To provide a summary of the existing published knowledge on the association between sedentary lifestyle and childhood asthma. Twelve years ago, the first longitudinal studies carried out in children showed a relationship between physical activity and asthma. Several epidemiological studies confirmed these findings, with sedentary lifestyle predicting the onset of asthma.
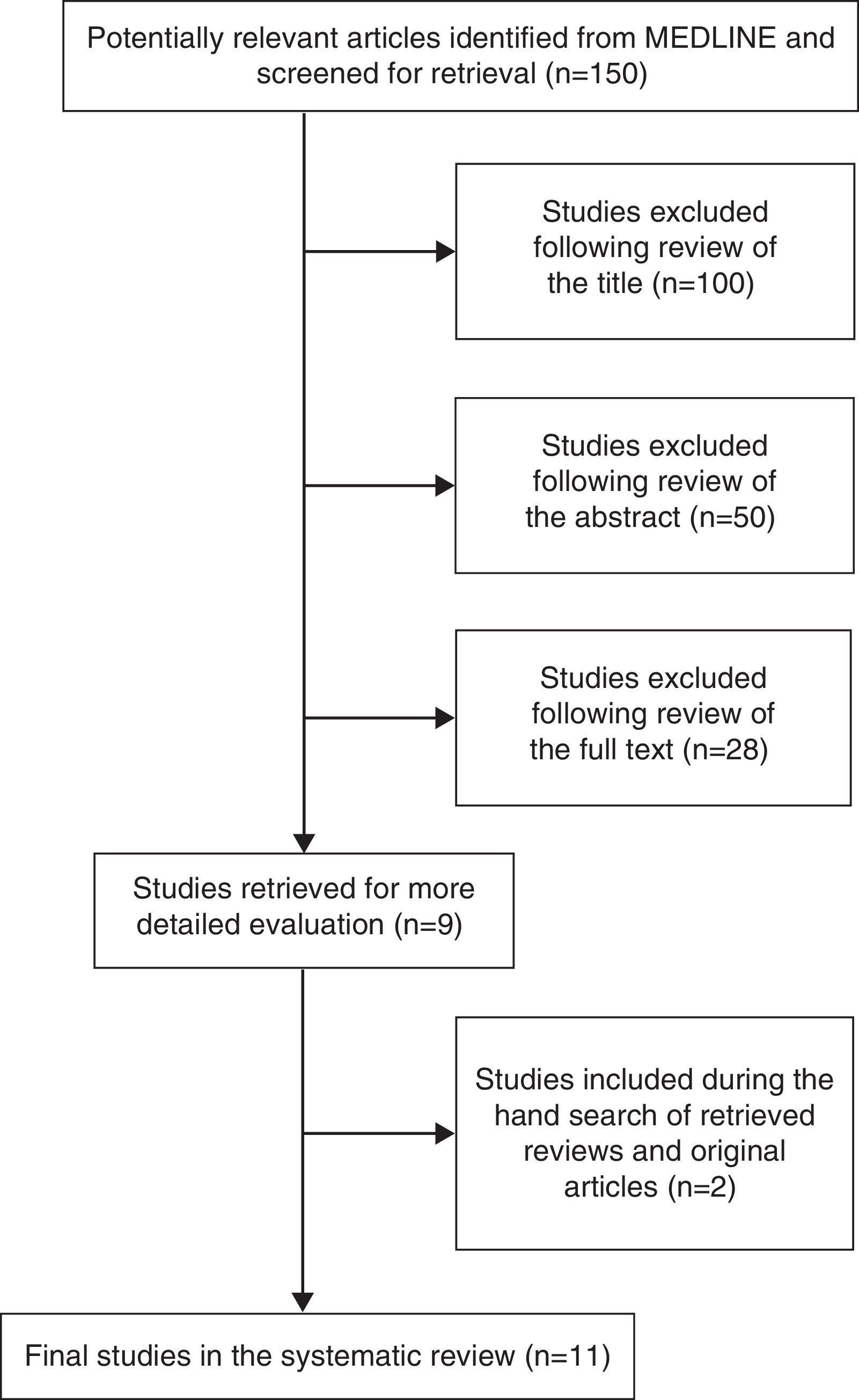
MethodsA systematic review of epidemiological studies was conducted within the MEDLINE database. Epidemiological studies on children subjects, published in English were included in the review. A comprehensive literature search yielded 50 studies for further consideration. Following the application of the eligibility criteria, we identified 11 studies.
