In recent years, the increasing use of spices has resulted in a rise of allergic reactions to them, especially in atopic patients. Curry is a mixture of several seeds such as coriander, onion, curcuma, caraway, cumin or mustard. Most of them belong to the Umbelliferae family.1 Contact dermatitis, the oral allergy syndrome and some cases of anaphylaxis are the most reported allergic reactions to these allergenic sources.2–5 Various pollen-food syndromes (PFS) have been described in pollinic patients, many of them produced by panallergens, but curry has never been included in them. However, some of the spices present in curry powder (parsley, caraway or coriander) have been reported as hidden allergens and cross-reactivity with mugwort pollens have been described (The celery–mugwort–spice syndrome).6
We describe a 45-year-old woman with rhinoconjunctivitis through May, June and September. She referred several episodes of papular lesions and pruritus in mouth mucosa, itching and erythema in face, palms and neckline immediately after eating several meals containing curry spices. No apparent relationship with other ingredients of the culprit meals as chicken, cous-cous or rice was suspected. The symptoms did not return when the patient ate the same meals cooking without curry. Skin prick test was positive to extracts from curry and coriander (Bial-Arístegui, Bilbao, Spain) (Fig. 1) as well as to pollens from Platanus acerifolia, Artemisa vulgaris and Chenopodium album (ALK-Abelló, Madrid, Spain). It was negative to other curry components: curcuma, mustard, cinnamon, onion, garlic, fennel, ginger, black pepper, laurel, nutmeg, cardamom and clove (Bial-Arístegui, Bilbao, Spain) and pollens from Olea europaea, Cupressus arizonica, Plantago lanceolata and Dactylis glomerata (ALK-Abelló, Madrid, Spain). Serum specific IgE was determined by EAST technique (enzyme allergo sorbernt test). Solid-phase was obtained by coupling the extract solution (10mg/mL) to the 6-mm