Cushing’s disease is bilateral adrenocortical hyperplasia secondary to excessive secretion of ACTH by the pituitary gland. Angio-oedema is due to oedema in the deeper subcutaneous and submucosal tissues. We report a patient with acquired angio-oedema which developed after transsphenoidal surgery for Cushing’s disease (CD).
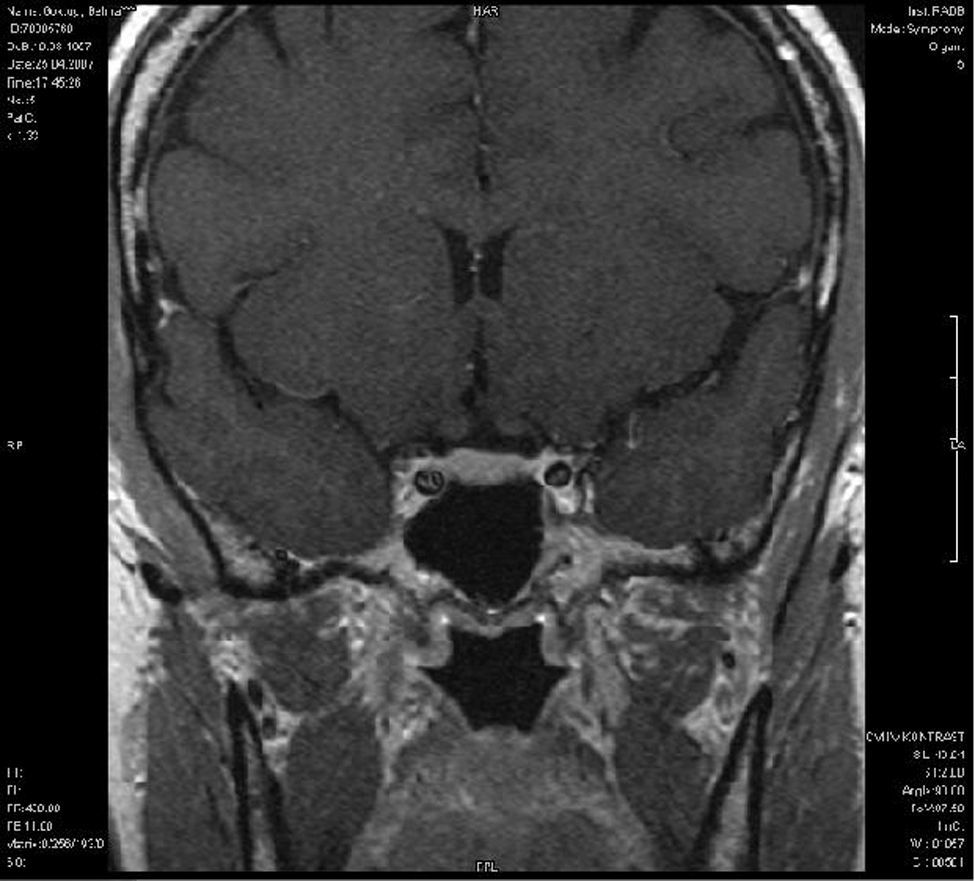
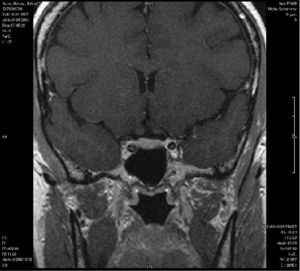
A 50-year-old woman admitted to the endocrinology department with a two-month history of weakness, weight gain, bruising and hypertension. On examination, she had moon facies, hypertrichosis, truncal obesity and non-pitting oedema. Results of laboratory investigations showed that baseline cortisol 40μg/dl (5–25μg/dl), urine cortisol 450μg/24 hours (80–120μg/24 hours) and ACTH 100pg/ml (0–46pg/ml) levels were out of the normal range. Serum cortisol levels failed to suppress after low dose dexamethasone (DST) (1mg>50μg/dl). Abdominal MR revealed a solid mass 1.9×1cm in size in the right adrenal gland; 2.3×1.5cm size in the left adrenal gland (Figure 1). Pituitary MR scan was found to be normal (Figure 2). Inferior petrosal sinus sampling showed elevated ACTH on the left side (central/peripheral ACTH ratio of 4) and ACTH secreting adenoma was diagnosed. The patient underwent trans-sphenoidal surgery (TSS). Histolopathology confirmed the diagnosis of adenoma. Postoperatively the patient’s serum cortisol levels remained low (1.8μg/dl) and prednisone was initiated at a dose of 7.5mg/d for six months. She was closely followed to determine the response to therapy as well as for the occurrence of any side effects.
