
Deferrable surgeries or those that can be replaced by other treatments.
The authors’ main recommendation is to perform RP only in high-risk, locally advanced patients and in patients who are not suitable for RT. Regarding PBx, their recommendation is to postpone it, except in cases with a high clinical suspicion if the COVID-19 emergency phase is prolonged in time.13
Stensland et al. suggest postponing most RPs, including high-risk, given the existence of other options such as RT.14 A delay even longer than 12 months should not alter follow-up and cancer-specific mortality. Fossati et al. in their study regarding the impact of time between PC diagnosis and RP on cancer control, reviewed 2,653 patients treated by RP. They found that 283 experienced BCR and 84 experienced clinical recurrence (CR). Patients at higher risk had higher rates of BCR and CR after 12 months of delayed surgical treatment. They report that, at high risk, waiting time was significantly associated with both factors, although clinical significance was most apparent after 12 months.15
The EAU categorizes different priorities according to a color code7:
- -
Low priority (green color): when clinical harm (understood as progression, metastasis or loss of function) is very unlikely if treatment is postponed for 6 months.
- -
Intermediate priority (yellow color): can be cancelled but should be reconsidered in the case of increased care capacity, given the probable clinical harm if postponed for 3–4 months.
- -
High priority (red color): the last to cancel. Avoid a delay of more than 6 weeks due to probable clinical harm if postponed longer.
- -
Emergency: cannot be postponed for more than 24 h due to life threatening condition.
Therefore, regarding RP, it is only recommended in locally advanced tumors, including lymph node involvement. The use of ADT plus RT is considered as an alternative to surgery and neoadjuvant therapy (NAT) in symptomatic patients, plus RT 6–12 months later. Ginsburg et al. state that delays of up to 12 months will not have worse oncologic outcomes (adverse pathology, staging or secondary treatment) for intermediate and high risk PC.16
According to Obek et al., surgery could be delayed for up to 6–12 months in unfavorable intermediate risk without administering neoadjuvant ADT.10 However, in high risk, it is recommended not to delay it for more than 6 months, and RT is the best option. In case of nodal involvement, treatment is required within 6 weeks after diagnosis, with ADT plus RT being the best option.17 Kutikov et al. recommend that high risk should be treated immediately, although they categorize by age.18
Regarding metastatic hormone-sensitive PC (mHSPC+) and metastatic castration-resistant PC (mCRPC+), the EAU, in addition to other authors, recommends offering immediate treatment with abiraterone, apalutamide or enzalutamide, avoiding the use of chemotherapy7 as much as possible, emphasizing that face-to-face visits should always be considered in cases of newly diagnosed advanced PC (node+, M+).17
In this situation, prescribing neoadjuvant ADT is a feasible option. Patients treated by NA ADT had better pathological outcomes after RP.19 CT2 tumors showed lower local recurrence figures, in T3, although there were lower rates of positive margins, the use of NA did not determine lower rates of PSA progression. However, patients who received more than 3 months of NA had a lower risk of BCR at 5 years compared to surgery alone,20 survival benefits remain unknown. Some papers advocate preferential care for high-risk patients considering the use of NAT21 on the basis that the NAT group has a lower pathologic T stage, lower likelihood of seminal vesicle invasion, positive lymph nodes or positive surgical margins.22
While surgical prioritization seems safe, this cannot be applied to the transition of PC patients to telemedicine consultations. Are all patients suitable for telephone visits? or, in other words, are face-to-face evaluations always necessary? How should we make this selection?
After a study carried out in the Montefiore urology department, a decision was made to convert all office visits to telephone visits, both for previously scheduled and new patients. From the beginning of this transition, in-office face-to-face visits were dramatically reduced to fewer than 5% of the total volume, reserved only for those patients requiring urgent in-office evaluation. Telematic visits are seen as an opportunity to reconsider the way in which health care has been delivered so far and on how it should evolve in the future.23
Telemedicine is not a new practice in the medical environment, although the literature in terms of urology is scarce.24 It is a useful model of care for remote populations and workforce shortages.25 It allows care to be delivered without exposing patients or staff to infection, reducing unnecessary hospital visits and limiting the number of people in waiting rooms, which is essential to avoid viral transmission.26 The importance of these preventive measures becomes even higher if we take into account the mean age of our patients27 and the fact that up to 94.5% of them may have one or more risk factors for SARS-CoV-2 infection.
Novara et al.24 carried out a review of 45 articles regarding telemedicine and urology (11 of them on PC) observing the success of telemedicine implementation, showing it to be, at least, non-inferior to face-to-face consultation. However, current evidence is scarce due to the heterogeneity of the data and the fact that it is limited to specific groups of patients.
