Although thousands of infants under the age of 12 months die each year from pneumonia in Latin America, little is known regarding the true occurrence of pneumonia, wheezing and other related respiratory illnesses in this age group.
Methods and resultsIn order to describe the prevalence and risk factors for radiologically confirmed pneumonia during the first year of life, a birth-cohort (n=188) of infants born in a low-income area in Santiago, Chile was followed up monthly.
ResultsThe prevalence of pneumonia during the first year of life was 13.3 % and there were no fatal events. Exclusive breastfeeding during the first 4 months of life was more prevalent in the non pneumonia group; conversely, wheezing episodes during 0-3 and 3-6 months of age, and hospitalization due to lower respiratory infection during 3-6 and 9-12 months of age were more prevalent in the pneumonia group. After a logistic multivariate analysis, the only risk factor that remained related with pneumonia was wheezing during the first 3 months of life (adjusted OR: 7.7, 95 CI: 1.32-44.92, p=0.024); while breastfeeding during the first 4 months was an independent protective factor for pneumonia (adjusted OR: 0.11, 95 CI: 0.03-0.44, p=0.002).
ConclusionThe significant protective effect of exclusive breast feeding against pneumonia in this cohort and the evident role of recurrent wheezing as risk factor for pneumonia during the first year of life support the implementation or reinforcement of public policies encouraging exclusive breastfeeding and an adequate management of wheezing since the first months of life.
Acute lower respiratory infection (ALRI) is one of the most common causes of morbidities and death among children1. Rates of pneumonia vary with age and are higher in children less than 2years old compared with older children2,3 and especially among the first six months of age4. Serious ALRI is more common and carries a higher mortality rate in children from developing populations than those in developed communities, e.g. specific mortality due to ALRI is 10 to 50 times higher in developing countries than in fully developed countries1,2,5–7.
Cross sectional studies have identified several risk factors that increase the likelihood and severity of ALRI such as younger children5,7, measles, malnutrition8, large families7,9 and environmental pollution10,11. Data obtained from community-based longitudinal studies have identified that male gender, low socio-economic status, mother with limited years of school, exposure to indoor air pollution, low birth weight, immunization status, not exclusively breastfeeding, attendance in child-care facility, having one or more siblings and crowding as additional risk factors for ALRI3,12,13.
Unfortunately, most community-based longitudinal studies have not focused on respiratory events occurring during the first year of life, when most of the morbidity and mortality due to ALRI occurs3,12,13. Although thousands of infants under the age of 12months die each year from pneumonia in Latin America1,14, little is known regarding the true occurrence of pneumonia, wheezing and other related respiratory illnesses in this age group13. A recent report from Chile found a high prevalence of wheezing (80.3 %) during the first year of life15, in contrast to developed countries where the prevalence ranges from 10 % to 42 %16–20. In the present study, we assessed the risk factors for radiologically confirmed pneumonia during the first year of life in a birth-cohort of infants from a low-income community in Santiago, Chile.
METHODSThis birth-cohort study was carried out in a low-income area in Santiago, Chile, where Hospital CRS El Pino is located, and where the vast majority of families earn the minimum salary (around USD $250 per month) and the mean parental educational level is 8 or less school-years. The methodology of this birthcohort was already published elsewhere15. Briefly, a random sample of 250 non-smokers mothers during their third trimester of pregnancy, monitored in the maternity outpatient clinic of El Pino Hospital were invited to participate in the study. Two hundred and twenty-five mothers accepted the invitation. From this group, only newborn babies who were 36 or more weeks of gestation and with a normal respiratory condition during the following 10days after delivery, were considered eligible for entry into the study and were scheduled to their first study visit at 1month of age. Two hundred and fifteen infants fulfilled the study inclusion criteria.
