Female urethral strictures are a rare condition that significantly impacts patients’ quality of life. Patient-reported outcomes are crucial, yet data regarding sexual function and treatment satisfaction are scarce. We aimed to provide insights from a reconstructive referral center.
Patients and methodsWe conducted a retrospective analysis of women treated with ventral onlay one-stage buccal mucosa graft urethroplasty for urethral strictures between 2009–2023. We assessed objective (retreatment-free survival, ΔQmax) and subjective outcomes (validated patient-reported outcomes).
ResultsOf 12 women, 83% and 17% had iatrogenic and idiopathic strictures, respectively. Median number of prior interventions was 6. Strictures were located meatal and mid-urethral in 25% and 75%, respectively, 22% had the bladder neck involved. Median graft length was 2 cm. At median follow-up of 66 months, 33% of patients underwent stricture retreatment, but only one case occurred within the first 2 years postoperatively. The median improvement in maximum flow rate (ΔQmax) was 10 ml/s. Median International Consultation on Incontinence Questionnaire Female Lower Urinary Tract Symptoms Modules (ICIQ-FLUTS) scores were 8 for filling symptoms, 6 for voiding symptoms, and 3 for incontinence symptoms. Median ICIQ-FLUTSsex score was 4. Higher scores indicate a higher symptom burden. Median ICIQ-Satisfaction outcome and satisfaction scores were 18 and 7, respectively, reflecting high treatment satisfaction.
ConclusionsBuccal mucosal graft urethroplasty by ventral onlay for female urethral strictures yields effective, durable, and positively received outcomes. However, larger studies across multiple institutions are necessary to further assess its efficacy, especially regarding patient-reported experiences and sexual function.
La estenosis uretral femenina es una enfermedad poco frecuente que afecta significativamente la calidad de vida de las pacientes. Si bien los resultados comunicados por el paciente (PRO, por Patient Reported Outcomes) son cruciales, los datos relativos a la función sexual y la satisfacción con el tratamiento son escasos. Nuestro objetivo es ofrecer información procedente de un centro de referencia en cirugía reconstructiva.
Pacientes y métodosSe realizó un análisis retrospectivo de las mujeres con estenosis de uretra sometidas a uretroplastia ventral con injerto de mucosa oral en una etapa entre 2009 y 2023. Se evaluaron los resultados objetivos (supervivencia libre de retratamiento, ΔQmax) y subjetivos (resultados comunicados por el paciente validados).
ResultadosDe 12 mujeres, el 83% y el 17% presentaban estenosis iatrogénicas e idiopáticas, respectivamente. Las pacientes presentaban una mediana de 6 intervenciones previas. Las estenosis se localizaban en el meato y la uretra media en el 25% y el 75%, respectivamente; el 22% de los casos presentaba afectación del cuello vesical. La mediana de la longitud del injerto fue de 2 cm. En una mediana de seguimiento de 66 meses, el 33% de las pacientes se sometió a reintervención para la estenosis, pero sólo en un caso esta se produjo durante los primeros 2 años del postoperatorio. La mediana de mejora del flujo máximo (ΔQmax) fue de 10 ml/s. La mediana de las puntuaciones de los síntomas del tracto urinario inferior femenino del Cuestionario Internacional sobre Incontinencia (ICIQ-FLUTS) fue de 8 para los síntomas de llenado, 6 para los síntomas de vaciado y 3 para los síntomas de incontinencia. La mediana de la puntuación ICIQ-FLUTSsex fue de 4. Las puntuaciones más altas indican una carga sintomática mayor. Las puntuaciones de ICIQ-Satisfaction y de satisfacción fueron 18 y 7 (mediana), respectivamente, lo que refleja una alta satisfacción con el tratamiento.
ConclusionesLa uretroplastia con injerto de mucosa oral onlay ventral para la estenosis uretral femenina produce resultados eficaces, duraderos y percibidos positivamente por las pacientes. Sin embargo, son necesarios estudios multicéntricos más amplios para evaluar su eficacia en profundidad, especialmente en lo que se refiere a los PRO y la función sexual.
