Nasal sensation of airflow describes the perception of the passage of air through the nose. Nasal obstruction can be assessed using subjective techniques (symptom scores and visual analogue scales [VAS]) and objective techniques (anterior rhinomanometry [RMN], acoustic rhinometry [AR], and peak nasal inspiratory flow [PNIF]). Few studies have evaluated the correlation between these techniques.
ObjectiveThe primary objective of our study was to determine the degree of correlation between subjective and objective techniques to assess nasal obstruction.
Materials and methodsNasal obstruction was assessed using a symptom score, VAS, RMN, AR (minimal cross-sectional area [MCSA] and volume), and PNIF in 184 volunteer physicians. Spearman's rho was recorded. Correlations were considered weak if r≤0.4, moderate if 0.4<r<0.8, and strong if r>0.8.
ResultsMean (SD) age was 37.1 (6.9) years (range, 25–56 years); 61% were women. We found a strong correlation (r>0.8; p=0.001) between the different parameters of RMN and a moderate correlation between symptom score and VAS (r=0.686; p=0.001) and between MCSA and RMN (resistance) (r=0.496; p=0.001) and PNIF (r=0.459; p=0.001). The correlations were weak or non-significant for the remaining comparisons.
ConclusionNasal obstruction can be assessed using subjective and objective approaches. The correlations between objective techniques were moderate to strong. In addition, between subjective techniques we reported a moderate correlation. Finally, the correlations between the subjective and objective techniques were weak and absent. These findings suggest that each of the techniques assesses different aspects of nasal obstruction, thus making them complementary.
The nasal airways humidify, filter, and warm the air we breathe. Consequently, they account for 50% of resistance in the respiratory tract.1 Nasal obstruction is our perception of air passing through the nasal airways. It has been defined as discomfort caused by insufficient airflow in the nose or as the sensation of increased resistance of airflow through the nostrils. The sensation of airflow through the nose arises from the cooling of the sensory receptors in the nostrils during inspiration. These receptors are innervated by the trigeminal nerve, and anaesthesia or damage of this nerve can produce a sensation of nasal obstruction.2
Nasal obstruction is one of the main symptoms of the various conditions affecting the nose and may be due to anatomical abnormalities, inflammatory processes (eg. rhinitis), nasal polyps, and tumours.
Objective assessment of nasal obstruction involves direct examination of the area or volume of the nasal cavity or indirect analysis of nasal airflow and resistance.
Subjective assessment of nasal symptoms using symptom scores (including those examining nasal obstruction) are highly variable; therefore, the visual analogue scale [VAS] has been proposed as a tool to evaluate severity3. The most widely-used objective methods to assess nasal obstruction are active anterior rhinomanometry, acoustic rhinometry, and measurement of peak nasal inspiratory airflow (PNIF).3
A recent review evaluated recommendations on the use of these approaches and the correlations between them.4,5 Few studies have examined the correlation between subjective and objective methods for assessing nasal obstruction.4,6
We analysed the correlation between subjective and objective techniques used to evaluate nasal obstruction.
Materials and methodsDesignWe performed a prospective descriptive study based on the voluntary participation of 184 clinicians attending an educational course on rhinitis during the period 2002–2008. Nasal obstruction was subjectively assessed using a symptom score (0, absence of symptoms or mild symptoms; 1, moderate symptoms; and 2, severe symptoms) and a VAS scoring from 0 to 10cm (0 indicated absence of symptoms and 10 indicated more severe symptoms). Nasal obstruction was also objectively assessed using active anterior rhinomanometry to record airflow (RMN Q) and resistance (RMN R) during inspiration and expiration in both nostrils (Rhinospir PRO, Sibel, Barcelona, Spain), acoustic rhinometry (SER 2000, RhinoMetrics, Lynge, Denmark) to determine the minimal cross-sectional area (MCSA) and nasal volume (0–6cm and 0–12cm [V0–6 and V0–12]) from both nostrils, and measurement of PNIF in L/min (Clement Clark International, Essex, UK) by recording the highest result of three manoeuvres. Throughout the study, the same trained physicians assessed nasal obstruction using these subjective and objective approaches.
