To assess concordance in the measurement of peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1) between the portable device Piko-1 (Ferraris) and a pneumotachograph.
Patients and methodsForced spirometry (Master Screen Jaeger) was performed according to ATS/ERS norms, selecting the best value of three curves, and three measurements with the Piko-1 were recorded, following the recommendations of the manufacturer.
ResultsEighty patients between 5–18 years of age were studied. Based on the Bland-Altman method, the mean differences obtained were 9.82 (95%CI: 2.43–17.21) for PEF and 0.17 (95%CI: 0.12–0.21) for FEV1. The intraclass correlation coefficient was 0.96 (p<0,001; 95%CI: 0.93–0.97) for FEV1 and 0.93 (p<0,001; 95%CI: 0.89–0.95) for PEF.
ConclusionsPiko-1 offers FEV1 measurements close to those obtained with forced spirometry, thus allowing more exact patient assessment in home-based follow-up, emergency services, or hospital wards.
The high prevalence1 of paediatric asthma demands increased effort to improve our knowledge of the natural history of the disease and its impact upon patient quality of life.
Together with the case history, the study of lung function through forced spirometry constitutes a fundamental element in the diagnosis and follow-up of asthmatic patents. Without aiming to replace forced spirometry, portable peak expiratory flow (PEF) recorders have traditionally been used to monitor the patient's course, fundamentally in individuals with unstable asthma; when there is no good perception of the symptoms2; or to identify the possible triggering factors.3 Such devices can also be used to identify the onset of crises; to monitor treatment and self-control in the home in combination with educational programmes4; or to classify asthma according to its severity – this latter possibility currently being the subject of controversy.5 In addition, these devices are of great help in assessing lung function in places where no conventional flow/volume spirometer is available. This is typically the case in primary care centres,6 in emergency services, or for conducting field studies.
Portable devices make it possible to perform serial measurements in the home – thereby improving knowledge of the true situation of each individual patient, since routine forced spirometric assessment on the day of the visit to the clinic does not rule out alterations in ventilatory mechanics during other periods, because of the bronchial lability that characterizes these patients.
The recent introduction of portable electronic systems which measure and store to memory both PEF and forced expiratory volume in one second (FEV1) theoretically paves the way for better knowledge and control of the disease based on the latter respiratory parameter – which is less dependent upon patient coordinated effort and muscle strength in the context of the expiratory manoeuvre than PEF, which may underestimate airway obstruction, particularly in children.7
The present study analyses concordance between the portable device Piko-1® (Ferraris Cardiorespiratory, Louisville, CO, USA) (Fig. 1) and a pneumotachograph, in measuring the spirometric variables PEF and FEV1.
Patients and methodsThe Piko-1® is a small, light-weight electronic recorder equipped with a pressure/flow sensor which integrates the recorded signals via the installed software, comparing the registries obtained with the previously introduced reference values. The established range for PEF is 15-999lpm (resolution 1lpm), versus 0.15–9.99litres for FEV1 (resolution 0.01litres). After completing the manoeuvre, a colour-zone indicator based on the reference values appears alongside the value obtained: green if the result exceeds 80% of the reference value; yellow if between 50–80%; and red if under 50%. The device is also equipped with an alarm system and a quality indicator (observed onscreen as an exclamation mark) which indicates when the test must be repeated because of abnormally low or high recordings with respect to the reference values, insufficient patient exertion, a slow initiation, or the appearance of cough.
All the test data are stored in the memory of the device, with the possibility of performing table- and plot-based analyses via the installed software (Piko Trend) and an interface support. The data can also be sent via e-mail.
A descriptive, observational and cross-sectional study was made with randomised selection of 80 asthmatic children between 5-18 years of age seen in the paediatric pneumology clinic, and who were able to correctly perform forced spirometry with a pneumotachograph (Master Screen Jagge®) according to ATS/ERS norms,8 and using the reference values established by Zapletal. After selecting the best of three curves, three measurements were made with the PiKo-1®, with selection of the best registry. All patients who correctly completed forced spirometry were also able to correctly complete three manoeuvres with the PiKo-1®. The time elapsed between the two tests was less than three minutes, and in all cases forced spirometry was performed first, in order not to affect the results of the test which would serve to determine our criteria in each individual patient.
