Wheezing is a very common respiratory symptom in infants. The prevalence of wheezing in infants, conducted in developed countries shows prevalence rates ranging between 20% and 30%. However, we do not know the risk factors in our population of wheezing infants.
MethodsA standardised written questionnaire (WQ-P1-EISL) in infants between 12 and 18 months of age residing in the city of Cordoba was used; population/sample included 1031 infants. Recurrent wheezing (RW) was defined as three or more episodes of wheezing reported by the parents during the first 12 months of life. Data obtained were coded in Epi-Info™ (version 7) and statistically analysed with SPSS (version 17.5) software in Spanish. Parametric tests (one-way ANOVA) were performed for identifying significantly associated variables.
ResultsThe prevalence of wheezing infants was 39.7%; recurrent wheezing 33%; and severe wheezing 14.7%; 13.7% had pneumonia before the first year and of these 6.3% were hospitalised, multiple variables as risk factors for wheezing were found such as: >6 high airway infections and bronchiolitis in the first three months of life, smokers who smoke in the home among other risk factors and protective factors in those who have an elevated socioeconomic status.
ConclusionIt is known that persistent respiratory problems in children due to low socioeconomic status is a risk factor for wheezing, pneumonia and could be a determining factor in the prevalence and severity of RW in infants. Research suggests that there are areas for improvement in the implementation of new educational strategies.
Wheezing constitutes a common respiratory symptom in infants, its causes are numerous and respond to different conditions in the lower respiratory tract; they have a significant impact on the quality of life for affected children and their families; produce a significant increase in the use of health resources, regardless of the cause, and have a high economic and social cost, especially recurrent episodes. It is called recurrent wheezing (RW) when three or more episodes occur during twelve consecutive months and are a frequent cause of paediatric consultation and an important challenge for public health worldwide. In most cases, the initial events occur in the first year of life.1
Several risk factors have been associated with the prevalence of RW and its severity, especially virus respiratory infections. In Latin America, about 100,000 children die in the first year of life from acute respiratory infections (2008–2010), and a significant proportion of them have a history of wheezing in the first year.2 In Argentina, lower respiratory infections (LRI) are the third leading cause of death in children under one year.3 Recent studies have shown it is a growing cause of emergency room visits in Argentina.4 New evidence suggests that the genetic background could be altered by exposure to environmental risk factors, even biological ones, in the first three months of life.5,6 Children born by Caesarean section have less diversity in their intestinal microbiota during their first two years of life than those born vaginally. Intestinal microbiota bacteria are essential to the development of the immunological system, and its alteration has been linked to asthma.7
A history of familial asthma, especially maternal or paternal, significantly increases the risk of wheezing as well as premature birth, low birth weight; siblings in the household, attending kindergarten, early weaning, and exposure to cigarette smoke during pregnancy and, in the postpartum period, low socioeconomic status and low parental level of education.8,9
Population studies assessing prevalence of wheezing in children are scarce, and have methodological differences that make it impossible to compare them. Although, for several years, in different parts of the world, work has been ongoing to define the risk factors and classification of phenotypes or groups of wheezing infants. The first data on the natural history of wheezing in early childhood were obtained by retrospective review of medical records or the use of questionnaires and, therefore, the data were at risk of being partial. To avoid these biases, prospective randomised studies have been launched. The first multicentre study designed for this purpose was the International Study of Wheezing in Infants (EISL), involving Latin American countries (Chile, Brazil, Ecuador and Colombia) as well as Spain and the Netherlands. Validated questionnaires were used to obtain data that elucidate and compare situations involving wheezing in infants.10 While most risk factors are common in Latin America and Europe, their impact on public health can be very different. Avoiding nurseries and smoking during pregnancy; promoting breastfeeding for more than three months and improving the education of the mother, would have an important role in reducing its prevalence worldwide.11
Materials and methodsSubjects and sampling frameThe standardised written questionnaire (WQ-P1-EISL)12 was administered to the parents or guardians of infants who consecutively attended the vaccination centres for routine immunisation (National Vaccination Schedule) and agreed to complete the questionnaire, from August 1, 2013, to March 31, 2014. The children were aged between 12 and 18 months old and were resident in the city of Córdoba, Argentina. The questionnaires were administered in the vaccination centres of the following hospitals: Children (in the southeast of the city of Córdoba), Misericordia Hospital (southwest), Paediatric Hospital (north), and two private vaccination centres (northeast) to compare different socioeconomic strata.