At the initial visit, demographic and environmental data were obtained and study visits were scheduled every month for 12months. During each scheduled visits, mothers were asked about their infants' health during the previuos 4weeks and a complete physical examination was performed by the study pediatrician. Infants were followed up at our outpatient clinic using an easy-access system that allowed their mothers to get direct contact with the study pediatricians and nurses in case of disease. Also, mothers were instructed and encouraged to bring their children to the outpatient clinic as soon as they started to have respiratory signs (e.g. sneezing, rhinorrhea, fever, cough, wheezing). Data regarding family history of atopy, breastfeeding, type of pregnancy and delivery, any illness occurred during the first year of follow up (i.e. viral upper respiratory infections or "colds" [URTI]-, acute bronchitis, pneumonia, acute otitis, wheezing episodes and eczema) were collected. Data on passive tobacco smoke exposure, crowding (defined as more than 3 persons over 2years of age sharing the bedroom with the infant, or more than one familial group sharing the household), parental education level, mother's employment status, pets at home, source of heating and cooking (gas, kerosene, wood, charcoal) were also obtained. Unfortunately, due to economical reasons, no etiological determinations for respiratory illnesses (including pneumonia) or cotinine measures for passive tobacco smoke exposure were made.
Infants were classified as having had pneumonia if the study pediatricians specified this diagnosis on the study form (sings of classic bacterial pneumonia with: fever, cough, tachypnea, respiratory distress and crackles on chest auscultation) and there was a radiographic evidence compatible with this diagnosis. X-ray criteria considered compatible with the diagnosis of pneumonia were the presence of alveolar infiltrates or lobar consolidation. Chest X-rays were not required in the study, and were ordered for clinical reasons only. Children with pneumonia who did not required hospitalization were followed-up daily by the same pediatrician. Infants were divided between those who had pneumonia and those who did not have pneumonia during the first 12months of life. The study was approved by the Hospital Ethics Committee and a written, signed and fully informed consent was obtained from parents.
Statistical analysisThe statistical analysis for differences between two groups (pneumonia or not) was done using Fisher and Chi-square test for categorical variables and Student t-test for continuous variables, respectively. A multivariate logistic regression model was performed, where pneumonia was the dependent variable, and those factors that became significant (p < 0.05) in the univariate analysis were taken as the independent variables. All the analysis was performed with STATA 7.0 statistical program (Stata Corp, College Station, TX).
RESULTSOf the 215 infants initially enrolled, 188 (98 females) completed the study. The main reasons for failure to completion were parents' relocation and parental unwillingness to continue with the study. The mean gestational age was 39.3 ± 1.9weeks, birth weight 3,468 ± 563g and birth length 50.7 ± 2.1cm.
From the whole cohort (188 infants), 163 (86.7 %) never had pneumonia and 25 (13.3 %) had pneumonia in the first year of life.
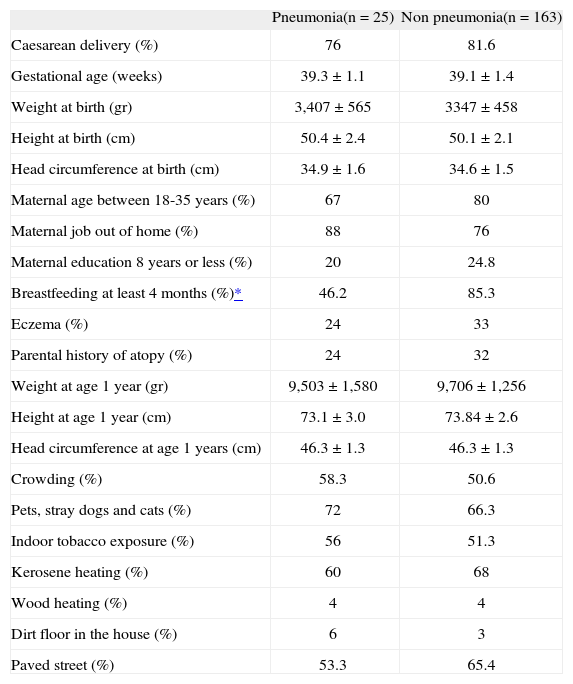
There was no significant difference in anthropometric parameters at birth and at the end of the first year of life or patient demographics between those children with or without pneumonia during the first year of life (table I). Infants who develop pneumonia were significantly less likely to be exclusively breastfed during the first 4months as compared to those who were not (46.2 % vs. 85.3 %, p = 0.001, respectively). There were more males than females in the pneumonia group, although the difference did not reach statistical significance (16.9% vs. 8.5%, p = 0.09, respectively). No differences between groups were found with respect to tobacco smoke exposure, indoor pollution, pets at home, crowding, dirt floor in the house and paved street (table I). Approximately one third of the episodes of pneumonia required hospitalization (8/25 events) and there were no fatal events.
