INTRODUCTION
Eosinophilic colitis, a subtype of eosinophilic gastroenteritis, is a disease characterized by peripheral blood eosinophilia and a prominent eosinophilic infiltration in the intestinal mucosa. Some reports suggested possible involvement of food allergy as the mechanism of the disease 1,2. Although mast cells are thought to be critical effector cells in gastrointestinal allergic reactions 3-5, the role of mast cells in eosinophilic colitis still remains unclear. Very recently, we have reported a case of acute pancreatitis possibly caused by allergy to bananas 6. However, as far as we have examined literary, there has been no case report of eosinophilic colitis in which the number of mast cells was examined. Here we report a case of eosinophilic colitis in which an accumulation of mast cells in the interstitium of colon was demonstrated.
CLINICAL CASE
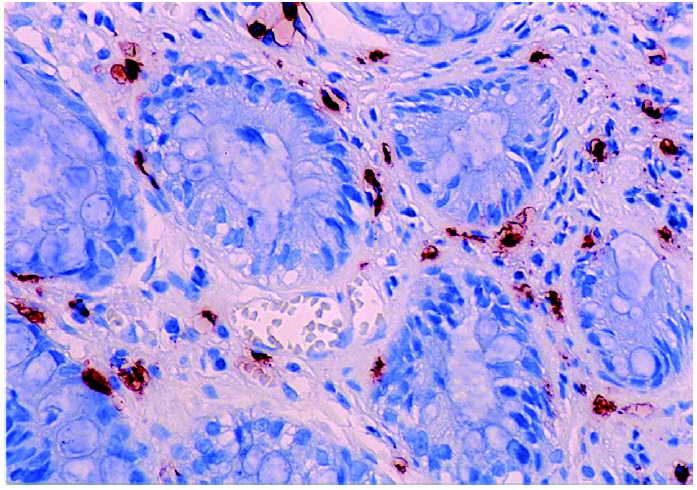
A 35-year-old man with chief complaints of chills and watery diarrhea visited the hospital on March 12th, 2004. In blood examination, CRP was 0.33 mg/ dl and peripheral blood leukocyte count was within normal range (8200/μl). No remarkable findings on physical examination were observed. Stool culture was negative for pathological bacteria. He was introduced to our allergy clinic by the finding of peripheral blood eosinophilia (17.9 %). A total serum IgE was 350 IU/ml, and IgE against Japanese cedar was 19.20 IU/ml. IgE levels against popular food antigens including fishes were all within normal ranges. No possible findings were present for parasite infection. Endoscopic examination of the upper digestive tract showed mild erosive change on the bulb, a small polyp at the fornix area and slight reddening change on the body of stomach. Biopsy could not be performed because reflex for vomiting was too strong. In colonoscopic examination, flare with slight edematous change was seen on both ascending colon and rectum, and biopsies were performed in each lesion. Hematoxylin-eosin staining with the biopsy specimens showed numerous eosinophil infiltration in the interstitium with edematous change of the tissue. The diagnosis of eosinophilic colitis was made by these findings with the clinical summary mentioned above. Immunohistochemical staining for human mast cell tryptase using monoclonal antibody against human mast cell tryptase (Chemicon, Temecula, Calif., USA) with the biopsy specimens showed an accumulation of mast cells in the mucosa and submucosa of colon (fig. 1). Counting the number of mast cells was done using an Olympus BX-50 microscope equipped with a 0.1 × 0.1 mm ocular grid (Olympus Eyepiece Micrometer U-OCMSQ 10/10) in 8 grid fields, and the mean was analyzed. The mean number of mast cells in ascending colon and rectum in eosinophilic colitis were 352/mm 2 and 405/mm 2, respectively.
Figure 1.--Immunohistochemical staining for human mast cell tryptase of the biopsy specimen from rectum of the patient. An accumulation of mast cells is seen in the mucosa and submucosa (magnification ×400). De Inamura et al.
Eating raw fresh-water fish seemed to be a highly possible cause of the complaints of the patient. However, provocation test could not be performed as the informed consent of the test was not obtained. Therefore, avoiding eating raw fresh-water fish conservativety followed him. He has been followed up without any specific treatment and the laboratory findings including the number of peripheral blood eosinophils became normal in a month. Until now, the patient has not suffered from any further attacks by avoiding digestion of raw fresh-water fish.
DISCUSSION
Eosinophilic colitis is a subtype of eosinophilic gastroenteritis. Histologic evidence of a predominant eosinophilic infiltration in the gastrointestinal mucosa in the absence of parasitic infection and extraintestinal diseases confirms a diagnosis of eosinophilic gastroenteritis 7. In some patients of eosinophilic colitis, food allergy seemed to be associated with the disease 1. However, direct evidence of allergy has not been consistently confirmed in eosinophilic colitis.
Mast cell granules are known to contain chemotactic mediators causing eosinophilic infiltration in tissues. Bischoff 8 reported that eosinophils and mast cells seemed to be mutually related in the allergic reaction in digestive tract mucosa. However, as far as we know, there is no case report of eosinophilic colitis in which the number of mast cells was examined. In this report we examined the number of mast cells in the interstitium of colon. Mean number of mast cells in ascending colon and rectum were 352/mm 2 and 405/mm 2, respectively. We could not investigate the number of mast cells in colon when the patient's condition became well because the informed consent of the test was not obtained. So as controls, biopsy specimens were obtained from the same site in five normal volunteers, and we examined the number of mast cells for comparison. The mean number of mast cells in normal control in ascending colon and rectum were 150 ± 16 (mean ± SD)/mm 2 and 126 ± 63/mm 2, respectively (data unpublished). Recently Sasaki et al 9 reported in their study that the number of mast cells in ascending colon and rectum from normal control were 122 ± 18 (mean ± SD) cells/mm 2 and 110 ± 16 (mean ± SD) cells/mm 2, respectively, and their findings are consistent with those of our study. Taken together, these findings indicate the number of mast cells in the interstitium of eosinophilic colitis may have increased in our present case. Further studies are required.
CONCLUSIONS
This is the first report of eosinophilic colitis showing an accumulation of mast cells in the interstitium.
Correspondence:
M. Kurosawa, MD
Gunma Institute for Allergy and Asthma
Shin-Ohra Hospital
3233-1 Shinozuka. Ohra-machi
Gunma 370-0615. Japan
E-mail: motohiro@shin-ourahp.or.jp