Wheezing was defined as an affirmative response to the question, “Has your child had wheezing or wheezed during the first 12 months of his/her life?” Recurrent wheezing (RW) was defined as three or more episodes of wheezing reported by the parents during the first 12 months of life.
Data obtained were coded in Epi-Info™ (version 7) and statistically analysed with SPSS (version 17.5) software in Spanish. Parametric tests (one-way ANOVA) were performed and then for identifying significantly associated variables we applied the Backward Stepwise multiple regression. A probability (p) of 0.05 was set. Odds Ratio was used to assess the protection or risk factors.
Subgroups in the studyThe wheezing infants were divided into groups according to the frequency of episodes of wheezing: Group 1, one or two wheezing episodes (hereinafter occasional wheezing, OW); Group 2, three to five wheezing episodes (recurrent wheezing or RW); and Group 3, six or more wheezing episodes (severe recurrent or SW). Those who never had a wheezing episode were designated no wheezing (NW).
Ethical approvalThe study was approved by the Ethics and Scientific Committee at each local health centre, and by the Board of Ethics Assessment and Health Research (CoEIS) and the Ethics in Health Institutional Committee (CIEIS) of the province of Córdoba and the parents and guardians who answered the questionnaire after signing the written consent with full knowledge of the study.
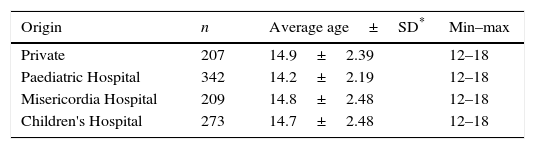
Results1091 parents of children aged 12–18 months were surveyed. 60 questionnaires belonging to children who came from other localities were excluded. Therefore, the final sample consisted of 1031 questionnaires. They were completed by the mother, 95.4% (n=984); father, 3.4% (n=35); others, 1.2% (n=12); and overall response rate was 94.5%. Of the 1031 children evaluated, 531 (51.5%) were male. The number of participants for each centre and ages in months are shown in Table 1.
Centre of origin and age of the cases analysed.
| Origin | n | Average age±SD* | Min–max |
|---|---|---|---|
| Private | 207 | 14.9±2.39 | 12–18 |
| Paediatric Hospital | 342 | 14.2±2.19 | 12–18 |
| Misericordia Hospital | 209 | 14.8±2.48 | 12–18 |
| Children's Hospital | 273 | 14.7±2.48 | 12–18 |
A total of 409 children (39.0%) had one or more episodes of wheezing in the first 12 months and the average age of onset was 4.47±2.96 (range: 1–12 months). Of these, 214 children (52.3%) were occasional wheezing (OW), 135 (33%) were recurrent wheezing (RW), and 60 (14.7%) were severe wheezing (SW).
When the prevalence of SW was evaluated, it was observed that at the Paediatric Hospital it was 8%; at the Children's Hospital 8.8%; Misericordia Hospital 0.9%; and Private Centres 2.9%.
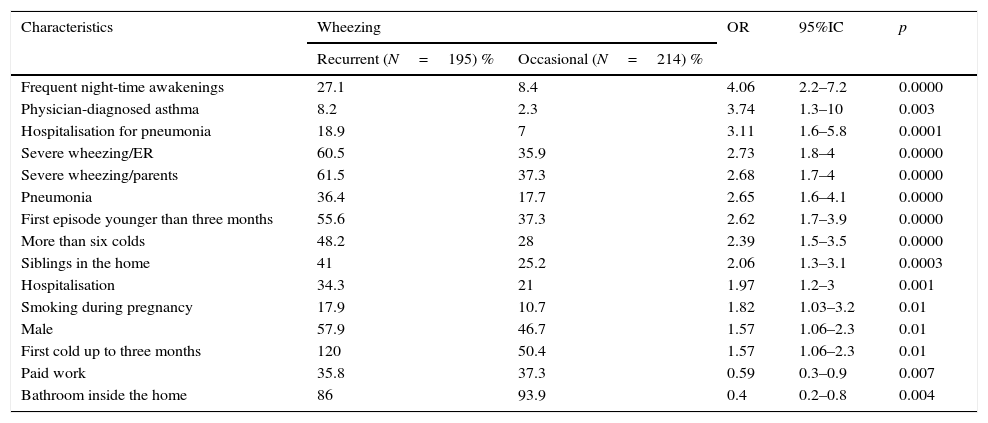
There was an independent association between RW and OW. After bivariate analysis, factors significantly associated with recurrence are shown in Table 2.
