Latex has been recognized since the 1980s as an occupational hazard and, as latex products are used increasingly worldwide, there has been an increase in the number of reported cases.
Immediate-type hypersensitivity reactions to latex have been studied more frequently, because of their frequency and possibility of live threatening reactions1. In latex gloves the most common allergens for delayed-type hypersensitivity are the chemical additives, even though, since 1992 some cases have been reported of type IV allergy to pure natural rubber latex (NRL), associated or not to type I allergy2. Additionally, some recent prospective studies also confirmed the existence of type IV hypersensitivity to natural rubber latex, with a prevalence ranging from 1 %, in patients commonly referred for epicutaneous tests, to 6 %, in rubber glove users with chronic hand eczema3,4.
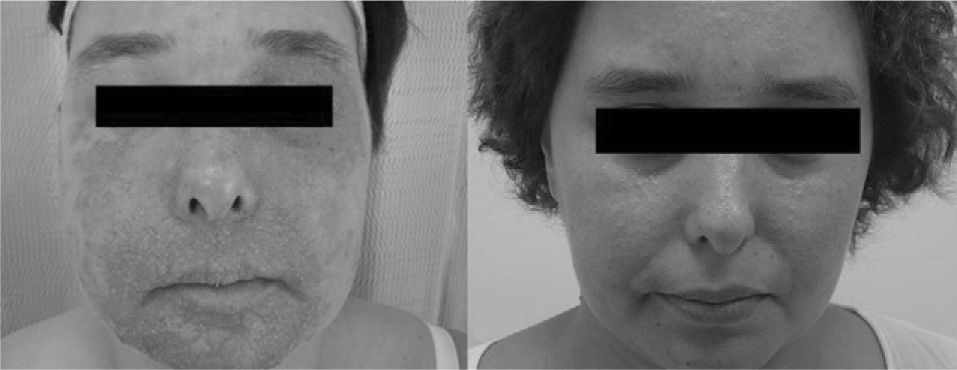
We present a case of a 32-year-old female patient, social caregiver. This patient was observed in our department in January 2006 due to a 9-month history of severe eczema, localized initially on the hands, and subsequently on her forearms, face and neck, which aggravated in relation with her professional activity and with peanut and chestnut ingestion (fig. 1a), with significant improvement on her holidays. She also complained of mild nasal and eye pruritus, mucous rhinorrhea, nasal obstruction and sneezing attacks aggravated in the workplace. The patient's personal background included a history of mild persistent allergic rhinitis since childhood.
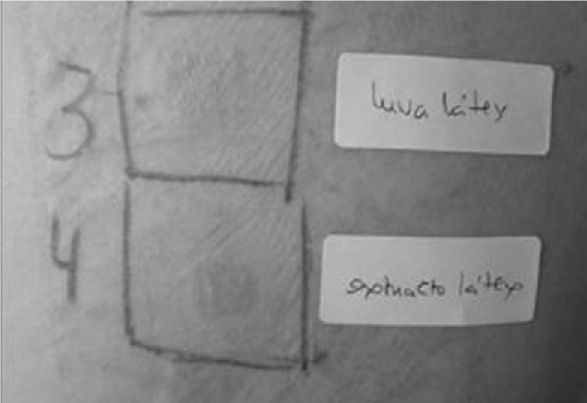
Patch tests were positive to NRL extract (glycerin 50 % and phenol 0.3 % ALK-Abelló™) and to patient's own rubber gloves (fig. 2) and negative to standard and rubber additives series. Skin prick-tests with aeroallergens were positive to latex, grass-pollen and olive, and skin prick-tests with foods were positive to peanut, chestnut and avocado. The laboratory evaluation documented: total IgE of 13545 UI/mL; specific serum IgE quantification positive to latex (> 100 kUA/L), grass-pollen (> 100 kUA/L), olive (9,83 kUA/L), peanut (0,46 kUA/L), chestnut (0,67 kUA/L) and avocado (1,18 kUA/L); and rHev b2 (24,0 kUA/L), rHev b5 (> 100 kUA/L), rHev b6.01 (44,2 kUA/L), rHev b6.02 (50,3 kUA/L), and rHev b11 (24,0 kUA/L). It was also demonstrated by enzyme immunoassay method (FITkit-Quattromed™) that the gloves used by the patient at the workplace had a high allergenic content: Hev b1: 0.11μg/g; Hev b3: 0.59μg/g; Hev b5: 2.03μg/g; Hev b6.02: 1.07μg/g; total: 3.80μg/g.
It was diagnosed latex allergy of professional aetiology, associated to latex-fruit syndrome. Patient initiated sublingual immunotherapy for latex (ALK-Abelló™) and was advised to avoid contact with latex. After 6months of therapy, the dermatosis completely improved and she reassumed her professional activity, maintaining latex restriction measures - the patient uses latex free gloves and her colleagues non-powdered latex gloves (fig. 1b).
We underline the importance of this case for the exuberance of the initial clinical presentation and for the coexistence of manifestations mediated by immediate and delayed hypersensitivity to natural rubber latex. Although this coexistence is not common, it may cause diagnostic difficulties. Hence we suggest that, in cases of glove dermatitis, standardized NRL should be used routinely in a patch-test and skin-prick test, in addition to patch-tests with rubber chemicals.
In the above case it was also evident a cross-sensitivity between latex and two fruits: chestnut and peanut, as already described in the literature5. The finding of a high allergen concentration in the patient's own glove is of concern and alerts to the necessary recommendations for the rubber industry and regulatory health authorities on the use of low-protein gloves and powder-free latex gloves.
This case also suggests that specific immunotherapy with latex, recently at our disposal6, can be a suitable therapeutic option in some of these patients.