Microperc is the upgraded form of percutaneous nephrolithotomy miniaturization. The aim of this study is to compare prospectively microperc and retrograde intrarenal surgery for the treatment of renal stones smaller than 2cm.
Material and methodsA comparative prospective study of both techniques was carried out between January 2014 and June 2015. Thirty-five patients were divided in two groups: Group A, 17 patients treated by retrograde intrarenal surgery and Group B, 18 patients treated by microperc. Stone clearance was assessed using CT scan 3 months after surgery.
ResultsBoth groups were statistically comparable as demographic variables and stone size was similar (16.76mm Group A vs 15.72mm Group B). Success rate, hospital stay and JJ stenting were similar for both groups. There was no statistically significant difference regarding post-operatory complications: 17.64% Group A vs 5.56% Group B (p=0.062), all of them Clavien I and II. Surgical time was statistically different (63.82min Group A vs 103.24min Group B) as well as hemoglobin drop (0.62g/dl Group A and 1.89g/dl Group B).
ConclusionMicroperc is an effective and safe procedure for the treatment of renal lithiasis smaller than 2cm, which makes it a good alternative to retrograde intrarenal surgery for this stone size. However, more prospective studies that include a larger cohort are necessary to confirm our results.
Microperc es el culmen de la miniaturización de la nefrolitectomía percutánea. El objetivo de nuestro trabajo es comparar prospectivamente microperc y cirugía retrógrada intrarrenal para el tratamiento de la litiasis renal menor de 2cm.
Material y métodosRealizamos un estudio comparativo prospectivo entre ambas técnicas, entre enero de 2014 a junio 2015, sobre 35 pacientes que fueron divididos en 2 grupos: grupo A, 17 pacientes tratados mediante cirugía retrógrada intrarrenal y grupo B, 18 pacientes tratados mediante microperc. La tasa de éxito se estableció mediante TC a los 3 meses de la intervención.
ResultadosAmbos grupos resultaron estadísticamente comparables gracias a la ausencia de diferencia tanto en variables demográficas como en el tamaño litiásico (16,76mm grupo A y 15,72mm grupo B). La tasa de éxito, la estancia hospitalaria y el tiempo de cateterismo posquirúrgico fueron similares para ambos grupos. Las complicaciones posquirúrgicas no alcanzaron diferencia estadísticamente significativa: 17,64% grupo A y 5,56% grupo B (p=0,062), todas ellas Clavien I y II. El tiempo quirúrgico sí alcanzó diferencia estadísticamente significativa (63,82min grupo A y 103,24min grupo B), así como la caída de hemoglobina (0,62g/dl grupo A y 1,89g/dl grupo B).
ConclusiónMicroperc es un procedimiento eficaz y seguro para el tratamiento de la litiasis renal inferior a los 2cm, pudiendo considerarse como alternativa a la cirugía retrógrada intrarrenal en este rango litiásico. Son necesarios más estudios prospectivos con un tamaño muestral mayor para confirmar nuestros resultados.
In the last decade, endourological techniques to treat renal lithiasis have evolved substantially. Retrograde intrarenal surgery (RIRS) has expanded its indications thanks to technological improvements that have increased its maneuverability by reducing its caliber and optimizing its vision. In addition, the evolution in the holmium laser has enabled to treat larger lithiasic sizes reducing the operative time. This development has made RIRS a well-established, widely accepted technique, offering a high success rate while maintaining a minimally invasive profile.1–4
On the other hand, the reduction of the caliber of percutaneous nephrolitectomy (PNL), which allowed the mini-PNL (miniperc) to reduce complications,5 has continued to progress toward minimum calibers. The micro-PNL (microperc) is the culmination of this process of miniaturization of percutaneous surgery. The pioneering series of Desay,6 published in 2011, has been followed by many more, not only in the adult patient but also in the pediatric patient, reporting high success rates without significant complications.7–13 These results make this technique another treatment option for small and medium-size stones,14 entering into clear competition with RIRS.
To our knowledge, there are only 2 studies in the literature that prospectively compare RIRS and microperc in the adult population,15,16 which is why we need a greater number of studies to know what place the microperc occupies within the therapeutic arsenal of lithiasis. The objective of our study is to prospectively compare both techniques in the treatment of renal lithiasis smaller than 2cm, analyzing their results and morbidity.
