INTRODUCTION
Fixed Drug Eruptions (FDE), first described by Brocq, in 1894, consists of recurrent eruptions that can affect any part of the skin and/or mucous membrane, characterized by sharply marginated, round, erythematous to violaceous plaques which vary in size, occurring after ingestion of the offending drug 1-3. Vesicles and bullae with crusting may develop subsequently 4. Generalized bullous fixed drug eruption is a rare and severe condition that requires differential diagnosis with toxic epidermal necrolysis and bullous pemphigoi d5.
The diagnostic hallmark is its recurrence at previously affected sites with repeated ingestion of the suspected drug 2,3. When the acute phase subsides, there is usually residual hyperpigmentation that becomes more pronounced after each recrudescence 4.
FDE are common cutaneous drug reactions, frequently misdiagnosed, occurring in all ages, although more commonly in young adults 4. They are responsible for 10 % of all adverse drug reactions 6.
It is currently known that many drugs can cause FDE, but some seem to be more frequent. The most common implicated drugs are antibiotics, namely sulfonamides, and nonsteroidal anti-inflammatory drugs (NSAIDs) 1,2,7.
To our knowledge, there are only eight cases of FDE induced by nimesulide reported in the literature 8,9.
CASE REPORT
We report a case of a 41-year old healthy male referred to our Drug Allergy Clinic for several episodes of urticaria and lip swelling after drug ingestion.
He reported 2 episodes of urticarial rash on the lower back and legs and swelling of the lips, 12 hours after oxatomide ingestion (30 mg). One year later, a similar episode occurred, this time with a predominant lesion on the right leg, after ingestion of cefixime (400 mg), nimesulide (100 mg) and paracetamol-caffeine-brompheniramine association. All the episodes resolved spontaneously after drug withdrawal.
In order to assess alternative treatment options skin prick tests (SPT) and intradermal tests (IDT) were performed with hydroxyzine and promethazine. SPT were negative and IDT were positive to both drugs at 1/10 dilution (5 mg/ml and 2,5 mg/ml, respectively). Patch tests with oxatomide were negative. Single-blind placebo controlled oral challenge (SBPCOC) with increasing doses of an alternative antihistamine, desloratadine (cumulative dose of 10 mg), was well tolerated.
Five months later, he returned to our clinic with a circular, well limited, violaceous, nodular, non pruritic lesion on the right leg (fig. 1), approximately 18 hours after ingesting nimesulide (100 mg) and clarithromycin (500 mg), prescribed for acute pharyngitis. He stopped both drugs but 48 hours later developed serious lesion vesiculation (fig. 2) that resolved in 3 weeks.
Figure 1.--Recurrent lesion after drug intake, suggesting nimesulide-induced fixed drug eruption.
Figure 2.--Vesiculated lesion.
When specifically asked about lesion recurrence, the patient recalled that he also had a predominant round lesion on the lumbar region each time he ingested oxatomide, that he underestimated.
SPT and IDT with clarithromycin were negative.