Statistical analysisQualitative variables were analysed using proportions. Quantitative variables were analysed using measures of position, central tendency, and dispersion. Values were compared using the Mann–Whitney test. The Spearman correlation coefficient (rho) was calculated. A 95% confidence level was set with a 5% alpha error. Statistical significance was set at p<0.05. Correlations were generally considered weak if r≤0.4, moderate if 0.4<r<0.8, and strong if r>0.8.7
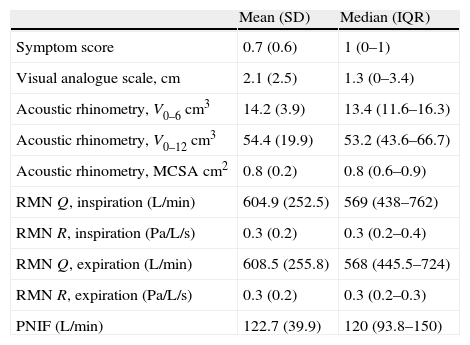
ResultsMean (SD) age was 37.1 (6.9) years with a range of 25–56 years. Women accounted for 61% of the sample. The values for the symptom score, VAS, active anterior rhinomanometry, acoustic rhinometry, and PNIF are shown in Table 1.
Subjective and objective variables in the assessment of nasal obstruction.
| Mean (SD) | Median (IQR) | |
| Symptom score | 0.7 (0.6) | 1 (0–1) |
| Visual analogue scale, cm | 2.1 (2.5) | 1.3 (0–3.4) |
| Acoustic rhinometry, V0–6 cm3 | 14.2 (3.9) | 13.4 (11.6–16.3) |
| Acoustic rhinometry, V0–12 cm3 | 54.4 (19.9) | 53.2 (43.6–66.7) |
| Acoustic rhinometry, MCSA cm2 | 0.8 (0.2) | 0.8 (0.6–0.9) |
| RMN Q, inspiration (L/min) | 604.9 (252.5) | 569 (438–762) |
| RMN R, inspiration (Pa/L/s) | 0.3 (0.2) | 0.3 (0.2–0.4) |
| RMN Q, expiration (L/min) | 608.5 (255.8) | 568 (445.5–724) |
| RMN R, expiration (Pa/L/s) | 0.3 (0.2) | 0.3 (0.2–0.3) |
| PNIF (L/min) | 122.7 (39.9) | 120 (93.8–150) |
VAS, visual analogue scale; V0–6, volume between 0 and 6cm; V0–12, volume between 0 and 12cm; MCSA, minimal cross-sectional area; RMN, anterior rhinomanometry; Q, airflow; R, resistance; PNIF, peak nasal inspiratory flow.
Pa/L/s, pascal/litre/second; L/min, litre/minute.
The correlations between the subjective and objective methods are shown in Table 2.
- (a)
Correlation between subjective methods
Symptom score and VAS were moderately correlated.
- (b)
Correlation between objective methods
Correlation between rhinomanometry variables
The values for RMN Q and RMN R correlated strongly in both inspiration and expiration.
Correlation between acoustic rhinometry variables
The values for V0–6 and V0–12 were moderately correlated; V0–6 and MSCA were weakly correlated.
Correlation between anterior rhinomanometry and acoustic rhinometry
MCSA correlated moderately with anterior RNM R in inspiration and weakly with RMN Q and RMN R. MCSA correlated weakly with all the anterior rhinomanometry values.
Correlation between acoustic rhinometry variables and PNIF variables
MSCA and PNIF were moderately correlated.
- (c)
Correlation between subjective and objective methods
Correlation between acoustic rhinometry and symptom score
Symptom score correlated weakly with acoustic rhinometry (V0–6 and MCSA).
Correlations between subjective and objective variables of nasal obstruction (Spearman rho).