Female urethral strictures are a rare yet often overlooked condition, constituting approximately 1% of all cases among women with lower urinary tract symptoms (LUTS).1 The primary therapeutic approach typically involves urethral dilatation, which may necessitate repeated sessions or supplemented by intermittent self-dilatation. However, in cases of recurrent female urethral stricture or for those seeking a more definitive solution, urethroplasty, predominantly utilizing augmentation techniques, is recommended.2 Despite the importance of this procedure, comprehensive evidence on optimal techniques for reconstructing the female urethra is lacking, largely due to the rarity of the disease itself. A recent scope search conducted by the European Association of Urology (EAU) urethral stricture guideline panel revealed limited data, with hardly more than 250 women identified as having undergone open augmentation techniques.2 While various augmentation options exist, buccal mucosal graft urethroplasty (BMGU), in particular, emerges as the most commonly technique.2,3 BMGU has shown promising patency rates ranging from 63% to 100%; however, understanding of its long-term efficacy remains limited, largely due to the relatively short median follow-up periods in existing studies.2
Another critical quality metric following urethral reconstruction, especially in women, whose anatomical considerations significantly differ from men due to their close proximity to the vaginal canal and the urinary sphincter, is patient-reported outcome measures (PROMs).4 Recently, these measures have been integrated into standardized follow-up protocols after open urethroplasty as recommended by the EAU guidelines.2,5 Particularly, the evaluation of postoperative sexual function after urethral stricture surgery has been implemented into the guidelines with a strong recommendation. However, it is crucial to acknowledge that evidence of sexual function after female urethral stricture surgery is largely nonexistent, and our comprehension of patient experience post-surgery, particularly regarding predominantly understudied domains such as sexual function and satisfaction with the surgical outcome, remains limited.
Against this backdrop, our aim was to deliver comprehensive long-term outcomes of one-stage BMGU in women presenting with urethral strictures refractory to conservative treatment measures. Additionally, we prioritize the utilization of validated PROMs to ensure a holistic understanding of the treatment's effectiveness from the patients' perspective. Through our study, we endeavor to deepen the understanding of female urethral stricture treatment and make a significant contribution to patient-centered care in this field.
Patients and methodsStudy populationWe performed a retrospective analysis of our institutional data including women undergoing BMGU for urethral stricture between 07/2009-05/2023, which was approved by the ethics committee of the medical council of Hamburg (PV4123) and was conducted based on local laws (Hamburgisches Krankenhausgesetz, HmbKHG §12.1). We excluded transwomen (n = 5) and women with simultaneous urethrovaginal fistula closures (n = 4) to mitigate etiological bias. By digital chart review we extracted clinical, etiological, and surgical characteristics as depicted in Table 1.
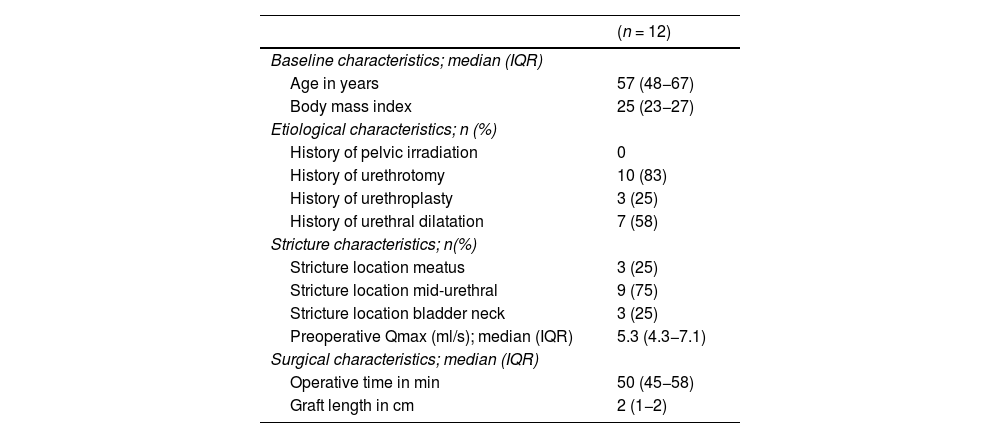
Clinical, etiological, and surgical characteristics of 12 female patients undergoing buccal mucosal graft urethroplasty for urethral strictures.