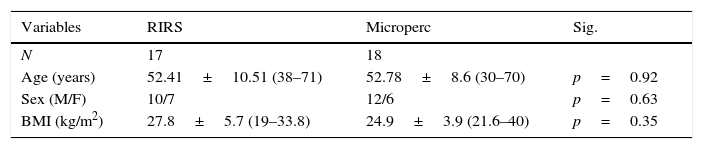
Material and methodsWe performed a prospective comparative study between 2 series of patients with single renal stones smaller than or equal to 2cm, operated consecutively between January 2014 and June 2015, using RIRS (group A) and microperc (group B). From a total of 35 patients, 17 cases (10 males and 7 females, with a mean age of 52.41±10.51) were consecutively assigned to RIRS (group A) and the following 18 (12 men and 6 women, with a mean age of 52.78±8.6) to microperc (group B).
For surgical planning and measurement of lithiasis size, a non-contrast CT scan was performed in all cases. In addition, pre-intervention urine cultures were obtained in all patients, and preoperative prophylaxis was performed with the same therapeutic regimen. Success in both groups was defined as the absence of significant remnants greater than 2mm after 3 months of CT intervention.
Both techniques were performed under general anesthesia. In all cases of RIRS, a ureteral access sheath of less than 14Fr (Navigator®-Boston Scientific, Natick, MA and Flexor Parallel®-Cook urological, Bloomington, IN) and digital flexible or optic fiber ureteroscopes (Flex XC® and Flex X2®-Storz, KARL STORZ, Tuttlingen, Germany). For lito-fragmentation, a double-pulse 30W holmium laser (Odyssey®-Cook urological, Bloomington, IN) was used with 200 and 273μm fibers. A nitinol basket (NGage®-Cook urological, Bloomington, IN) was used for the removal of fragments. In all patients operated on by microperc, supine position, radiologically and radiographically guided puncture, 4.85Fr sheath, 8F ureteral catheter and the same laser were used to reduce intrarenal pressure. In both techniques, an irrigation pump with manual perfusion control and double J or ureteral catheter were used at the end of the procedure.
To collect the data, a database was created in the Excel program. The data were analyzed using the statistical software SPSS v.15.0 (SPSS Inc., 1989–2006). The normality of the quantitative variables was established with the Kolmogorov–Smirnov test. To study the association between qualitative variables, the Chi square test was used with Fisher's exact test or likelihood ratio, depending on the application conditions. Student's ‘t’-test or Mann–Whitney U test were used to study the differences between means. The significance level for all tests was considered for a p≤0.05.
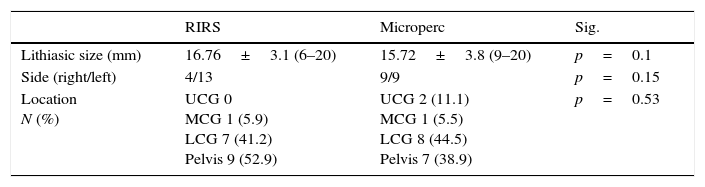
ResultsBoth groups were statistically comparable, both in the lithiasic size and in the demographic variables (Tables 1 and 2).
Characteristics of the lithiases.
| RIRS | Microperc | Sig. | |
|---|---|---|---|
| Lithiasic size (mm) | 16.76±3.1 (6–20) | 15.72±3.8 (9–20) | p=0.1 |
| Side (right/left) | 4/13 | 9/9 | p=0.15 |
| Location N (%) | UCG 0 MCG 1 (5.9) LCG 7 (41.2) Pelvis 9 (52.9) | UCG 2 (11.1) MCG 1 (5.5) LCG 8 (44.5) Pelvis 7 (38.9) | p=0.53 |
RIRS: retrograde intrarenal surgery; LCG: lower calyceal group; MCD: middle calyceal group; UCG: upper calyceal group.
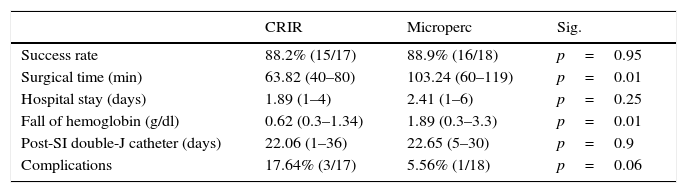
There were no intraoperative complications in any patient in both series. The success rate obtained was similar in both groups (88.2% for group A vs 88.9% for group B).
There was a clear difference in the surgical time used in both interventions, in favor of RIRS. The mean was 63.82min in group A, compared to 103.24min in group B (p=0.01). Statistically significant differences were also found in the fall of hemoglobin in favor of group A (0.62g/dl vs 1.89g/dl).