DiscussionThe implementation of telemedicine may seem tedious and entail issues related to reimbursement and coverage in sectors such as private medicine.29 However, this process was relatively simple in our setting, despite the lack of previous experience. It was necessary to allow remote access to the health service intranet, which had been limited to health centers until then. The use of electronic prescriptions was generalized, and staff members were supplied with cell phones. Webcams were installed to allow multidisciplinary sessions and communication across services. The principle of confidentiality and data protection was always applied, and appropriate platforms were used. Privacy was a relevant aspect, and adequate transmission and reception of information was ensured.26
Despite the clear benefits of telemedicine, its rapid implementation in an imperative and generalized manner may initially lead to its rejection. However, several studies have shown high satisfaction with virtual consultations, without finding differences between patients with oncologic diagnoses and those with benign diseases,30 in some cases even preferring them to face-to-face consultations. Nevertheless, patients pointed out the structuring of the consultation and technological barriers as the main points for improvement.31,32
It is essential that professionals receive education in telematic consultation.33 Rodriguez Socarras et al.26 provide a comprehensive guide to safe consultation. They stress the need to maintain the same level of professionalism as in face-to-face consultations so as not to deteriorate the doctor-patient relationship based on trust. In case of doubts about the patient’s understanding, a second visit should be scheduled in the near future.34 Prasad et al.28 designed a set of guidelines and developed a patient handout to improve the effectiveness of telephone consultations. The design of appropriate privacy-compliant platforms must also be implemented35 and, although urgent short-term solutions have been provided by the various healthcare systems, patient privacy and cybersecurity issues need to be defined and regulated from this moment on.36 In addition, in the long term, the quality, safety and efficacy of telemedicine will need to be evaluated.
On the other hand, we should not forget the psychological impact that the vast majority of professionals acknowledge after assisting patients with COVID-19, which is more intense in front-line personnel.37 This, in addition to burnout syndrome, is highly prevalent among physicians.38 For all these reasons, we must remember the need for protective measures and psychological support for our professionals, even in the face of apparent mild symptoms.
The necessary adaptive changes in our urology field have required the development of different strategies to optimize in-office care, including screening by “direct triage” or the classification of patients before their arrival to the doctor’s office. In our unit, we screened all patients scheduled in the PC consultation to determine who was eligible for a telemedicine visit. This was developed during the first months of the pandemic period by the 4 urologists in charge of the unit, together with a case manager who is, to our understanding, an essential part of the development of this work. The professional in charge of this task must have extensive experience in the management of information related to PC, as well as in the administration of patient agendas. The aim was to minimize exposure by coordinating the essential medical tests, thus reducing the need for risky situations (hospital visits, overcrowded waiting rooms, etc.).39
Analyses carried out by other authors in this scenario agree that most urology consultations should be in the way of telemedicine visits or be postponed during the pandemic period. If the slogan is to keep patients safe at home, we must manage a series of guidelines that allow us to do this with providing appropriate care that guarantees solutions for cancer patients. We must be cautious and apply all the knowledge collected in similar studies, taking into account the resources available and, undoubtedly, the capacity of each patient to cope with this type of care.40
The review carried out and our own experience have allowed us to develop a classification to differentiate patient care in consultation. Telematic care has been a growing approach since the beginning of the pandemic period. Screening of all consultations to determine which patients required in-person visits and which should be attended telematically, has been the basis of this work.
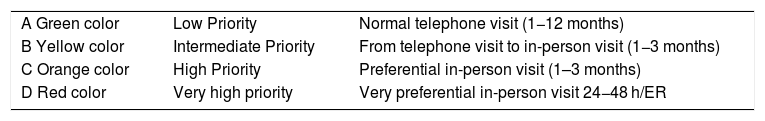
Initially, and due to the situation, telephone visits were given the highest priority, although consultations have been adapted to the characteristics of each patient and the profile of the disease. Finally, we have developed a classification of priorities in the different stages of PC (screening, diagnosis, treatment and follow-up) taking into account all aspects of the disease and, consequently, the telephone or face-to-face check-ups required have been adapted to this. Therefore, we have introduced a new element, the telephone consultation. We have established 4 priorities that are associated with different colors for better understanding, as follows (Tables 1 and 2):
- ‐
Priority A or low (green color), the consultation will be by telephone in all cases with margins for follow-up visits of 1–12 months.
- ‐
Priority B or intermediate (yellow color) when the patient is considered eligible for face-to-face visits after telephone consultations. This visit will be scheduled within the following 3 months.
- ‐
Priority C or high (orange color) the patient will be seen in person within a time frame of 1–3 months.
- ‐
Priority D or very high (red color), the visit should always be face-to-face within a time frame of up to 48 h and is considered highly preferential.