| (n = 12) | |
|---|---|
| Baseline characteristics; median (IQR) | |
| Age in years | 57 (48−67) |
| Body mass index | 25 (23−27) |
| Etiological characteristics; n (%) | |
| History of pelvic irradiation | 0 |
| History of urethrotomy | 10 (83) |
| History of urethroplasty | 3 (25) |
| History of urethral dilatation | 7 (58) |
| Stricture characteristics; n(%) | |
| Stricture location meatus | 3 (25) |
| Stricture location mid-urethral | 9 (75) |
| Stricture location bladder neck | 3 (25) |
| Preoperative Qmax (ml/s); median (IQR) | 5.3 (4.3−7.1) |
| Surgical characteristics; median (IQR) | |
| Operative time in min | 50 (45−58) |
| Graft length in cm | 2 (1−2) |
IQR = interquartile range.
Cross-sectional follow-up was conducted via phone (JK) and electronically via an online survey between October 2023 and January 2024. The objective study outcomes were evaluated based on two endpoints: Firstly, functional success, defined as retreatment-free survival, was assessed by phone with retreatment defined as any reintervention for true urethral stricture recurrence,6 and secondly, the ΔQmax, representing the change in uroflowmetry maximum flow rate (Qmax) from preoperative to 21 days postoperative at the time of a combined radiographic and functional voiding trial was extracted from digital charts. Secondly, validated PROMs were used to report subjective outcomes: International Consultation on Incontinence Questionnaire Female Lower Urinary Tract Symptoms Modules (ICIQ-FLUTS),7 Female Sexual Matters Associated with Lower Urinary Tract Symptoms Module (ICIQ-FLUTSsex),7,8 and ICIQ-Satisfaction (ICIQ-S).9 The PROMs were self-administered via a pseudonymized online survey.
Surgical procedure and perioperative managementPatients were evaluated preoperatively according to the institutional urethroplasty protocol,10 which included a detailed medical history, physical examination, urinalysis and respective antimicrobial treatment,11 vaginal inspection, cystoscopy, and retrograde and voiding cystourethrography. The surgical procedure was performed by two experienced surgeons (RD, MF) with extensive expertise in urethral reconstruction and female urology. All women underwent BMGU, using a ventral onlay technique via a stricturotomy at 6 o’clock, according to the nomenclature as suggested by the most recent EAU guidelines.2 In summary, the patient was placed in the lithotomy position, and the procedure began with a midline incision in the anterior vaginal wall near the proximal end of the stricture. After entering the paraurethral plane, both sides of the anterior vaginal wall were mobilized to provide clear access to the entire posterior urethral section from 3 to 9 o'clock. A stricturotomy was then performed at the 6 o'clock position, extending the incision along the entire length of the stricture and approximately 5 mm beyond either end of it. Next, three stay sutures were placed, each incorporating the urethral mucosa, to facilitate the positioning of the buccal mucosal graft. Adequate graft material was harvested from the inner cheek to cover the entire length of the stricturotomy. An 18 F Foley catheter was then inserted, and the buccal mucosal graft was sutured onto the stricturotomy using continuous 4-0 monofilament absorbable sutures. In cases where sufficient sponge tissue was present, it was sutured over the graft. The vaginal epithelium was meticulously closed using a continuous suture technique with a 3-0 monofilament absorbable suture to ensure optimal healing. To maintain the integrity of the repair and assist with hemostasis, a small vaginal pack (tamponade with iodoform and panthenol) was gently inserted. The Foley catheter was retained for 21 days, after which a standardized radiographic and functional voiding trial was conducted to assess the healing of the graft, evaluate for potential extravasation, perform uroflowmetry, and measure post-void residual volume.12
Statistical analysesThe distribution of clinical, etiological, and surgical characteristics was presented as frequencies and proportions, and for continuous variables, medians with interquartile ranges (IQRs). The median follow-up was calculated using reverse Kaplan-Meier estimates in censored patients and retreatment-free survival estimates were calculated for median follow-up and at two and five years. PROMs were scored according to the respective user manuals and their distribution was depicted graphically in violin plots. Female LUTS and their impact on quality of life were assessed using the ICIQ-FLUTS questionnaire. Specifically, filling, voiding, and incontinence symptoms were evaluated separately using the respective symptom subscales which ranged from 0 to 16, 0 to 12, and 0 to 20.7 Female sexual matters, including pain and discomfort due to a dry vagina, the impact of urinary symptoms on sexual function, pain during sexual intercourse, and urine leakage during sexual intercourse, were assessed using the comprehensive ICIQ-FLUTSsex scale which ranged from 0 to 14, with higher values indicating increased symptom severity.8 Treatment satisfaction was assessed using the ICIQ-S outcome score, which is a scale ranging from 0 to 24. This score incorporates six questions to evaluate satisfaction with surgical outcomes, along with an item that measures overall satisfaction with surgery, scored from 0 to 10.9 All statistical analyses were performed using Stata® (StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC). Reported P values are two-sided, and a value of less than .05 was considered to be indicative of statistical significance.