ResultsA positive association and an excess risk of asthma during childhood were revealed to sedentary lifestyle. The findings proved the association between childhood asthma and sedentary lifestyle. The correlation between bronchial asthma and sedentary life during childhood and identifying whether preventable or treatable risk factors exist needs to be determined. Further research on the topic is essential for safer and standardised conclusions.
Conclusions and practice implicationAsthma can be controlled when managed properly. The role of the nurse as an educator should establish and maintain a relationship with patients in order to help them manage their disease. The steps towards asthma management will help paediatric patients to guide their approach to the condition.
Twelve years ago, the first longitudinal studies carried out in children showed a relationship between physical activity and asthma.1 Subsequently, several epidemiological studies confirmed these findings, where sedentary lifestyle predicts the onset of asthma.
Bronchial asthma is a common chronic disease in childhood; with a frequency variance between 7 and 11%.2 Recent epidemiological studies suggest that despite its worldwide increase in the last decades, its occurrence seems to be stabilising in many countries. In Greece, the percentage of asthma oscillates from 8 to 11%. Asthma is caused by a combination of genetic and environment factors.3,4
However, the increase in asthma prevalence is related to environmental exposure, rather than to a change in genetic susceptibility. Many factors play an important role in the development of the disease, including outdoor and indoor air pollution; infections; tobacco smoking; allergen exposure; diet; and lifestyle patterns.2
Nowadays there is evidence that limited physical activity or sedentary lifestyle may be linked to childhood asthma, since several studies have shown that exercise functions as a barrier against certain diseases, such as in asthma.5–7 The need for children to have aerobic exercise is now pressing and imperative due to the technological innovations where physical activity imposes, in a certain way, a rather customised sedentary, tense and unnatural way of life. Moreover, physical aerobic exercise is a unique antidote for biological deterioration, which activates all the cells of the body and exercises not only the muscles, but the respiratory and cardiovascular systems as well.3,8,9
Many children and young asthmatics believe that limitations on their activity are an inevitable part of having asthma. On the contrary, a number of strategies which increase their participation in physical activity have been proposed. For example, previous studies and reviews reported that when swimming is compared to other sports, it is linked to a lower asthmogenicity and to a decrease of the severity of asthma symptoms.10–12
AimThe present systematic review aims to summarise the existing published scientific knowledge regarding the association between sedentary lifestyles and bronchial asthma in children.
MethodA systematic review of the literature on the effect of sedentary lifestyle in children's asthma was performed. The following question was applied: “Given the existing epidemiological evidence, the question arises as to whether there is a connection between asthma and sedentary lifestyle on children”. We drew up a review protocol in advance, following standards outlined in the MOOSE guidelines for meta-analyses and systematic reviews of observational studies.13 Furthermore, a systematic comprehensive bibliographic search was carried out using the U.S National Library of Medicine Medline database for the years 1997–2010 and the published interface key terms used were: SEDENTARY LIFESTYLE, CHILDREN'S, ASTHMA, PHYSICAL ACTIVITY, LEISURE TIME AND STUDENTS. Retrieved studies were checked against a list of eligibility criteria while the references of each retrieved study were also checked for additional studies that met the eligibility criteria.
Prior eligibility criteria to restrict studies were defined. Epidemiological studies which referred to children, and published in English after 1997 were only included (of any study design) which compared asthmatic symptoms to inactivity during leisure time. Studies not meeting these criteria were excluded from the review. The following data were extracted from each study: main characteristics, study population, study local measures of effects, and confidence intervals for each outcome.
ResultsFig. 1 shows the number of studies identified and excluded in each phase of the search. Manual searching of references provided an additional study that met the broad eligibility criteria. Ultimately, eleven studies were deemed suitable for inclusion in the review although one study included two sub-studies3,4 and as a result we finally concluded to consider ten studies as the final number of studies included in the systematic review.
