Asthma diagnosis is difficult in infants with recurrent respiratory symptoms. Most children with asthma develop symptoms within the first three years of life. Clinically, these children are difficult to differentiate from those who have recurrent symptoms due to different causes, particularly from those with transient wheezing. After ruling out possible causes of chronic respiratory symptoms, the next step is to assess severity and frequency of symptoms in order to initiate controller therapy. Inhaled corticosteroids (ICS) are the first line medication for asthma management in all age groups under an appropriate diagnosis. Failure to respond to a six-week trial of ICS should certainly prompt re-evaluation rather than increase in doses. If ICS are commenced and there is no beneficial effect, clinical guidelines would recommend they be discontinued. There is concern about excessive use of ICS and in higher dosages. Even though they are the preferred drugs for all severities of asthma, in most children with mild disease, control can be achieved with inhaled corticosteroids. Clinically they are more effective for maintenance treatment and improve outcomes to a greater extent than any other drug available for patients with mild persistent asthma. At therapeutic dosages for three months, nebulised corticosteroids did not seem to suppress the HPA axis in infants 6–24 months old with recurrent or persistent wheeze.
A consensus report endorsed by EAACI and AAAAI, the PRACTALL initiative, recommends inhaled corticosteroids for children more than two years old as regular controller therapy to reduce bronchial inflammation in asthma.1 Despite this information, there are few data and no general consensus on how to treat recurrent wheezing in children less than two years of age.
A multi-centre, multi-national study (The International Study of Wheezing in Infants) was conducted in Curitiba, Brazil aiming to (1) verify the prevalence; (2) clinical characteristics; and (3) risk factors of recurrent wheezing in the first year of life. This cross-sectional study approached parents of infants 12–15 months old, who attended 35 randomly selected Health Centres for routine immunisation and they were requested to respond fully or to at least 95% of questions. A questionnaire focused on wheezing characteristics, risk factors and prescribed medications was standardised and validated.2,3 Questions about treatment were: a) “Has your baby been treated with inhaled medications to relieve chest wheezing (bronchodilators)?”; b) “Has your baby been treated with inhaled steroids?”; c) “Has your baby been treated with leukotrienes modifiers?”; d) “Has your baby been treated with oral steroids?”
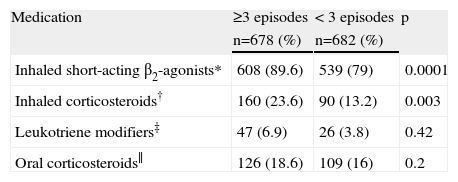
Parents of 3003 infants were involved. One thousand three hundred and sixty (45.3%) infants have had at least one wheezing episode and 678 (22.6%) had three or more episodes (recurrent wheezing).4 Recurrent wheezing infants used β2-agonists agents and inhaled corticosteroids more than those with less than 3 episodes. Leukotriene modifiers and oral corticosteroids have been used for both recurrent wheezing infants and for those who had less than 3 wheezing episodes (see Table I).
Treatment of infants according to the frequency of wheezing episodes
| Medication | ≥3 episodes | < 3 episodes | p |
| n=678 (%) | n=682 (%) | ||
| Inhaled short-acting β2-agonists* | 608 (89.6) | 539 (79) | 0.0001 |
| Inhaled corticosteroids† | 160 (23.6) | 90 (13.2) | 0.003 |
| Leukotriene modifiers‡ | 47 (6.9) | 26 (3.8) | 0.42 |
| Oral corticosteroids∥ | 126 (18.6) | 109 (16) | 0.2 |
Number of blank answers: 6*, 10‡, 12†, 20∥.
The limitations of our study were a convenience sample to reach a reliable number of individuals and information obtained by parental report. However, the high number of fully answered questionnaires allowed an adequate statistical analysis. Many countries monitor mortality and hospitalisation related to asthma, but there is less surveillance on medication use for recurrent wheezing in infancy.
ICS have been more prescribed than leukotriene modifiers as regular controller therapy for wheezing infants no matter whether the diagnosis of asthma was confirmed, a therapy which follows international guidelines. In spite of the difficulty to establish wheezing phenotype when transient and persistent wheezers overlap, infants with recurrent wheezing have been treated with inhaled corticosteroids as any other type of asthma. Viral respiratory infections are the main triggers of wheezing episodes in infancy. A trial of ICS may be considered in preschool children with frequent episodes or with family history of asthma but the clinical benefits of ICS for episodic viral wheeze are controversial.
An evidence-based approach indicates that ICS should be prescribed to 1–2 year-old babies if their symptoms are troublesome and if they show a clear response to treatment. The phenotypes used in epidemiological studies can only be applied retrospectively. They have improved understanding but they are of little use to the clinician. In addition, for infants younger than one year of age, ICS should not be prescribed, as evidence of efficacy is poor in this age group.
In conclusion, asthma starts early in life, recurrent wheezing is frequent in the first year of life, phenotypes overlap in this age group, paediatricians frequently prescribe controller asthma medication, demonstrating that evidence-based guidelines are little utilised in clinical practice. Free access to medication can change the decision in asthma management and could also influence the pattern of prescriptions in our population.5