ResultsClinical, etiological, and surgical characteristicsA total of 12 patients underwent one-stage BMGU for female urethral stricture between July 2009 and September 2023. The median age of the cohort was 57 years (IQR 48−67), and the median body mass index was 25 (IQR 23−27). None of the patients had a history of pelvic radiotherapy. The strictures were predominantly iatrogenic in 10 patients (83%) and idiopathic in two patients (17%). The median number of prior urethral interventions was 6 (IQR 3–10). Regarding the location of the strictures, three cases (25%) were isolated meatal stenoses, 9 (75%) were mid-urethral, and 2 of the latter (22%) had additional bladder neck and sphincter involvement. The median operative time was 50 min (IQR 45−58), and the median graft length was 2 cm (IQR 1−2). Clinical, etiological, and surgical characteristics are depicted in Table 1.
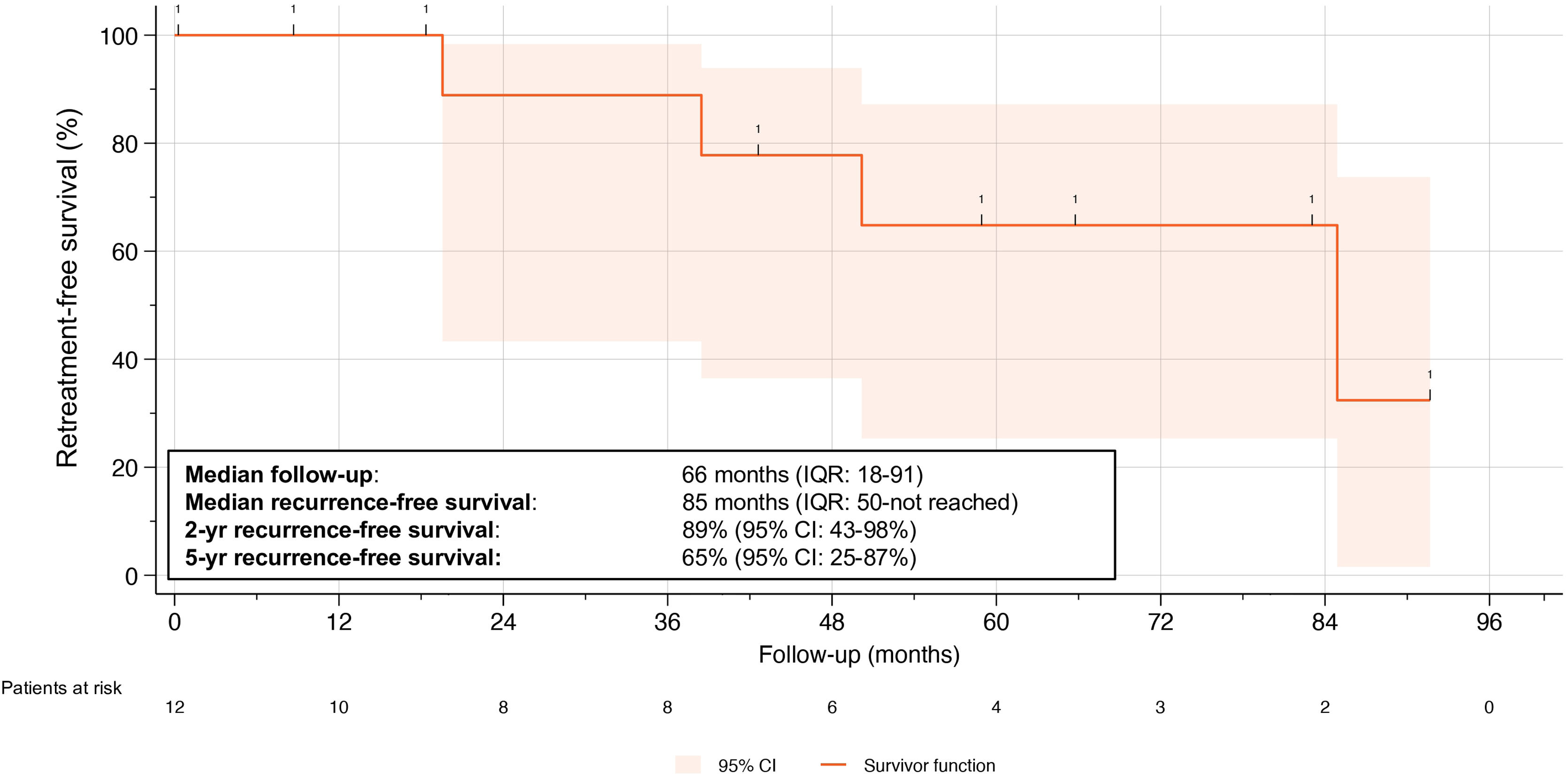
Objective retreatment-free survivalOverall, four patients (33%) experienced recurrent strictures according to our definition at a median follow-up of 66 months (IQR 18–91); of these, three required dilatation, and one underwent urethrotomy. This translated into a median stricture recurrence-free survival rates of 85%, 89% at two years, and 65% at five years (Fig. 1). Notably, only one of the four recurrences occurred within the first two years postoperatively, while the others occurred after three, four, and seven years, respectively. The median preoperative maximum flow rate (Qmax) was 5.3 ml/s (IQR 4.3−7.1), which increased to 18 ml/s (IQR 14–29) at 21 days postoperatively, resulting in a median change in Qmax (ΔQmax) of 10 ml/s (IQR 9.4−35 ml/s).