There were differences regarding postoperative complications, but without reaching statistical significance: 17.64% in group A and 5.56% in group B (p=0.062). All complications were Clavien I and II: 2 febrile syndromes and a mild hematuria in group A and a febrile syndrome in group B.
There were no significant differences in the days of hospital admission and duration of double J ureteral catheterization between both groups. All these values are expressed in Table 3.
Results.
| CRIR | Microperc | Sig. | |
|---|---|---|---|
| Success rate | 88.2% (15/17) | 88.9% (16/18) | p=0.95 |
| Surgical time (min) | 63.82 (40–80) | 103.24 (60–119) | p=0.01 |
| Hospital stay (days) | 1.89 (1–4) | 2.41 (1–6) | p=0.25 |
| Fall of hemoglobin (g/dl) | 0.62 (0.3–1.34) | 1.89 (0.3–3.3) | p=0.01 |
| Post-SI double-J catheter (days) | 22.06 (1–36) | 22.65 (5–30) | p=0.9 |
| Complications | 17.64% (3/17) | 5.56% (1/18) | p=0.06 |
RIRS: retrograde intrarenal surgery; g/dl: grams per deciliter; SI: surgical intervention; min: minutes.
There is no doubt at present that RIRS is widely used by urologists, and that more and more groups use it as the first treatment option for a very high percentage of renal lithiases.17 Technological advances have allowed it to achieve high success rates, with a high security profile.18 But not all are advantages in flexible ureteroscopy. The technique has some limitations that we cannot ignore, regardless of the lithiasic size. In the first place, the need to ascend a ureteral access sheath: in some patients this maneuver is impossible from the start and in a small percentage the ureter can be injured in its ascent.19 Secondly, the need for postoperative catheterization, with the corresponding morbidity that it causes in a significant number of patients.20 And, thirdly, the influence of the anatomy of the pyelocalyceal cavities on the results of the intervention: inferior calyces with excessively acute pyelocalyceal angle, infundibular stenoses or calyceal diverticula adversely influence retrograde access.21 In these cases where RIRS has limitations, PNL is presented as an effective alternative. After more than 30 years of history, PNL has shown a high rate of resolution, but at the same time accepting a certain morbidity, bleeding being the most frequent complication. Despite the generalized attempt to access the urinary tract through the calyx papilla chosen to minimize hemorrhagic complications, we know that a certain percentage of percutaneous accesses bleed. And it seems proven that one of the factors that can condition bleeding is the caliber of the tract.22 For this reason the miniperc was popularized in the adult in small and medium size lithiasis. Reducing the caliber of the tract, the hemorrhagic complications of standard PNL are reduced.5
Following this concept, Desai et al.6 developed micropercutaneous surgery. Using the initial idea of Markus Bader23 of all-seeing needle, they adapted the intervention to a 4.85Fr caliber. The channel of the shirt carried the lens of 0.9mm diameter, irrigation, and a laser fiber of 200μm. The quality of the micro-optics provided enough vision to perform the procedure safely. The main advantage was the lack of need for dilation of the tract, reducing the possibility of bleeding. From 2011 to the present, several series of cases of microperc in small and medium size stones (10–20mm) have been published, both in children and adults, with success rates around 90% and rates of complications close to 10%.7,24 And although the reported results are encouraging, the number of patients treated is small and limited to a few centers and, on the other hand, studies comparing microperc to other techniques prospectively are very scarce.