diameter CNBr-activated paper discs, as described by Ceska and Lunqvist.7 EAST was performed following the manufacturer's instructions (Specific IgE EIA kit HYTEC HYCOR Biomedical Ltd. UK), and values equal to or higher than 0.35kU/L were considered positive. Serum specific IgE against extract from three different types of curry powder were 1.3, 1.9 and 2.2kU/L, respectively. Serum specific IgE measurements to three different types of curry powder were 1.3, 1.9 and 2.2kU/L, respectively. Among the species of the Umbelliferae family, it resulted positive to aniseed 2.2, dill 1.2, caraway 1, fennel 1.3, cumin 0.5 and coriander 0.5kU/L. It was negative to parsley, celery and carrot.
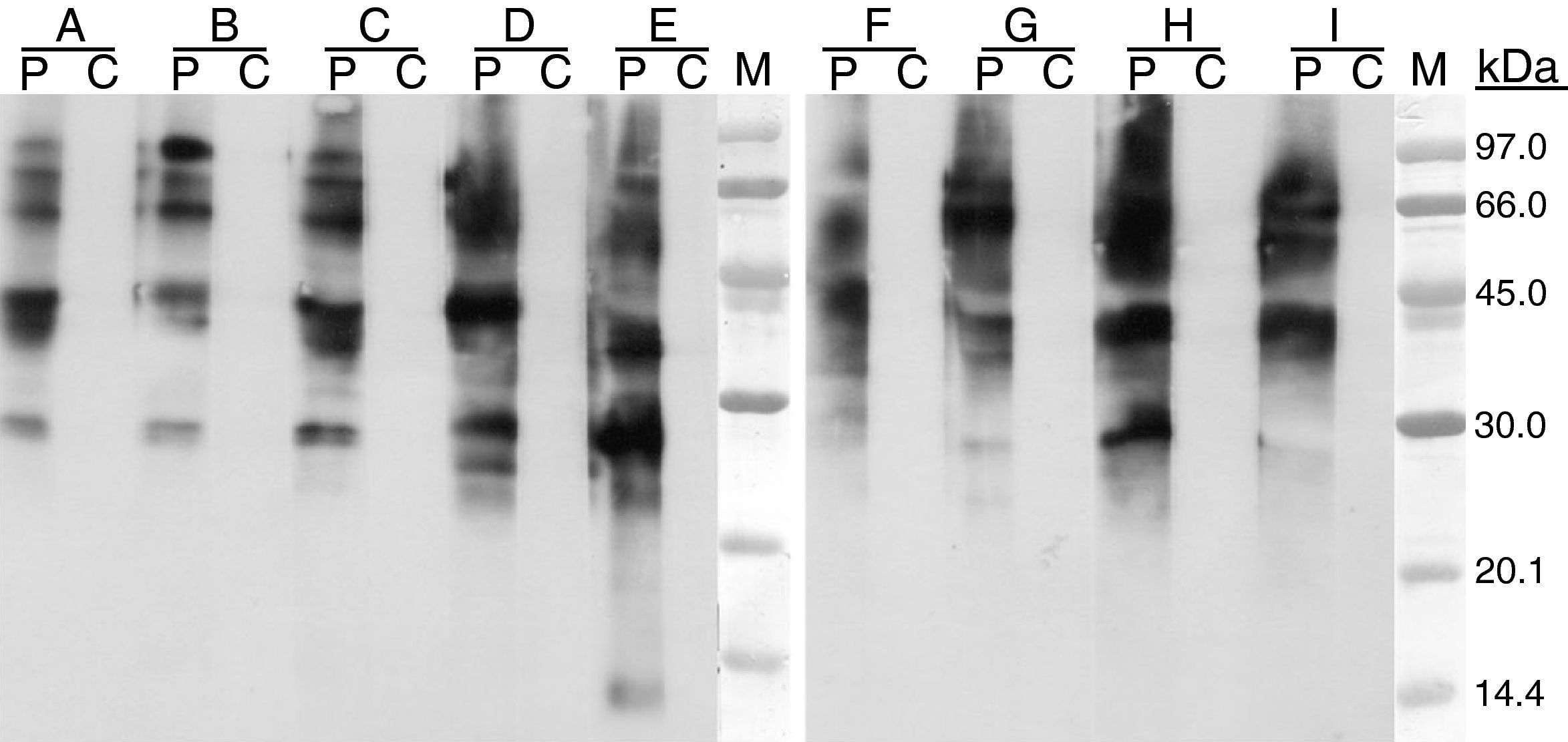
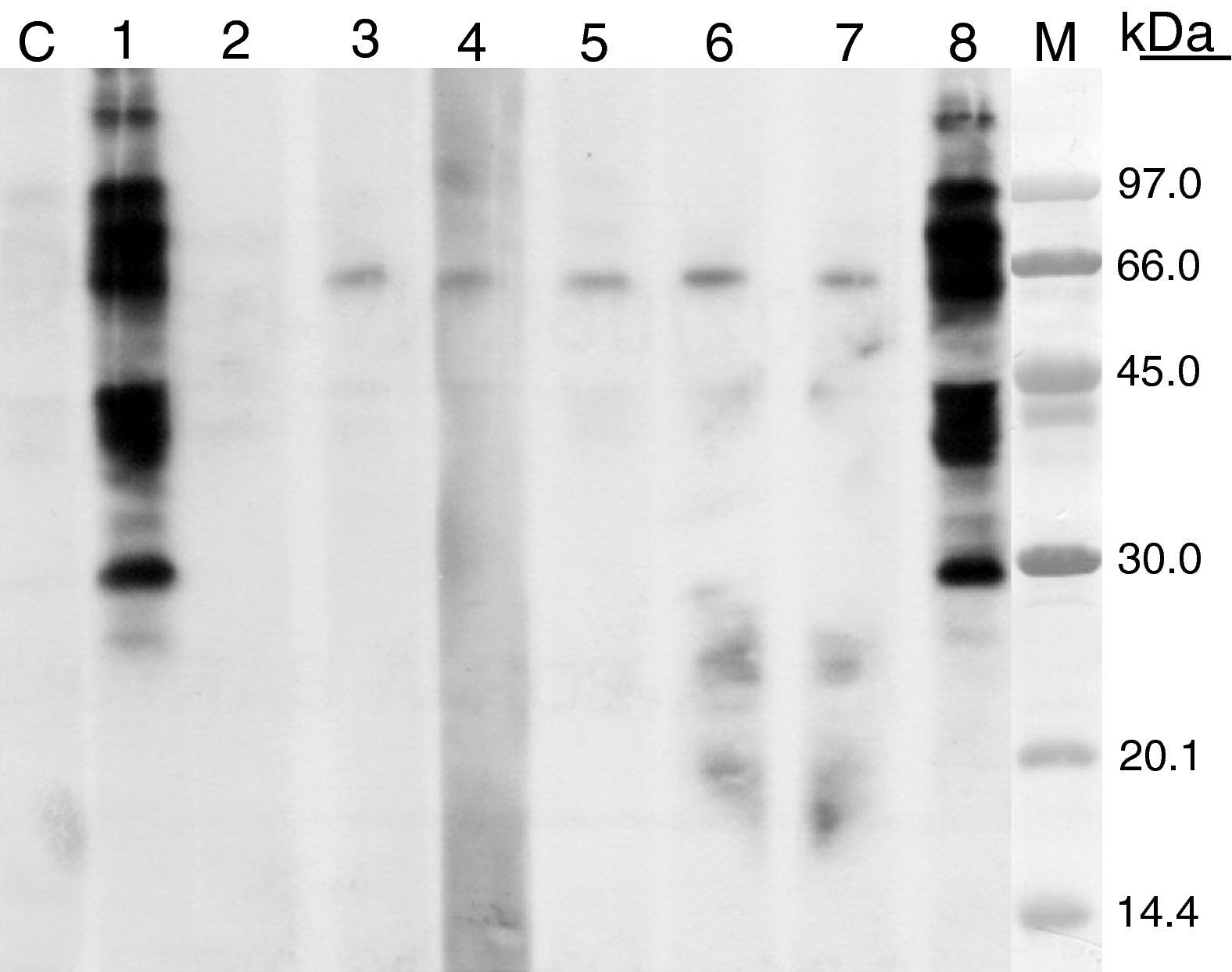
The molecular mass of the IgE binding protein was calculated by SDS–PAGE immunoblotting. SDS–PAGE was carried out according to the method of Laemmli,8 12.5% and 4% were used for separating and stacking gel, respectively. The samples were prepared in 0.125M HCl–Tris pH 6.8, 0.1% SDS, 5% β-mercaptoethanol at 100°C for 5min. When immunoblotting was performed, proteins were electrophoretically transferred to polyvinylene difluoride membrane (PVDF) and after membrane blocking with 5% dry skim milk (1h at 37°C), they were incubated with patient's serum (16h at 4°C); after washing they were incubated with peroxidase-conjugated mouse Anti-human IgE (-chains specific) (SouthernBiotech, USA), and detected by the chemioluminescence method as recommended by the manufacturer (ECL-Plus; Amersham Pharmacia Biotech). When immunoblotting inhibition was carried out patient serum was preincubated with the inhibition phases at 1mg/mL (overnight at 4°C). The IgE-binding pattern observed by immunoblotting with three types of curry powder and different spices were similar. The molecular masses of the IgE-binding bands ranged from 30 and 92kDa (Fig. 2). Cross-reactivity was studied by means of IgE-immunoblot inhibition assay, revealing allergenic relationship between curry and cumin or cilander and between curry and pollens from A. vulgaris, P. acerifolia and C. album (Fig. 3).