Demographic characteristics of infants with or without pneumonia during the first year of life*
| Pneumonia(n = 25) | Non pneumonia(n = 163) | |
| Caesarean delivery (%) | 76 | 81.6 |
| Gestational age (weeks) | 39.3 ± 1.1 | 39.1 ± 1.4 |
| Weight at birth (gr) | 3,407 ± 565 | 3347 ± 458 |
| Height at birth (cm) | 50.4 ± 2.4 | 50.1 ± 2.1 |
| Head circumference at birth (cm) | 34.9 ± 1.6 | 34.6 ± 1.5 |
| Maternal age between 18-35years (%) | 67 | 80 |
| Maternal job out of home (%) | 88 | 76 |
| Maternal education 8years or less (%) | 20 | 24.8 |
| Breastfeeding at least 4months (%)* | 46.2 | 85.3 |
| Eczema (%) | 24 | 33 |
| Parental history of atopy (%) | 24 | 32 |
| Weight at age 1year (gr) | 9,503 ± 1,580 | 9,706 ± 1,256 |
| Height at age 1year (cm) | 73.1 ± 3.0 | 73.84 ± 2.6 |
| Head circumference at age 1years (cm) | 46.3 ± 1.3 | 46.3 ± 1.3 |
| Crowding (%) | 58.3 | 50.6 |
| Pets, stray dogs and cats (%) | 72 | 66.3 |
| Indoor tobacco exposure (%) | 56 | 51.3 |
| Kerosene heating (%) | 60 | 68 |
| Wood heating (%) | 4 | 4 |
| Dirt floor in the house (%) | 6 | 3 |
| Paved street (%) | 53.3 | 65.4 |
Numbers were expressed in mean ± SD or percentage.
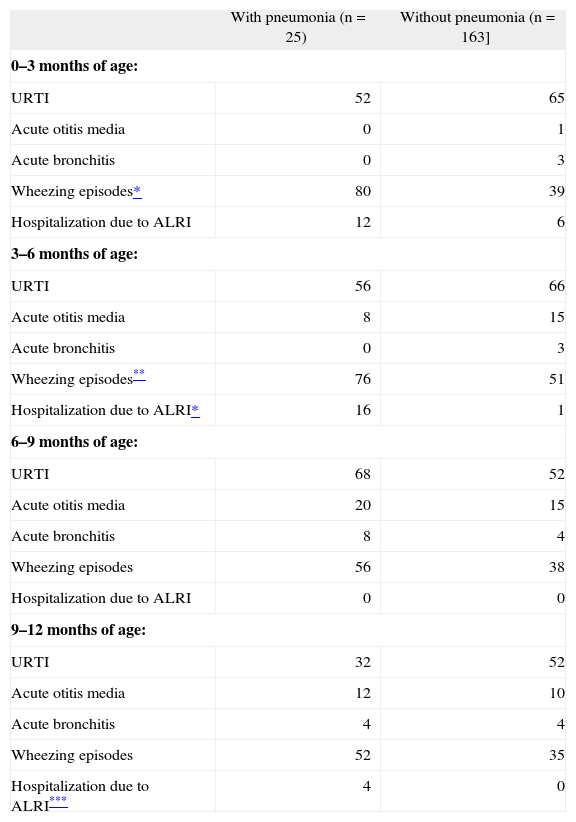
No differences between infants with and without pneumonia were found with respect to previous episodes of URTI, acute otitis media and acute bronchitis (table II). However, the proportion of infants who had wheezing during the first 6months of age was significantly higher in the group with pneumonia as compared to the one without pneumonia (0–3months: 80 % vs. 39 %, p < 0.0001 and 3–6months: 76 % vs. 51 % p < 0.05, respectively). Wheezing episodes between 6 to12 months of age were also higher in the pneumonia group, but it did not reach statistical significance (6–9months: 56 % vs. 38 %, p = 0.08 and 9–12months: 52 % vs. 35 % p = 0.1, respectively). Children in the pneumonia group had a significantly higher proportion of hospitalization due to ALRI during the 3–6months and 9–12months of age than children without pneumonia (3–6months: 16% vs. 1 %, p = 0.0001 and 9–12months: 4 % vs. 0% p = 0.01, respectively) (table II).