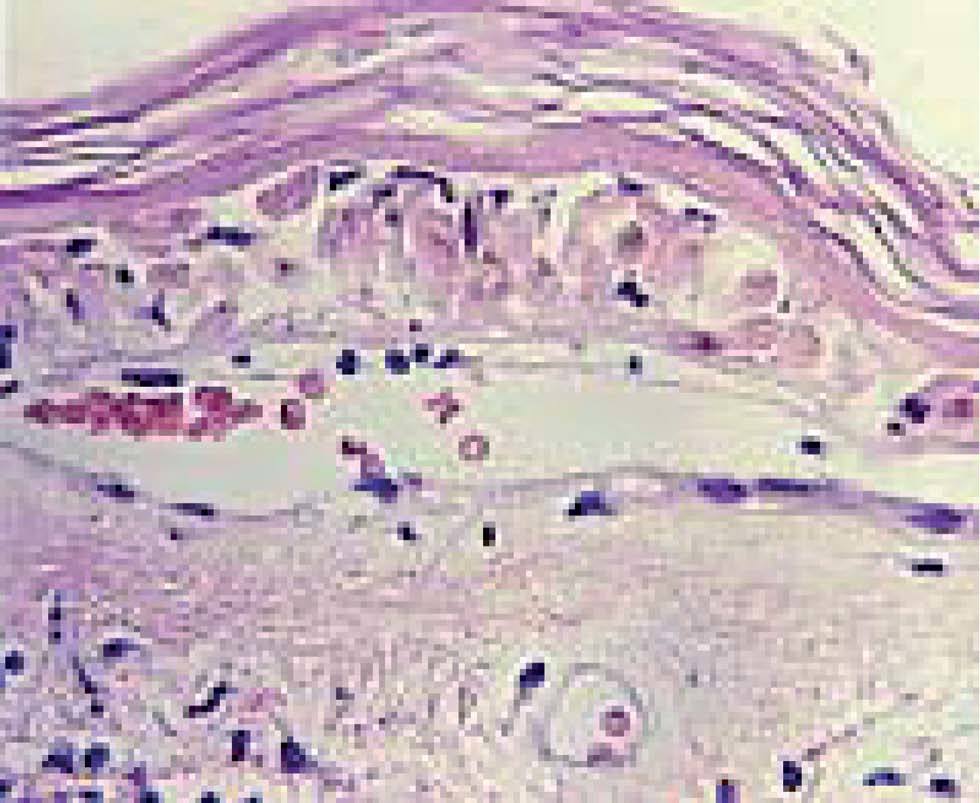
Skin biopsy performed 2 weeks after the onset of the lesion revealed histological findings consistent with epidermal necrolysis (fig. 3).
Figure 3.--Skin biopsy suggesting epidermal necrolysis.
Patch tests (10 % in pet.) on residual pigmented skin, performed 2 months after the onset of the lesion, were positive (48h) to nimesulide (+ + +) (Aulin®, Donulide®) and paracetamol-caffeine-brompheniramine association (+) (Ilvico®) (fig. 4). Control patch tests on unaffected skin were negative.
Figure 4.--Positive patch testing on residual lesion.
SBPCOC with increasing doses of an alternative NSAID, meloxicam, up to 15 mg, was carried out with good tolerance.
Nowadays, he maintains residual hyperpigmentation and avoidance of the culprit drugs.
DISCUSSION
As in most cases, the causative agent was identified from the patient history, lesion recurrence on the previously affected site after re-exposure to the suspected drug(s) and positive patch testing on residual lesions 3,10.
Oral challenge with suspected drugs were not performed considering that the patient presented a bullous form of FDE with a risk of developing a generalized and severe reaction. According to some authors, although re-challenge remains the most reliable diagnostic method, topical provocation on sites of previous lesions has been increasingly adopted, as it is a simple, fast and safe alternative to oral challenge 10,11.
The positivity of patch tests to paracetamol-caffeine-brompheniramine association could be explained by the fact that this patient also had antihistamine hypersensitivity.
Thereby, what we initially thought to be an urticarial reaction to antihistamine could, in fact, be a FDE, considering that there was a predominant lesion on the lumbar region each time the patient ingested oxatomide. The patient only referred this predominant lumbar lesion after we suspected that the lesion on his leg was a FDE, and specifically asked him about lesion recurrence.
SPT and IDT with oxatomide were not performed, once in our Country there is not any parenteral formulation available. Patch tests with this drug were negative probably because they were performed on unaffected skin. The patient refused to perform patch tests with oxatomide on the residual lesion on the lumbar region, since he already had an alternative antihistamine.
Sensitization to several drugs is not frequent 12. When it occurs, lesions have a preferential localization related to each of the implicated drugs, recurring at one specific site everytime that drug is taken 6.
Treatment consists of drug discontinuation. Lesions usually fade within one week, but increased pigmentation may remain for months. Typically, corticosteroid treatment is not required. However, in the generalized bullous form of the disease, topical corticosteroids, systemic antimicrobial agents and antihistamine may be necessary 3.
In conclusion, this seems to be a bullous form of FDE, induced by nimesulide, and eventually by oxatomide.
We believe it is important that physicians be aware that although common, FDE are frequently misdiagnosed, and that a detailed anamnesis and physical examination are key to suspect this condition.