SDS–PAGE immunoblotting-inhibition. Curry extract in solid phase. Control serum (C), patient serum (1). Patient serum preincubated with extracts from: curry (2), cumin (3), coriander (4), Artemisia vulgaris pollen (5), Chenopodium album pollen (6), Platanus acerifolia pollen (7), lamb (8). M: molecular weight standards.
We present a case of immediate hypersensitivity to curry powder in an atopic patient. Skin prick test and specific IgE were positive to the spices of the Umbelliferae family present in curry as well as to pollens from the following families: Compositae, Platanacea and Chenopodiaceae.
The existence of specific IgE against common panallergens from pollens and plant-derived foods is a widely accepted and experimentally supported explanation for some of the allergenic relationships detected. Some of the responsible cross-reactive molecules for the development of PFS in weed pollinosis have been described in detail as profilin, LTPs, and high MW allergens and/or glycoallergens.9
Pollens from the Compositae family (Artemisia),9,10 Chenopodiacea9 and Platanacea pollens11 have been described as a cause of PFS with different fruits (e.g. banana, melon) but allergies to spices have never been associated to Platanaceae or Chenopodiacea pollens.
In this study we found in vitro cross-reactivity with clinical implications among food spices belonging to Umbelliferae family and pollens from the Compositae family (A. vulgaris), the Platanacea (P. acerifolia), and the Chenopodiaceae (C. album), due to allergens with molecular masses between 30 and 97kDa.
Sources of fundingAuthors disclose no financial relationship, which can cause a conflict of interest regarding this article.
Presented in poster session in the XXV Congress of the European Academy of Allergology and Clinical Immunology (EAACI), Vienna, June 2006.