Following the recommendations of the manufacturer, we adjusted the values obtained with the portable device, multiplying them by 1.03, due to the height of the city of Madrid above sea level (1.5% adjustment for every 300metres when used at more than 300metres above sea level: approximately 600metres in the case of Madrid).
In both tests the patients were trained and controlled by a technician specialised in pulmonary function, and verbal informed consent was requested in all cases.
An analysis was made of concordance between the measurements obtained with the two systems in terms of the spirometric variables PEF and FEV1, based on the Bland-Altman method, and the intraclass correlation coefficient, using the SPSS version 11.0 statistical package.
ResultsThe 80 selected children presented a mean age of 10.03±3.45 years (range 5–18 years). There were 50 boys and 30 girls.
The mean FEV1 as percentage of the theoretical value was 100.73±16.18, with minimum of 52.7% and maximum of 128.48%; 26.2% of asthmatic children obtained a result of FEV1/FVC below 80%. With regard to asthma severity, 71% had a FEV1 greater than 80%, 10% between 60–80% and only one patient below 60%.
The mean values obtained by forced spirometry for both PEF and FEV1 were greater than those obtained with the Piko-1® (PEF: 273.8±91.4 versus 264.0±86.3litres/sec.; FEV1: 2.0±0.7 versus 1.8±0.6litres).
Analysis of the variables using the Pearson correlation test revealed excellent correlation between the two techniques for both PEF (r=0.93; p<0.001) and FEV1 (r=0.96; p<0.001). However, this test cannot correctly evaluate concordance between continuous variables. In the event of systematic error between the two measuring systems, the values could show excellent correlation but not good concordance.
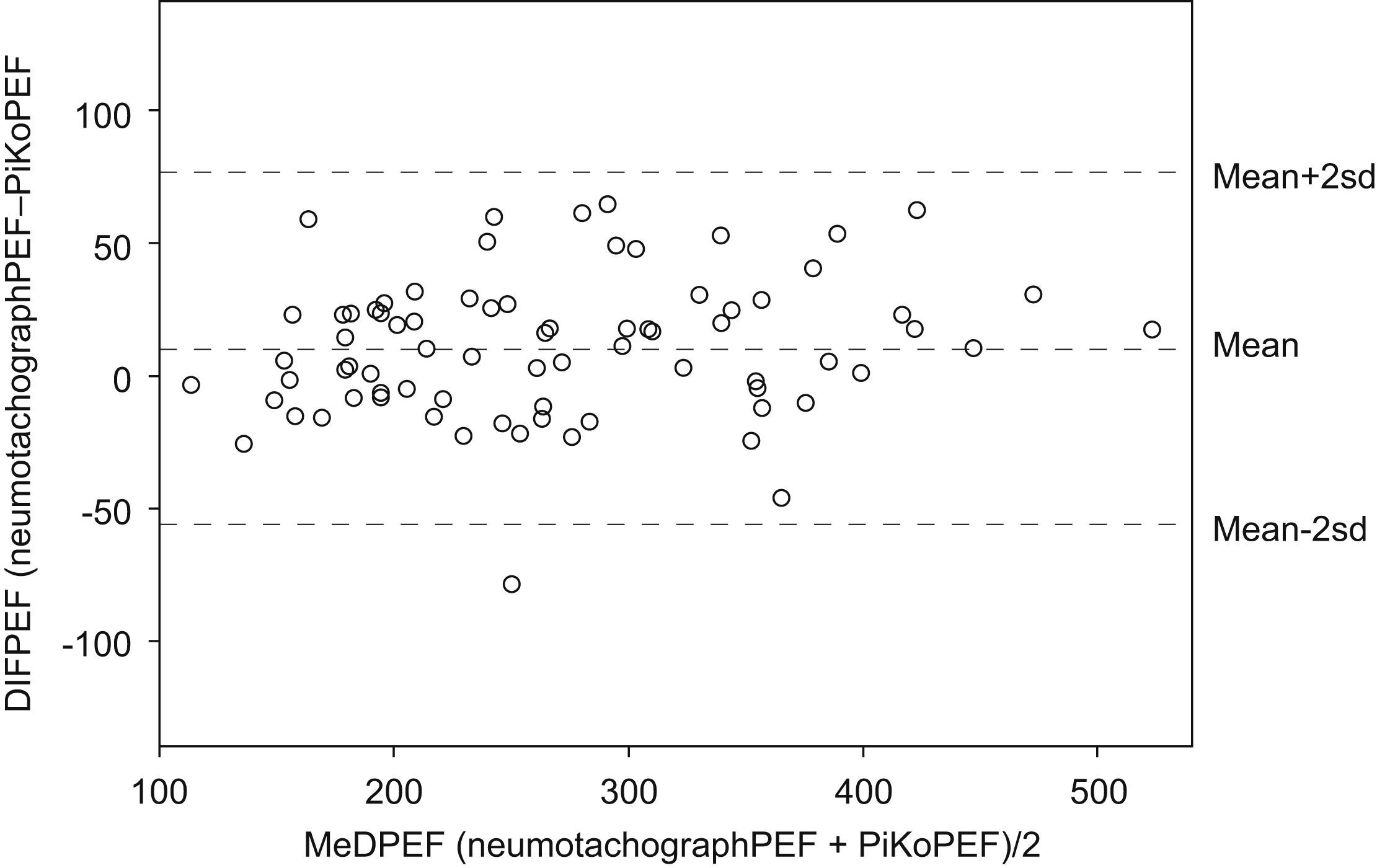
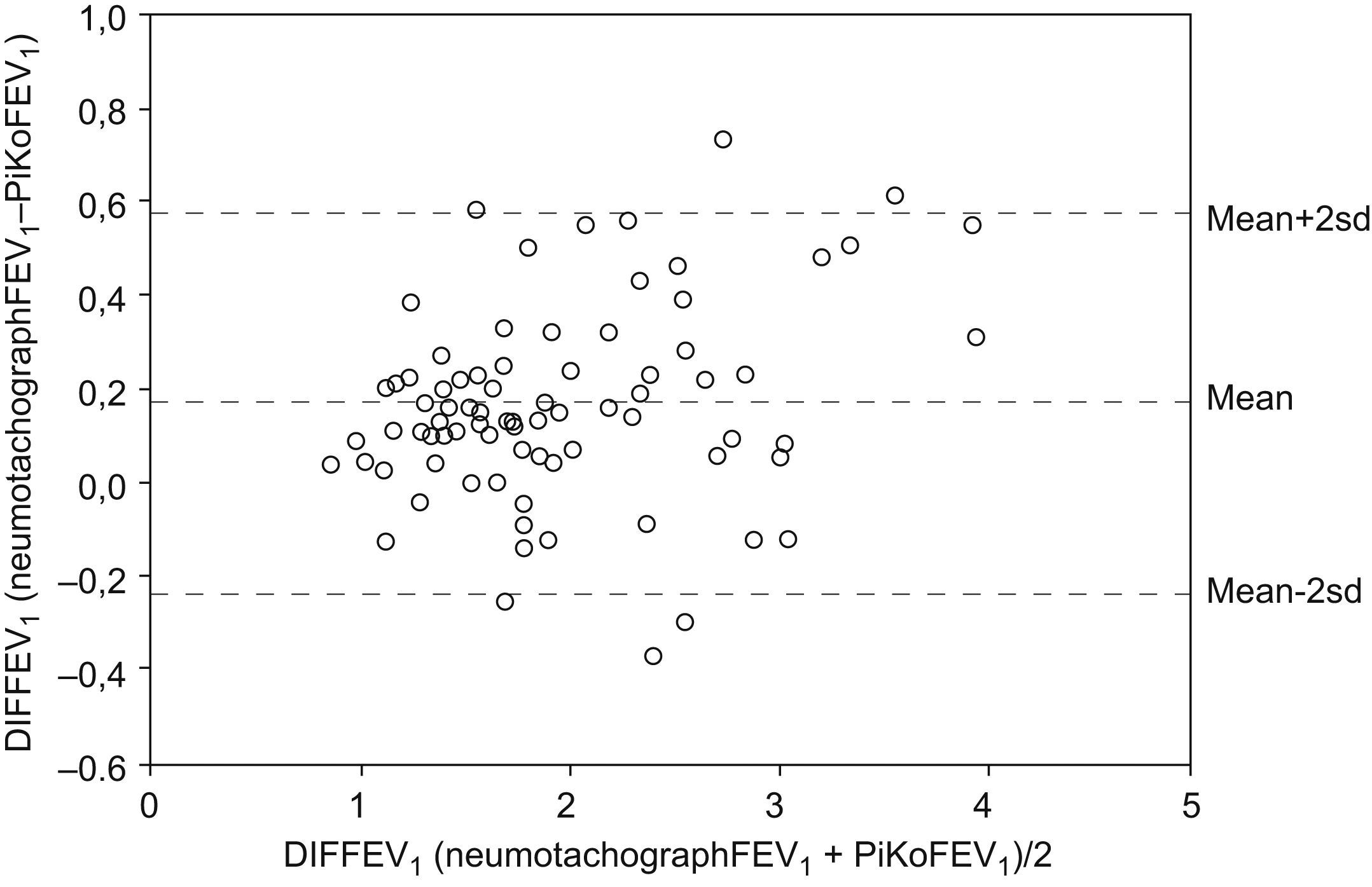