Identified significant demographic factors and health characteristics of wheezing infants (n=409), according to the development of recurrent wheezing. Results of Bivariate analysis.
| Characteristics | Wheezing | OR | 95%IC | p | |
|---|---|---|---|---|---|
| Recurrent (N=195) % | Occasional (N=214) % | ||||
| Frequent night-time awakenings | 27.1 | 8.4 | 4.06 | 2.2–7.2 | 0.0000 |
| Physician-diagnosed asthma | 8.2 | 2.3 | 3.74 | 1.3–10 | 0.003 |
| Hospitalisation for pneumonia | 18.9 | 7 | 3.11 | 1.6–5.8 | 0.0001 |
| Severe wheezing/ER | 60.5 | 35.9 | 2.73 | 1.8–4 | 0.0000 |
| Severe wheezing/parents | 61.5 | 37.3 | 2.68 | 1.7–4 | 0.0000 |
| Pneumonia | 36.4 | 17.7 | 2.65 | 1.6–4.1 | 0.0000 |
| First episode younger than three months | 55.6 | 37.3 | 2.62 | 1.7–3.9 | 0.0000 |
| More than six colds | 48.2 | 28 | 2.39 | 1.5–3.5 | 0.0000 |
| Siblings in the home | 41 | 25.2 | 2.06 | 1.3–3.1 | 0.0003 |
| Hospitalisation | 34.3 | 21 | 1.97 | 1.2–3 | 0.001 |
| Smoking during pregnancy | 17.9 | 10.7 | 1.82 | 1.03–3.2 | 0.01 |
| Male | 57.9 | 46.7 | 1.57 | 1.06–2.3 | 0.01 |
| First cold up to three months | 120 | 50.4 | 1.57 | 1.06–2.3 | 0.01 |
| Paid work | 35.8 | 37.3 | 0.59 | 0.3–0.9 | 0.007 |
| Bathroom inside the home | 86 | 93.9 | 0.4 | 0.2–0.8 | 0.004 |
N=number of subjects; OR: Odds ratio; 95%CI: 95% confidence interval; ER: Emergency Room.
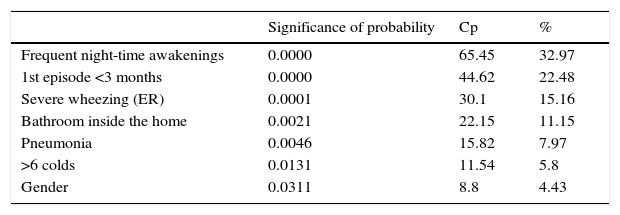
After multivariate analysis and multiple regression, the variables that maintained significance are shown in Table 3.
Multiple stepwise regression of recurrent wheezing.
| Significance of probability | Cp | % | |
|---|---|---|---|
| Frequent night-time awakenings | 0.0000 | 65.45 | 32.97 |
| 1st episode <3 months | 0.0000 | 44.62 | 22.48 |
| Severe wheezing (ER) | 0.0001 | 30.1 | 15.16 |
| Bathroom inside the home | 0.0021 | 22.15 | 11.15 |
| Pneumonia | 0.0046 | 15.82 | 7.97 |
| >6 colds | 0.0131 | 11.54 | 5.8 |
| Gender | 0.0311 | 8.8 | 4.43 |
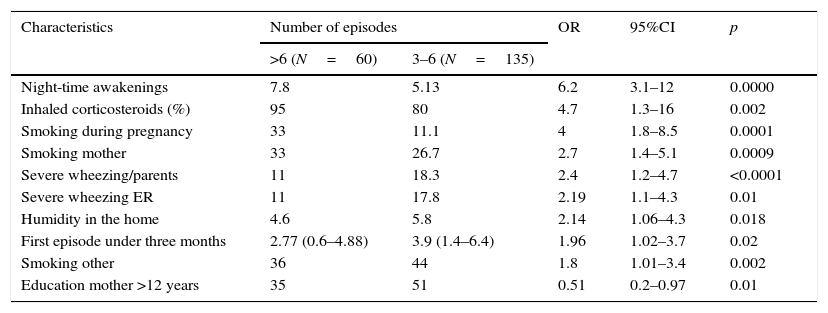
To identify those factors associated with severity of wheezing, we compared RW with SW infants and Table 4 shows that significantly related (univariate analysis).
