INTRODUCTION
Hydroxychloroquine (HXQ) sulphate is a synthetic antimalarial drug, widely used in rheumatology due to its immunosuppressive properties. Antimalarials are well known to cause adverse reactions, cutaneous and ocular side effects being the most frequently described problems. The most common cutaneous adverse reaction is skin pigmentation. Delayed-type sensitization to HXQ is rare. Contact dermatitis 1, fatal toxic epidermal necrolysis 2, acute generalized exanthematous pustulosis 3 and phototoxic and photoallergic dermatitis 4 have been reported. We present a case of type IV hypersensitivity to hydroxychloroquine with two different clinical patterns in the same patient.
CASE REPORT
A 47-year-old woman diagnosed with HLA B27 ankylosing spondylitis was treated with HXQ for 22 days. She discontinued the drug due to gastric intolerance. Five days later a generalized papulo-erythematous itchy cutaneous eruption developed, affecting the soles and palms, as well as typical target zones on the extensor surfaces of her arms. She had no mucosal lesions or other symptoms. No focus herpes simplex lesions or any sign or symptom of infection was identified.
She was diagnosed with erythema multiforme (EM) by her dermatologist and was referred to our Department for study. She was treated with systemic steroids and antihistamines, followed by complete resolution of the lesions without scales or residual pigmentation in 20 days.
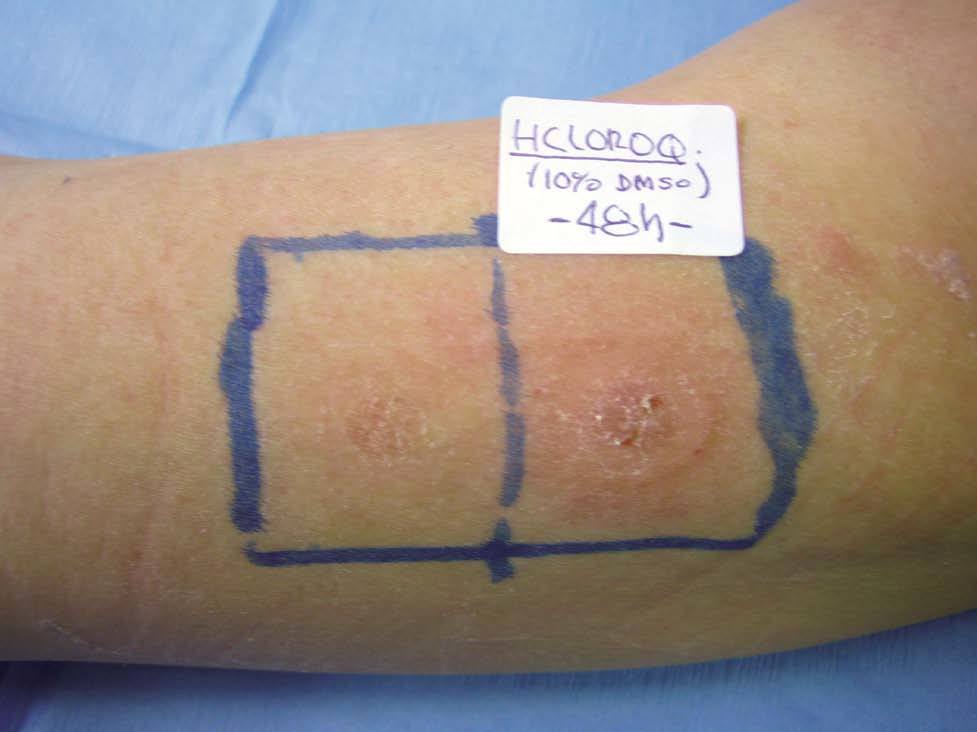
Patch testing with 10 % HXQ in DMSO proved positive at 48 and 96 hours (fig. 1) and negative in 5 control subjects. Eight days after patch testing, a generalized pruriginous erythematous papular exanthema developed without involvement of the soles or palms. Target lesions were not identified.
Figure 1.--Positive patch-test with hydroxychloroquine (10 % in DMSO) at 48 hs. At left side, negative result with DMSO.
A skin biopsy obtained during this second episode showed discrete irregular acanthosis, parakeratosis and spongiosis in the epidermis, and a perivascular inflammatory infiltrate with lymphocytes, mononuclear cells and eosinophils present in dermis.
Other frequent causes of EM were ruled out. The complete blood cell count and liver and renal function parameters were within normal limits. Serum antibodies to herpes simplex virus, adenovirus, Mycoplasma pneumoniae and histoplasma proved negative. Levels of C1q, C4, C2 and C3, circulating immune complexes, cryoglobulins and ANA antibodies were normal.
DISCUSSION
We report a case of delayed hypersensitivity to HXQ confirmed by patch testing and skin biopsy. Patch tests with HXQ have been found to be positive in a few cases reported in the literature. Meier et al 1 described a case of contact dermatitis and bronchial asthma due to HXQ with a positive patch test at concentrations of 0,1 %, 0,5 %, 1 % and 2 % (vehicle is not mentioned). Lisi et al 4 reported a positive photopatch test with 5 % HXQ sulphate in water solution in a case of photoallergic dermatitis. Despite of the diagnostic value and reduced risk of patch testing, it is poorly standardized for some drugs, few cases of hypersensitivity to them have been documented, and testing only exceptionally elicits generalized cutaneous reactions 5.
In our patient, the first cutaneous reaction corresponded to a generalized maculo-papular-erythematous rash, with typical target lesions, patognomonic of EM, and with an extensive and unusual distribution. On the other hand, patch testing elicited a systemic eczematous dermatitis. We thus report two different clinical patterns of delayed hypersensitivity in the same patient and with the same drug. Systemic contact-type dermatitis can presents as several clinical variants that includes eczematous eruption and EM 6: this therefore may reflect the wide clinical spectrum of the same immuno-pathological mechanism. To our knowledge, EM to HXQ has not been reported to date.
Correspondence:
P. Rojas Pérez-Ezquerra
Dr. Esquerdo, 46
28007 Madrid. Spain
E-mail: projasperezezquerra@hotmail.com