Prevalence (%) of respiratory illnesses in infants with or without pneumonia during the first year of life
| With pneumonia (n = 25) | Without pneumonia (n = 163] | |
| 0–3months of age: | ||
| URTI | 52 | 65 |
| Acute otitis media | 0 | 1 |
| Acute bronchitis | 0 | 3 |
| Wheezing episodes* | 80 | 39 |
| Hospitalization due to ALRI | 12 | 6 |
| 3–6months of age: | ||
| URTI | 56 | 66 |
| Acute otitis media | 8 | 15 |
| Acute bronchitis | 0 | 3 |
| Wheezing episodes** | 76 | 51 |
| Hospitalization due to ALRI* | 16 | 1 |
| 6–9months of age: | ||
| URTI | 68 | 52 |
| Acute otitis media | 20 | 15 |
| Acute bronchitis | 8 | 4 |
| Wheezing episodes | 56 | 38 |
| Hospitalization due to ALRI | 0 | 0 |
| 9–12months of age: | ||
| URTI | 32 | 52 |
| Acute otitis media | 12 | 10 |
| Acute bronchitis | 4 | 4 |
| Wheezing episodes | 52 | 35 |
| Hospitalization due to ALRI*** | 4 | 0 |
URTI: upper respiratory tract infections; ALRI: acute lower respiratory infections.
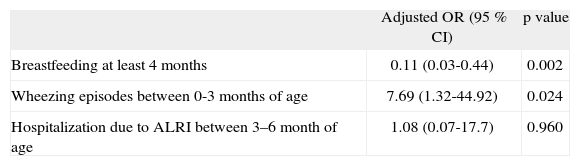
The multiple logistic regression analysis showed that only wheezing in during 0–3months of age was an independent risk factor for pneumonia (OR: 7.7, 95 CI: 1.32-44.92, p = 0.024); conversely, exclusive breastfeeding during the first 4months was a significant and independent protective factor against pneumonia in the first year of life (OR: 0.11, 95 CI: 0.03-0.44, p = 0.002), (table III).
Risk factors for pneumonia during the first year of life: multivariate analysis
| Adjusted OR (95 % CI) | p value | |
| Breastfeeding at least 4months | 0.11 (0.03-0.44) | 0.002 |
| Wheezing episodes between 0-3months of age | 7.69 (1.32-44.92) | 0.024 |
| Hospitalization due to ALRI between 3–6month of age | 1.08 (0.07-17.7) | 0.960 |
The variable "Wheezing episodes between 3–6months of age" was dropped due to colineality. Similarly, "Hospitalization due to ALRI between 9–12months of age" was dropped from the model due to one cell containing 0 observations.
This first birth-cohort longitudinal study performed in Latin America to evaluate risk factors for x-ray confirmed pneumonia in the first year of life shows that infants who have one or more wheezing episodes during the first 3months of life have greater than 7-fold increased risk of developing pneumonia. In contrast, infants who were exclusively breastfed during the first 4months were far less likely to develop pneumonia suggesting that breast feeding provides a major protective effect against pneumonia.
The prevalence of x-ray confirmed pneumonia in the first year of life in our study was considerably higher (13.3 %) as compared to previous community based longitudinal studies where the prevalence of pneumonia during the first five years of life ranged from 4 % to 8.2 % 1,3,21. In addition, the severity of pneumonia in our infants was also higher (32 % required hospitalization) as compared to the Tucson birth-cohort where none of their children who developed pneumonia required hospitalization22.