Identified significant characteristics of recurrent wheezing infants according to the frequency of acute episodes in the first year – results of univariate analysis.
| Characteristics | Number of episodes | OR | 95%CI | p | |
|---|---|---|---|---|---|
| >6 (N=60) | 3–6 (N=135) | ||||
| Night-time awakenings | 7.8 | 5.13 | 6.2 | 3.1–12 | 0.0000 |
| Inhaled corticosteroids (%) | 95 | 80 | 4.7 | 1.3–16 | 0.002 |
| Smoking during pregnancy | 33 | 11.1 | 4 | 1.8–8.5 | 0.0001 |
| Smoking mother | 33 | 26.7 | 2.7 | 1.4–5.1 | 0.0009 |
| Severe wheezing/parents | 11 | 18.3 | 2.4 | 1.2–4.7 | <0.0001 |
| Severe wheezing ER | 11 | 17.8 | 2.19 | 1.1–4.3 | 0.01 |
| Humidity in the home | 4.6 | 5.8 | 2.14 | 1.06–4.3 | 0.018 |
| First episode under three months | 2.77 (0.6–4.88) | 3.9 (1.4–6.4) | 1.96 | 1.02–3.7 | 0.02 |
| Smoking other | 36 | 44 | 1.8 | 1.01–3.4 | 0.002 |
| Education mother >12 years | 35 | 51 | 0.51 | 0.2–0.97 | 0.01 |
N=number of subjects; OR: Odds ratio; 95%CI: 95% confidence interval; ER: Emergency Room.
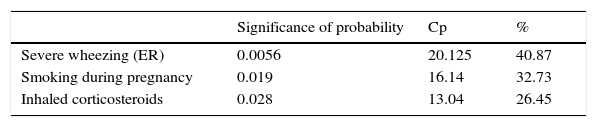
After multivariate analysis and multiple regression, the variables that maintained significance with respect to severity are shown in Table 5.
DiscussionGenetic and environmental factors have been suggested as risk factors and protection for wheezing in early life. The identification of these factors, in this age group, is crucial for a better understanding of the different wheezing phenotypes in relation to the development and progression of asthma.13
The first multicentre study on the prevalence of recurrent wheezing during the first year of life (EISL) showed a high prevalence, with a high variability of the risk factors. This variability occurs among the participating countries and also within the same country, with lower prevalence and severity in European centres than in Latin American, which suggests that the influence of regional or local environmental/ecological factors could explain the magnitude of the effect of these factors in relation to risk/protection.10,11
According to the EISL study, the prevalence of recurrent wheezing in the first 12 months of life varies between Mérida (Mexico) 2.3% and Porto Alegre (Brazil) 36.3%, with an average of 21.4% for Latin America and Europe 15%.14 The prevalence for the city of Córdoba in our study was 18.9%.
Among the socio-demographic factors, male gender was a risk factor studied. Garcia-Marcos et al.,15 as well as others5,6,16–18 showed that male gender was a risk factor for RW during the first months or years of life and that the risk was higher in Europe than in Latin America. In our study, however, it was a risk factor only in recurrent wheezing in children but not in occasional wheezing, nor in severe wheezing in the multivariate analysis. A similar finding was observed in another study.19
Having presented six or more episodes of upper respiratory tract infections in the first year of life, especially with the emergence within three months of life of the first cold (OR=2.03), was a factor to suffer occasional wheezing and/or recurrent wheezing in 2319 children under two years of age.20 We determined that it was a risk factor associated with wheezing in both occasional wheezing and recurrent wheezing (Table 2), but could not find such an association in severe wheezing. The presence of at least one sibling was associated with recurrent wheezing in the bivariate analysis and could be, in part, an explanation of the early onset of these infections and eventual cause of recurrent wheezing, but it was not a risk factor for severe wheezing.