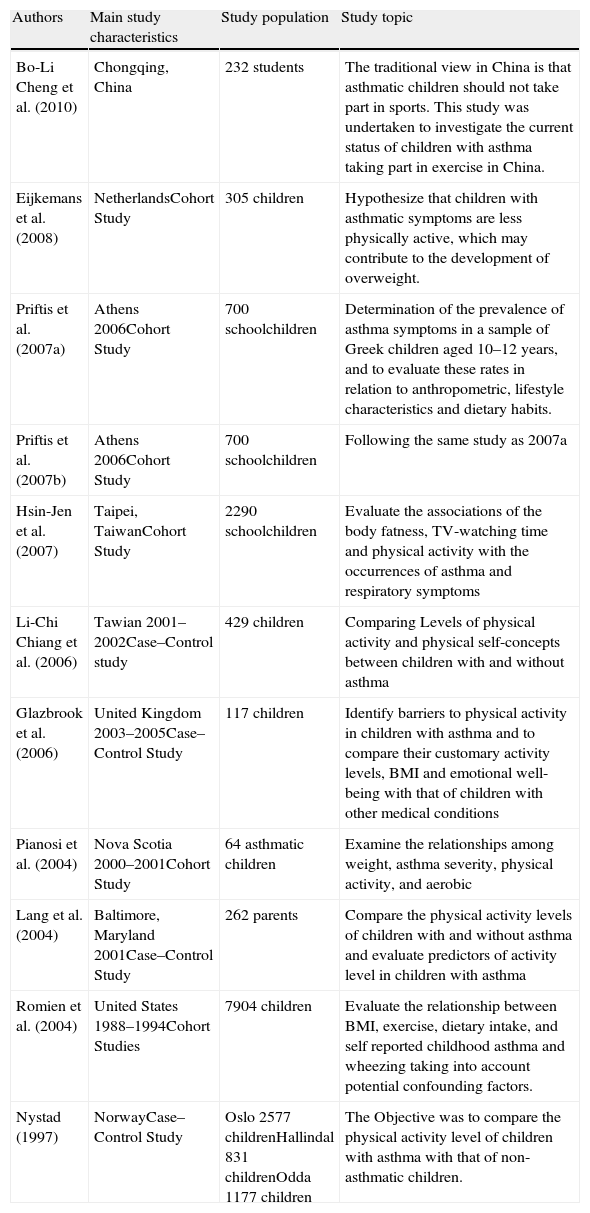
The main characteristics of the studies included in the analysis are given in Table 1 The systematic review included six cross-sectional cohort studies3,4,8,9,14,18 and four case control studies.1,15–17
Summary of the characteristics of studies included in the systematic review.
| Authors | Main study characteristics | Study population | Study topic |
| Bo-Li Cheng et al. (2010) | Chongqing, China | 232 students | The traditional view in China is that asthmatic children should not take part in sports. This study was undertaken to investigate the current status of children with asthma taking part in exercise in China. |
| Eijkemans et al. (2008) | NetherlandsCohort Study | 305 children | Hypothesize that children with asthmatic symptoms are less physically active, which may contribute to the development of overweight. |
| Priftis et al. (2007a) | Athens 2006Cohort Study | 700 schoolchildren | Determination of the prevalence of asthma symptoms in a sample of Greek children aged 10–12 years, and to evaluate these rates in relation to anthropometric, lifestyle characteristics and dietary habits. |
| Priftis et al. (2007b) | Athens 2006Cohort Study | 700 schoolchildren | Following the same study as 2007a |
| Hsin-Jen et al. (2007) | Taipei, TaiwanCohort Study | 2290 schoolchildren | Evaluate the associations of the body fatness, TV-watching time and physical activity with the occurrences of asthma and respiratory symptoms |
| Li-Chi Chiang et al. (2006) | Tawian 2001–2002Case–Control study | 429 children | Comparing Levels of physical activity and physical self-concepts between children with and without asthma |
| Glazbrook et al. (2006) | United Kingdom 2003–2005Case–Control Study | 117 children | Identify barriers to physical activity in children with asthma and to compare their customary activity levels, BMI and emotional well-being with that of children with other medical conditions |