Nevertheless the prevalence of associated wheezing in the present birth-cohort was enormous in comparison with other longitudinal studies from developed countries, where the prevalence of ≥ 1 episode of wheezing during the first year of life reported in USA and UK ranges from 10 % to 42 %17–19,23 and for recurrent wheezing (≥ 3 episodes) ranges from 8 % to 17 %19,20; while no episodes of pneumonia were reported in those studies19,20. A potential explanation of our higher prevalence of wheezing associated with pneumonia is that during their first year of life 80.3 % of our infants had ≥ 1 wheezing episodes and 43.1 % had ≥ 3 wheezing episodes15. Although we did not study infant lung function in this cohort, it is likely that altered pulmonary function in the first year of life may play a role in the development of wheezing and pneumonia later in life16. It was previously demonstrated in the Tucson birth-cohort study, that children who developed pneumonia in the first three years of life had diminished respiratory function very early on life –mean 2.4months of age– and before any ALRI episode had taken place22. Besides, it is postulated that the first months of life are a critical period where environmental stimuli may alter the innate immune response resulting in more frequent/severe episodes of bronchial obstruction and infections, and eventually pneumonia19,20,23,24. The latter would be supported by our data where the vast majority of pneumonia occurred during the first 3months of life. Similarly Bashour et al21, reported the highest incidence of pneumonia in the first 6months of life. Finally, it is important to emphasize the strong association found in this study between wheezing during first 3months of life and pneumonia during the first year of life that brings for discuss the importance and convenience to initiate controller therapy early after the first wheezing episode in order to decrease the development of pneumonia, at least in disadvantaged communities like ours.
Exclusive breastfeeding during the first four months was the only protective factor against pneumonia which could be identified. This finding is in agreement with a recent meta-analysis where breastfeeding was found to protect against mortality associated with ALRI and pneumonia among children less than one year of age25. Interestingly, we did not find an association between pneumonia and atopy (parental history of atopy and eczema in the child); and a similar finding has previously reported by the Tucson birth-cohort22, where children with pneumonia were not more likely to have positive skin tests to aeroallergens or elevated total serum IgE levels as compared to the control group; leading to speculated the importance of respiratory infection early on life and the developing of non-atopic asthma. We recently reported that children from the same city with non-atopic asthma had more history of pneumonia episodes than children with atopic asthma26.
Other traditional risk factors for pneumonia and/or its severity such as low birth weight, malnutrition, large families, environmental smoke pollution, low socio-economic status and incomplete immunization described in infants and older children from Latin America and other developing countries worldwide3,8–13,27,28 were not found in our birth-cohort study. At least three reasons may explain this difference. Firstly, in our study infants with and without pneumonia shared similar socioeconomic and environmental conditions (e.g. indoor pollution and crowding). Secondly, risk factors considered to be important for the development of pneumonia, such as malnutrition and incomplete immunization were not present in our population. Thirdly, most information on traditional risk factors comes from studies not longitudinally designed to qualify and quantify different respiratory conditions (e.g. wheezing, bronchitis, pneumonia, etc.) that usually also occur during the first year of life.
In addition, when interpreting results from longitudinal studies that have shown certain risk factors for acute infections during the first year of life, we always must be aware that the ecological conditions that were important risk factors in the past (e.g. malnutrition, micronutrient deficiencies, incomplete immunization, indoor smoke from solid fuels, unsafe water and hygiene and poor access to health systems) may have changed over time in those settings29. If the ecological conditions have changed, as it has happened with transitional economies like Chile, it is urgent to redefine the current risk factors for acute infections like respiratory diseases.
The present study has some limitations. Firstly, the cohort of children was small and consequently the number of pneumonia cases observed during the 12month study period is relatively small. Secondly, the etiology of the pneumonia cases could not be assessed, and it is also known that chest radiographs may not reliably distinguish between viral and bacterial pneumonia30. Thirdly, the present birth-cohort may not be representative for all the underprivileged populations across Latin America and other developing countries, although this population may be similar to those commonly found in their big cities. Therefore, more extensive, multi-centre studies, including children from both developed and developing countries, must be performed to determine and compare the current epidemiological characteristics of wheezing and pneumonia especially during the first year of life, the time of the greatest morbidity and mortality.
In summary, this birth-cohort study shows that infants who had one or more wheezing episodes in the first 3months of life had a 7-fold greater risk of developing pneumonia during the first year of life, particularly during the first six months. In contrast, exclusive breastfeeding during the first 4months of life protected against pneumonia. Public health policies e.g. encouraging exclusive breastfeeding and an adequate management of wheezing since the first months of life should be implemented in order to reduce the prevalence of pneumonia and its significant morbidity and mortality in developing countries.
We thank Dr. Joseph Spahn (Health Sciences Center, University of Colorado, CO, US) for his critical review.