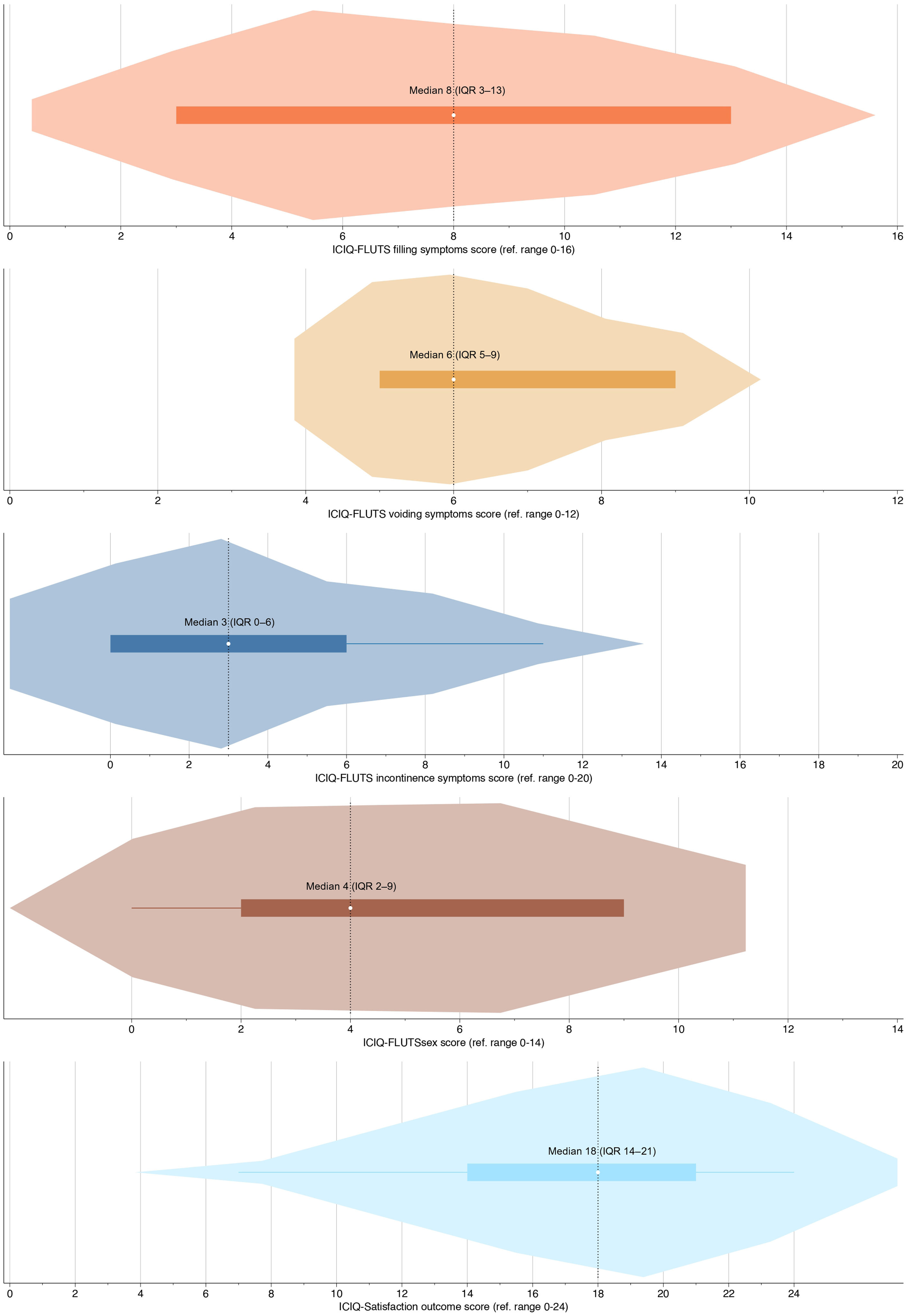
Subjective patient-reported outcomesMedian time for PROM completion was 59 months (IQR 19–83), and complete PROM questionnaires were available in seven patients (58%), of which two had stricture recurrence (29%). Despite multiple attempts, we were unable to reach 5 out of the 12 patients (42%) by phone, leading to their classification as lost to follow-up for the PROMs. The overall distribution of PROM scores is depicted in Fig. 2. Median ICIQ-FLUTS subscales for filling symptoms, voiding symptoms, and incontinence symptoms were 8 (IQR 3–13), 6 (IQR 5–9), and 3 (IQR 0–6), respectively. The median FLUTSsex score was 4 (IQR 2–9), with higher scores indicating a greater symptom burden. The median ICIQ-S outcome score was 18 (IQR 14–21), and the median satisfaction score was 7 (IQR 1–9). It is important to note that higher scores on the ICIQ-S denote greater treatment satisfaction with the surgical outcome.
DiscussionOver recent years, the surgical techniques for BMGU in females have experienced minimal evolution.2 However, our understanding of what constitutes a successful procedure has dramatically evolved.6 Success is no longer defined merely by technical and anatomical outcomes; PROMs and patient-reported experience measures of surgical success have emerged as critically important factors. Bearing this perspective in mind, our study presents valuable insights from an institutional series of 12 