Color-coded priorities.
| A Green color | Low Priority | Normal telephone visit (1−12 months) |
| B Yellow color | Intermediate Priority | From telephone visit to in-person visit (1−3 months) |
| C Orange color | High Priority | Preferential in-person visit (1–3 months) |
| D Red color | Very high priority | Very preferential in-person visit 24−48 h/ER |
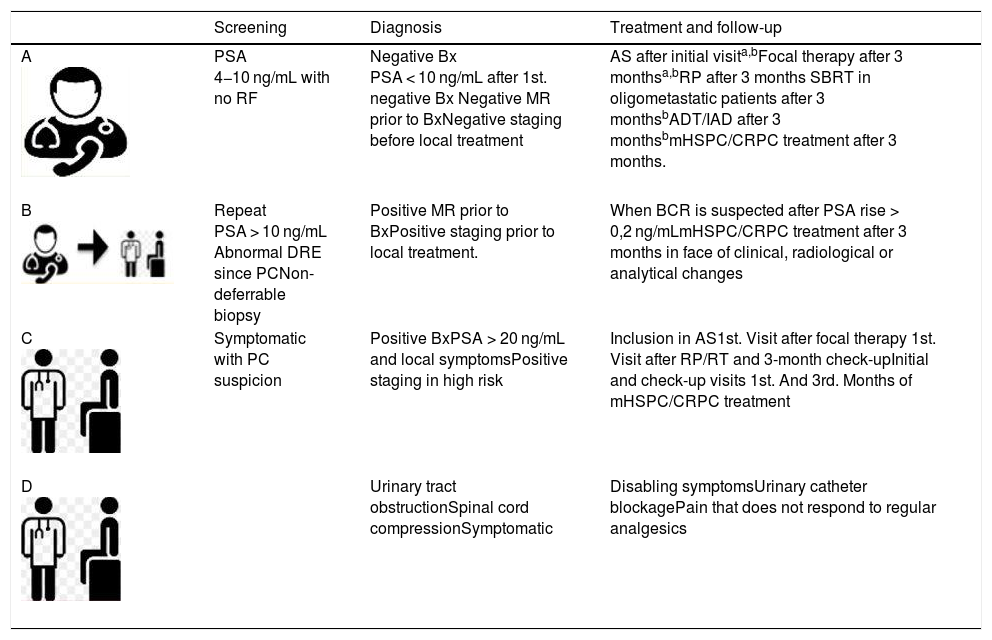
Consultation priority according to PC stage.
| Screening | Diagnosis | Treatment and follow-up | |
|---|---|---|---|
| A | PSA 4−10 ng/mL with no RF | Negative Bx PSA < 10 ng/mL after 1st. negative Bx Negative MR prior to BxNegative staging before local treatment | AS after initial visita,bFocal therapy after 3 monthsa,bRP after 3 months SBRT in oligometastatic patients after 3 monthsbADT/IAD after 3 monthsbmHSPC/CRPC treatment after 3 months. |
| B | Repeat PSA > 10 ng/mL Abnormal DRE since PCNon-deferrable biopsy | Positive MR prior to BxPositive staging prior to local treatment. | When BCR is suspected after PSA rise > 0,2 ng/mLmHSPC/CRPC treatment after 3 months in face of clinical, radiological or analytical changes |
| C | Symptomatic with PC suspicion | Positive BxPSA > 20 ng/mL and local symptomsPositive staging in high risk | Inclusion in AS1st. Visit after focal therapy 1st. Visit after RP/RT and 3-month check-upInitial and check-up visits 1st. And 3rd. Months of mHSPC/CRPC treatment |
| D | Urinary tract obstructionSpinal cord compressionSymptomatic | Disabling symptomsUrinary catheter blockagePain that does not respond to regular analgesics |
PC: primary care; Bx: biopsy; PC: prostate cancer; mHSPC: metastatic hormone-sensitive prostate cancer; CRPC: castration-resistant prostate cancer; RF: risk factors; IAD: intermittent androgen deprivation; RP: radical prostatectomy; BCR: biochemical recurrence; pMR: prostate magnetic resonance; RT: radiotherapy; SBRT: stereotactic body radiotherapy; BC: bladder catheter; ADT: androgen deprivation therapy; DRE: digital rectal examination; AS: active surveillance.
In short, while the COVID-19 pandemic has forced the restriction of face-to-face consultation in various aspects of medical practice, it has opened the door to the implementation of telephone consultations. In this work, we have aimed to bring together the knowledge collected with our own experience in the management of PC, adapted to the current context. The management of prostate cancer, as has been demonstrated, offers us adequate room for maneuver with oncologic safety. In addition, the total number of outpatient consultations has not decreased considerably, with an 80% maintained during the pandemic period in our setting (our own unpublished data). Hence, our proposal for a rationalization program, in which telematic care is introduced, and which allows evaluations adapted to new advances in the disease and to the corresponding healthcare characteristics.
ConclusionThe lessons learnt during the SARS-CoV-2 pandemic will undoubtedly change the management of cancer patients. These changes should be built on the analysis and knowledge of the evolution and response to PC treatments. We believe that the figure of a case manager, who previously reviews the results of the different tests, in the way of an initial filter, is essential in this aspect. Telematic care represents an opportunity to develop new guidelines that should be thoroughly analyzed in future work, with the aim of creating a safe environment and guaranteeing results for these patients.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García Rodríguez J, González Ruiz de León C, Sacristán González R, Méndez Ramírez S, Modrego Ulecia L, Fernández-Gómez JM. Cambios en el manejo ambulatorio de pacientes con cáncer de próstata durante la pandemia por SARS-CoV-2. Revisión bibliográfica y aporte de nuestro grupo en atención telemática. Actas Urol Esp. 2021;45:530–536.