The results of the Tucson Cohort Study indicated that exposure to one or older siblings or childcare assistance within the first six months was a risk factor for frequent wheezing during the first two years of life, but such exposure protected them from asthma and frequent wheezing in children (6–13 years).21 This association was also observed in children 6–59 months living in São Paulo.22 Benicio et al. found in a bivariate analysis that living in homes with four or more people was associated with wheezing, but it was not an independent risk factor after adjusting for potential factors in the multivariate analysis, contrary to what was observed in the Tucson Study.
We note that in the province of Córdoba the average population per household is 3.2 people, according to the 2010 census.23 In our study, we only found an association with RW when there were siblings in the home, but we found no statistically significant association in the number of people per household or kindergarten attendance; but it could have to do with bias, as only 122 (11.8%) of the children surveyed were attending kindergarten.
Respiratory infections of the lower airways (LRTI) especially those caused by tRSV and rhinovirus have been associated with wheezing in childhood, although early infection in the later development of asthma is less clear.24 The EISL study showed a significant association between LRTI and wheezing in infants15 as well as other studies that have shown its association with asthma.25 In our study we found that having an infection (“bronchiolitis”) in the first three months of life, according to the bivariate analysis, is a risk factor for RW and SW. We also determined that having had pneumonia (prevalence: 13.7%) is a risk factor for occasional wheezing and RW, although it is not for SW, both in bivariate and multivariate analyses (Tables 2 and 3). Having been hospitalised for this condition is also a risk factor for OW and RW. In a Brazilian study26 it was shown that pneumonia and having been hospitalised for it is associated independently with RW and SW. In a cohort of new-borns of low socioeconomic status in Santiago (Chile) done during the first year of life, it was determined that the presence of recurrent wheezing in the first three months of life had a strong association with the diagnosis of pneumonia.6
Another variable studied was exposure to second-hand smoke during pregnancy and exposure after birth. Exposure to cigarette smoke, both prenatal and postnatal, is associated with the risk of wheezing in infants and preschool children in different studies,14,16,27 as well as in adolescence.28 In a meta-analysis, it was shown that prenatal and/or postnatal exposure increases the risk of wheezing incidence between 30% and 70%, especially in children under two years old.29 We have demonstrated that maternal smoke (smoke during and after pregnancy) and living with other smokers are risks factors for OW as well as SW. In the case of RW we found an association only with tobacco exposure during pregnancy.
When we analysed infants according to the severity of their wheezing, variables such as visits to the emergency ward, severe crisis perceived by parents, admissions for wheezing, physician-diagnosed asthma and frequent night-time awakenings were risk factors for RW; and that the use of inhaled corticosteroids, night-time awakenings, visits to the emergency room and severe SW crises.
When we evaluated the type of housing in the provincial capital, 95% of households had an indoor bathroom23; in our population, 92.7% of respondents had that convenience. Having a bathroom inside the home for the sibilant was a protective factor OR=0.55 (0.3–0.8), p=0.006; likewise for RW, OR=0.4 (0.2–0.80), p=0.004. This finding agrees with that reported by Mallol et al.6 with regard to the increased prevalence of wheezing in lower socioeconomic strata.
The present study had limitations related to the cross-sectional design thereof and any errors that arise when surveying parents. The strength of it is due to the attachment to the methodology used in other centres and the high response rate, allowing for the comparison of our results with those of other centres, even with very different cultural and social contexts. However, differences in the prevalence and severity of RW in infants within and between cultures are probably due to complex multifactorial gene–environment interactions that are distinctive for each locality and abilities to modulate the responses of the airways from early in life to adulthood.14
ConclusionsIn the present study the prevalence of wheezing was lower than expected in relation to the average in Latin America. We noted the same with severity; however, the prevalence of hospitalisation for wheezing was similar. It is known that persistent respiratory problems in children due to low socioeconomic status is a risk factor for wheezing, pneumonia and could be a determining factor in the prevalence and severity of RW in infants. Research suggests that there are areas for improvement in the implementation of new educational strategies and effective management of RW aimed at parents and healthcare personnel, which could reduce the prevalence of potentially fatal episodes, emergency room visits and hospital admissions, especially in patients with severe symptoms.
Finally, the results of our study should be considered by healthcare agencies to implement programmes that enable a systematic strategic approach to these major diseases in children.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.
The study has been self-financed and is part of the doctoral thesis by the principal author.