women who underwent one-stage BMGU over the last 15 years. This series sheds light on patients' perceptions of success and identifies functional parameters that should be prioritized when evaluating the effectiveness of this surgical technique in the context of female LUTS.13
Even with a notably longer follow-up of five years, our objective success rate remains consistent with those reported in the literature. For dorsal onlay BMGU, success rates range from 63% to 100% over a follow-up period of six to 33 months. On the other hand, for ventral onlay BMGU, success rates range from 92% to 100% across a follow-up of six to 25 months.14–21 The comparison between the two approaches is often hindered by the inconsistent use of nomenclature for ventral and dorsal approaches, leading to varied and sometimes contradictory definitions.22–24 To address this ambiguity, a group of esteemed surgeons with great expertise in reconstructive urology proposed adopting the terms “anterior” and “posterior” instead of “ventral” and “dorsal”. In their proposal, posterior refers to the region corresponding to the dorsal aspect of the patient when standing, which is the aspect facing the anterior vaginal wall. Anterior, on the other hand, refers to the ventral part facing the pubic bone. Consequently, in our series, patients were treated with posterior onlay BMGU. However, considering the absence of randomized evidence comparing dorsal and ventral augmentation, even in male urethroplasty, it is reasonable to infer that the approach may not notably alter treatment outcomes.