As a result, for analysis of the measurements we used the Bland-Altman method,9 which comprises the graphic representation of the mean difference between the two values. By applying this method we obtained a mean difference for PEF of 9.82 (95%CI: 2.43–17.21), versus 0.17 (95%CI: 0.12–0.21) for FEV1 – as can be seen in the Bland and Altman plot (Figs. 2 and 3, respectively).
The intraclass correlation coefficient was 0.96; (p<0.001; 95%CI: 0.93–0.97) for FEV1 and 0.93; (p<0.001; 95%CI: 0.89–0.95) for PEF.
DiscussionThe use of devices which measure PEF has decreased in recent years, probably as a result of the generalised incorporation of spirometry, which allows more precise diagnosis and better patient monitoring. Despite this situation, however, the evaluation of PEF retains its usefulness in the context of home monitoring, and in those cases where forced spirometry is not available, as a diagnostic tool in relation to the variability and assessment of bronchodilation or exertion response.10 Another application is the known classification of asthma severity according to the variability of PEF – this currently being the subject of debate following the recent publication of studies5 questioning its validity, despite this application being maintained in the national and international clinical guides.11,12
Thus, the possibility of using FEV1 outside the pulmonary function laboratory would offer a more precise measure of the true situation of the patient,7 facilitating more adequate treatment according to the needs of each individual subject. If, in addition, such FEV1 recordings are stored in the memory of the device, with the possibility of later downloading the data to a computer, it would become possible to assess monitoring compliance, which often constitutes a problem when interpreting the monitored period.13
According to the present study, the Piko-1® may be very useful for evaluating asthmatic patients. Although forced spirometry yields greater values for both FEV1 and PEF, the intraclass correlation coefficient obtained indicates excellent reliability – allowing use of the device under the aforementioned conditions.