| Symptom score | V0–6 | V0–12 | MCSA | RMN Q, inspiration | RMN R, inspiration | RMN Q, expiration | RMN R, expiration | VAS | PNIF | |
| Symptom score | 1.000 | −0.237a | −0.009 | −0.265a | −0.131 | 0.184 | −0.205 | 0.130 | 0.686b | −0.152 |
| V0−6 | −0.237a | 1.000 | 0.658b | 0.248b | 0.023 | 0.064 | 0.021 | 0.088 | −0.114 | 0.083 |
| V0−12 | −0.009 | 0.658b | 1.000 | −0.136 | 0.057 | 0.143 | 0.061 | 0.133 | 0.159 | −0.065 |
| MCSA | −0.265a | 0.248b | −0.136 | 1.000 | 0.300b | −0.496b | 0.257b | −0.322b | −0.151 | 0.459b |
| RMN Q, inspiration | −0.131 | 0.023 | 0.057 | .300b | 1.000 | −0.966b | 0.918b | −0.863b | −0.089 | 0.257b |
| RMN R, inspiration | 0.184 | 0.064 | 0.143 | −0.490b | −0.966b | 1.000 | −0.907b | 0.861b | 0.024 | −0.365b |
| RMN Q, expiration | −0.205 | 0.021 | 0.061 | 0.257b | 0.918b | −0.907b | 1.000 | −.893b | −0.090 | 0.188a |
| RMN R, expiration | 0.130 | 0.088 | 0.133 | −0.32b | −0.863b | 0.861b | −0.893b | 1.000 | −0.041 | −0.293b |
| VAS | 0.686b | −0.114 | 0.159 | −0.151 | −0.089 | 0.024 | −0.090 | −0.041 | 1.000 | −0.187 |
| PNIF | −0.152 | 0.083 | −0.065 | 0.459b | 0.257b | −0.365b | 0.188a | −0.293b | −0.187 | 1.000 |
V0–6, volume between 0 and 6 cm; V0–12, volume between 0 and 12 cm; MCSA, minimal cross-sectional area; RMN, anterior rhinomanometry; Q, airflow; R, resistance; VAS, visual analogue scale; PNIF, peak nasal inspiratory flow.
Analysis of the correlations between patients with greater or less nasal obstruction, depending on whether they had rhinitis at the time of the evaluation or whether they had a symptom score of 0–1 vs. 2–3 or a VAS score of <4 vs. >4, revealed no differences with respect to data obtained from an analysis of the total sample (data not shown).
DiscussionWe applied different subjective and objective techniques to assess nasal obstruction. The correlations between these techniques were generally weak or moderate. The most notable results were the strong correlation between the different parameters for active anterior rhinomanometry (r>0.8) and moderate correlation (0.4<r<0.8) between the symptom score and VAS and between MCSA and RMN R and PNIF.
VAS and several symptom scores have been shown to reveal changes in the severity of perceived nasal obstruction5 and a certain degree of correlation.8 We found correlations to be moderate; therefore, we suggest that both methods are similar when applied for subjective assessment of nasal obstruction.
Opinions on the value of objective assessment of nasal obstruction are divergent.4 PNIF has been used in several studies and its sensitivity is comparable to that of acoustic rhinometry and active anterior rhinomanometry.9,10 We found a moderate correlation with MCSA and a weak correlation with active anterior rhinomanometry.
Acoustic rhinometry has been compared with active anterior rhinomanometry. Its properties enable it to measure changes that are not assessed using active anterior rhinomanometry. Furthermore, several authors have found differences between the techniques and suggested that they should complement each other.11–13 Our weak correlations between the different variables in each technique, despite being moderate between MCSA and resistance, reinforce the concept that these techniques assess different aspects of nasal obstruction and are therefore complementary.
Correlations between subjective and objective measurements have also been investigated. In a study involving 250 volunteers, Jones et al.14 did not find an association between the subjective sensation of nasal obstruction and active anterior rhinomanometry. Gungor et al.15 did not find correlations between VAS and acoustic rhinometry during the nasal cycle. In other studies, the subjective nature of nasal obstruction correlates better with measurements of airflow resistance (RMN) than with acoustic rhinometry.16,17 A strong correlation has also been observed between PNIF and the subjective sensation of nasal obstruction.18
Despite the differences between subjective and objective techniques, all the methods provide reliable results and are used in several studies to evaluate the effect of treatment. Available data enable us to say that nasal obstruction should be evaluated using at least one subjective technique and one objective technique; PNIF should be reserved for outpatient monitoring of nasal obstruction.5
Although André et al.4 suggest that the presence of nasal obstruction could improve correlations between active anterior rhinomanometry and acoustic rhinometry, we did not find differences (data not shown) in the correlations depending on the degree of nasal obstruction. Consequently, correlations do not vary in patients who perceive greater nasal obstruction according to the symptom score, VAS, or presentation of symptoms of rhinitis at the time of the examination.
In conclusion, nasal obstruction can be assessed using subjective and objective approaches. The correlations between objective techniques were moderate to strong. In addition, between subjective techniques we reported a moderate correlation. Finally, the correlations between the subjective and objective techniques were weak and absent. These findings suggest that each of the techniques assess different aspects of nasal obstruction making them complementary.
Ethical disclosuresPatients’ data protectionConfidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentRight to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflict of interestThe authors have no conflict of interests to declare.
We thank Pablo Pons from Content Ed Net Madrid for Editorial Assistance.