Our PROMs results are notable due to the absence of an available comparator, as most retrospective studies on urethroplasties for female strictures have not incorporated PROMs. While only a select few studies have explored postoperative LUTS through PROMs following BMGU in females,15,19,20 our study stands out as the first to evaluate postoperative sexual function and treatment satisfaction. Our findings suggest that, while patients are generally satisfied with their treatment, the majority continue to experience symptoms across all categories. This may indicate differences in outcomes compared to their male counterparts undergoing the same procedure.5 These findings underscore the complexity and challenge of treating female urethral strictures, emphasizing the need for more focused research in this area.
It is important to acknowledge that our study has limitations, primarily a small sample size of only 12 patients over a period of 15 years. This can be attributed in part to our strict exclusion criteria aimed at minimizing etiological intrinsic bias. Nonetheless, it underscores the reality that even at a widely recognized referral center, only approximately one woman per year presents for open urethral stricture treatment. We look forward to the results of larger, multi-institutional studies, which will provide a more comprehensive understanding of the outcomes and experiences of patients undergoing BMGU for female urethral strictures.25 There are several additional limitations to our study, including its retrospective and monocentric design, the moderate response rate of approximately 60% to questionnaires, and the absence of preoperative PROM assessment. This last limitation renders comparison of pre- and post-treatment data unfeasible. Nonetheless, despite these limitations, our study contributes valuable insights to the existing body of literature. It does so by incorporating detailed patient-reported experience measures, utilizing both innovative and guideline-recommended validated questionnaires. Additionally, our study benefits from extensive long-term follow-up, further enriching its contribution to the field.
ConclusionsOne-stage ventral onlay BMGU for female urethral strictures, performed at a center specializing in reconstructive urology, has been found to be an effective treatment with long-lasting results and positive subjective outcomes. Nonetheless, further exploration of patient-reported experience measures, sexual function, and treatment satisfaction in larger, multi-institutional series is needed to investigate the equal efficacy compared to males undergoing similar procedures.
Conflicts of interestNo conflicts of interest are reported by the authors.
Collaborators:
J. Adamowicz1, Ł. Białek2, F. Campos-Juanatey3, F. Chierigo4, A. Cocci5, M. Frankiewicz6, F.X. Madec7, G. Mantica8, M. Oszczudłowski2, E.J. Redmond9, C.M. Rosenbaum10, W. Verla11, M. Waterloos11,12
1Department of Regenerative Medicine, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
2Department of Urology, Centre for Postgraduate Medical Education, Warsaw, Poland
3Andrology and Reconstructive Urology Unit, Marqués de Valdecilla University Hospital, School of Medicine, Cantabria University, IDIVAL, Santander, Spain
4Department of Urology, Azienda Ospedaliera Nazionale SS. Antonio e Biagio e Cesare Arrigo, Alessandria, Italy
5Department of Urology and Andrology, Careggi Hospital, University of Florence, Florence, Italy
6Department of Urology, Medical University of Gdańsk, Gdańsk, Poland
7Service d’Urologie, Hôpital Foch, Suresnes, France
8Department of Surgical and Diagnostic Integrated Sciences (DISC), University of Genova, Genova, Italy
9Department of Urology, Cork University Hospital, Cork, Ireland
10Department of Urology, Asklepios Hospital Barmbek, Hamburg, Germany
11Department of Urology, Ghent University Hospital, Ghent, Belgium
12Department of Urology, AZ Maria Middelares, Ghent, Belgium.
Please cite this article as: Klemm J, Marks P, Schulz RJ, Filipas DK, Stelzl DR, Dahlem R, et al. Uretroplastia femenina con injerto de mucosa oral en una etapa: resultados comunicados por las pacientes y tasas de éxito funcional a largo plazo. Actas Urol Esp. 2024. https://doi.org/10.1016/j.acuro.2024.04.002
The collaborators of the Trauma and Reconstructive Urology Working Party of the European Association of Urology Young Academic Urologists are presented in appendix 1.