A clear restriction of microperc is the lithiasic size – the majority of authors limit that to 1.5cm – given the impossibility of extracting fragments.25 In this range of lithiasic size, it is in competition with extracorporeal shock wave lithotripsy and RIRS. Before these ideas, the following question arises: is microperc an alternative to RIRS? In order to answer this question Sabnis,15 in a prospective randomized study, compared 35 patients undergoing microperc to 35 patients undergoing RIRS for a lithiasic size smaller than 15mm. The success rate and operative time were similar; however, microperc caused greater fall in hemoglobin and greater pain, but it had less need for double J catheter. Ramón de Fata,16 in a prospective study with fewer patients, found no significant differences between the 2 techniques. In our study, the success rate of both techniques was similar (88.2% for RIRS vs 88.9% for microperc). But if we restrict the field to the lower calyx, microperc proves superior to RIRS in terms of lithiasic resolution, according to a retrospective study in lithiases smaller than 20mm conducted in 127 patients.26 This difference in success rate can be explained by anatomic factors limiting the lower calyx for RIRS that are not so much for microperc.21
However, microperc has limitations. One of them is the limited mobility provided by the miniaturized sheath within the renal cavities, which requires a completely straight access to the lithiasis, since tangential trajectories to the stone can make fragmentation impossible. And if during this, migration of fragments occurs, we are obliged to reconvert the procedure to RIRS or miniperc to reach a complete resolution. Although in our study we did not need to reconvert any case, in series with a large number of patients, such as the one by Hatipoglu (n=140) or Ganpule (n=1313), the miniperc reconversion rate for residue migration or poor vision was 8.57 and 6.47%, respectively.11,13
Regarding surgical time, no statistically significant differences were found in the 2 existing prospective studies15,16 and it did in the retrospective one by Armagan,26 in favor of microperc. In our study, however, significant differences were found in favor of RIRS (63.82min) versus microperc (103.24min). This difference in time can be explained by the limitations intrinsic to microperc: the inability to extract fragments and the possible migration of significant remains. These setbacks oblige us to carry out a more rigorous vaporization or fragmentation in this group, to avoid important residual fragments or reconversion to another technique that slows down the procedure. In our opinion, RIRS enables a faster lithotripsy, due to the greater versatility that this technique offers in the renal cavities.
In our study, there were no significant differences regarding the postoperative stay between the two groups (1.89 days in group A versus 2.41 days in group B), which is in line with the results obtained by Sabnis and Ramón de Fata.15,16 In contrast, Armagan finds differences in favor of RIRS.26 In any case, being 2 minimally invasive techniques, both allow a short period of admission and a quick recovery to daily life.
After a RIRS, ureteral catheterization with a double J catheter is usually the norm, due to the possible ureteral damage produced by the access sheath. In contrast, microperc is not always associated with a double J catheter, since it does not use a sheath of ureteral access. Large series, such as the one published by Hatipoglu,11 have a low double J catheter rate (6.43%). This fact represents a clear advantage, as indicated in the aforementioned comparative studies.15,26 In our study, however, we did not find this advantage in favor of microperc: postoperative catheter days were similar for both groups: 22.06 in group A and 22.65 in group B. A reasonable explanation of this difference is that the treated lithiasic size has been greater than that of the mentioned series. With lithiasic load close to 2cm, the post-lithotripsy remains and the surgical time increase, with the consequent need for a postoperative double J catheter.
Both techniques have a high safety profile. Microperc has a complication rate of around 10% in all existing series.7–13 In our study, we found no intraoperative complications. Regarding the evaluation of postoperative complications, there was no statistically significant difference: the results were 17.64% in group A and 5.56% in group B (p=0.062), all of them corresponding to Clavien I and II. In the RIRS group, 2 patients had fever and one mild hematuria. One patient submitted to microperc presented febrile syndrome. The prospective studies mentioned above did not find significant differences either.15,16 It should be noted that the complication rate found in the RIRS group is slightly higher than that reported by our group in 2014.4 This can be explained by the lower number of patients treated in the current study. We are convinced that a larger sample size would decrease the rate of complications.
Regarding bleeding, we did find statistically significant differences in favor of RIRS, although no study patient required transfusion. The fall of hemoglobin was 0.62g/dl for the RIRS group versus 1.89g/dl for microperc (p=0.01). Similar results were found by other authors.15,26 The profile of less invasiveness of RIRS supports these results.27
Finally, a controversial aspect of microperc is the high pressures that are reached in the renal cavities during some phases of the intervention, due to the absence of drainage through the percutaneous sheath. Pressures significantly higher than those achieved with standard PNL have been tested with this technique.28 However, it appears that this hyperpressure has no clinical repercussion, as our results show. This problem is not found in RIRS when working with a sheath of ureteral access.
LimitationsThe main limitation of our study is the absence of randomization of the patients, although both groups were homogeneous and comparable.
ConclusionMicroperc is an effective and safe procedure for the treatment of renal lithiasis smaller than 2cm, being considered as an alternative to RIRS in this lithiasic range. More prospective studies with a larger sample size are needed to confirm our results.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Cepeda M, Amón JH, Mainez JA, de la Cruz B, Rodríguez V, Alonso D, et al. Cirugía retrógrada intrarrenal y micro-nefrolitectomía percutánea en la litiasis renal menor de 2cm. Actas Urol Esp. 2017;41:516–521.