Two weeks later the patient was seen by a dermatologist because of recurrent swelling of lips and periorbital area. She denied shortness of breath, change in voice and wheezing. The attacks were not associated with itching, redness, warmth and rash. There was no family history of similar complaints. Laboratory analysis including the blood counts, hepatic, renal, thyroid function tests, urinalysis and complement parameters (C1q, C3, C4, C1 esterase inhibitor activity) were found to be normal. Blood histamine concentration was 13nmol/L(4.5–9nmol/L). There was slight peripheral blood eosinophilia 6% (2–4%). Skin prick test was negative. Oral hydroxyzine hydrochloride 25mg twice a day for three months was prescribed. Remission occurred within three months of diagnosis and at one year follow up the patient was still asymptomatic.
Cushing’s syndrome refers to a state of hypercortisolism regardless of its aetiology. Screening for hypercortisolemia involves 24-hour urinary free cortisol, DST and pituitary MR imaging. Patients in whom MR findings are normal, should undergo Inferior Petrosal Sinus Sampling (IPSS) to confirm the diagnosis of Cushing’s disease.1 This test confirmed the diagnosis of ACTH secreting adenoma in our patient. She underwent TSS and adenoma was removed. In postoperative period, Hypothalamic-Pituitary-Adrenal (HPA) axis is often suppressed for months to years, resulting temporarily in adrenal insufficiency. The replacement treatment starts after surgery with 7.5–10mg of prednisone daily and often lasts 6 months to 2 years.2 In our patient, prednisone 7.5mg/d was prescribed for six months. Despite prednisone therapy, probably due to the disrupted HPA axis, angio-oedema occurred.
The HPA axis responsiveness is regulated by multitude of factors, contributing to individual differences. Gender, hormonal status, and immune system are among these affecting factors.3 Menopause shows the greatest effect on HPA axis dysregulation.4 In addition, reduced HPA axis responsiveness in patients with atopic dermatitis and allergic asthma has been reported.5 Dyke et al. showed that basophils were activated by corticotrophin releasing hormone and ACTH in chronic urticaria. Response to ACTH was found stronger than normal controls. The authors concluded urticaria was associated with deranged function of the HPA axis.6 Moreover, subphysiological HPA axis response after TSS in Cushing’s Disease patients receiving steroids post-operatively has been observed. 7
A good clinical history is essential for determining possible cause of angio-oedema. Initial investigations for angio-oedema include screening test for haematological abnormalities, infections, rheumatologic conditions, thyroid dysfunction, hepatic and renal dysfunction. Physical examination and almost all laboratory tests including complement levels were normal in our patient. Only peripheral blood histamine and eosinophils were slightly elevated. She had no history of infection and drug intake except prednisone. Angio-oedema started two weeks after operation and lasted three months. No recurrence was observed in a one-year follow-up period. It seems possible that the pathogenetic mechanism for postoperative development of angio-oedema in our patient is mast cell activation followed by degranulation and secretion of mediators as histamine, triptase, and chymase. This presumption has been substantiated by slightly increased histamine concentration. Mast cell activation together with the activation of lymphocytes, macrophages, eosinophils and neutrophils, also leads to transcription of a variety of cytokines including TNF-α (tumour necrosis factor-α), interleukin-3 (IL-3), IL-4 and IL-5; synthesis of lipoxygenase products as LTC4 (leukotriene C4) and LTD4; and the COX (cyclo-oxygenase) product PGD2. Increased production of cytokines and prostaglandins, potent synergistic inducers of endothelin (ET) and nitric oxide (NO) synthesis, results in increased ET and NO levels.8 ET, probably via ETB receptors, also increases NO secretion. NO is known as the most powerful vasoactive mediator causing vasodilatation.9 Interacting with vascular endothelial growth factor (VEGF) NO increases vascular permeability.10
Our case is interesting because angio-oedema developed after trans-sphenoidal surgery for Cushing’s disease. Despite glucocorticoid replacement therapy, HPA axis dysregulation may cause angio-oedema attacks. Return of normal HPA axis function can explain the disappearance of the disease.