One way to obtain a more exact assessment of the condition of the patient involves the introduction of the best personal value – obtained through successive measurements with the Piko-1® – as reference value.14
The mentioned differences in the values obtained may be influenced by a number of factors, including for example the sequence used in performing the tests. The selected patients were asthmatic children seen in the clinic for assessment of the course of their illness. With the purpose of not interfering with this assessment, we first performed forced spirometry, followed by use of the Piko-1®. This test sequence could have resulted in lower values with the Piko-1®, due to patient tiredness or demotivation after forced spirometry. However, in the first international paper comparing FEV1 and PEF spirometric and Piko-1 measurements in adults in which 50% performed first forced spirometry and 50% Piko first used to obtain the values of FEV, and PEF, there were no relevant differences between measurements from both devices.15
It must also be taken into account that in seeking the best possible result for patient evaluation, we allowed as many as eight forced spirometry attempts in accordance with the ATS norms, but only three attempts with the Piko-1®.
On the other hand, the use of animation devices with the spirometer in performing the expiration manoeuvre may represent an incentive that results in better values as a consequence of greater patient effort and concentration.16
Despite the observed differences, the Piko-1® appears to be a reliable alternative for the evaluation of asthma in those situations where forced spirometry is not available. In this line, a recent study in Spain involving 40 adults seen in the clinic for pulmonary function tests recorded FEV1 and PEF values with the Piko-1® which also showed good concordance with the values obtained by forced spirometry.17
Financial supportNo external financial support has been received for the present study.