| Pianosi et al. (2004) | Nova Scotia 2000–2001Cohort Study | 64 asthmatic children | Examine the relationships among weight, asthma severity, physical activity, and aerobic |
| Lang et al. (2004) | Baltimore, Maryland 2001Case–Control Study | 262 parents | Compare the physical activity levels of children with and without asthma and evaluate predictors of activity level in children with asthma |
| Romien et al. (2004) | United States 1988–1994Cohort Studies | 7904 children | Evaluate the relationship between BMI, exercise, dietary intake, and self reported childhood asthma and wheezing taking into account potential confounding factors. |
| Nystad (1997) | NorwayCase–Control Study | Oslo 2577 childrenHallindal 831 childrenOdda 1177 children | The Objective was to compare the physical activity level of children with asthma with that of non-asthmatic children. |
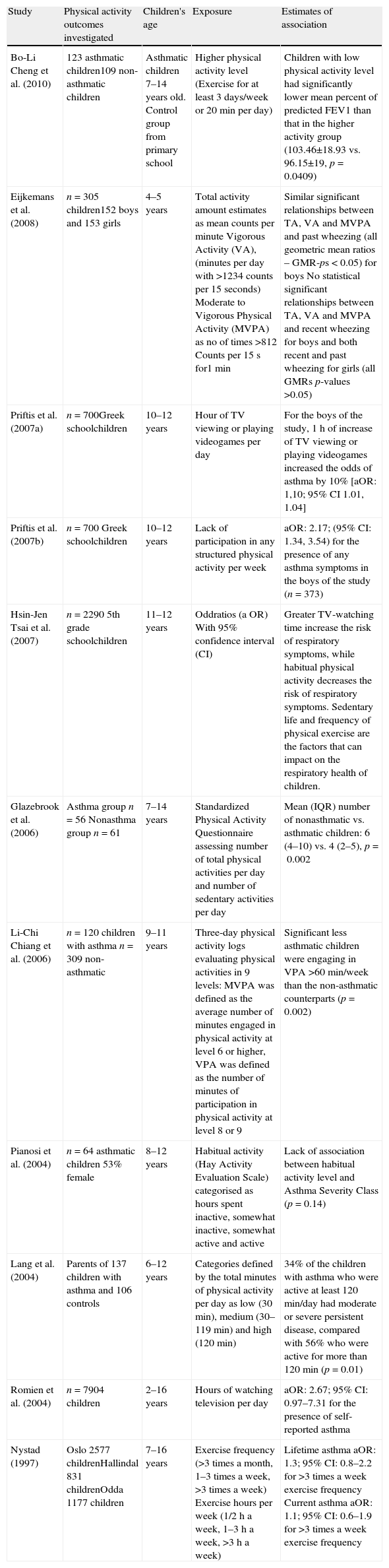
Table 2 summarises the main findings of the ten studies included in the systematic review. Hsin-Jen et al. reported that there was no significant difference in TV-watching time between boys and girls, but boys had more physical activity afterwards than girls did (p<0.05).9 Long TV watching time (>3h/day) was positively associated with more frequent occurrences of five out of seven respiratory symptoms (p<0.05).9 More physical activity was associated with less frequent occurrences of two out of seven respiratory symptoms (aOR=0.66, 95% CI=0.45–0.95 for dyspnoea-associated wheezing and aOR=0.73, 95% CI=0.55–0.99 for exercise-inducing cough) (p<0.05).9
Main Findings of studies included in the systematic review.
| Study | Physical activity outcomes investigated | Children's age | Exposure | Estimates of association |
| Bo-Li Cheng et al. (2010) | 123 asthmatic children109 non-asthmatic children | Asthmatic children 7–14 years old. Control group from primary school | Higher physical activity level (Exercise for at least 3 days/week or 20min per day) | Children with low physical activity level had significantly lower mean percent of predicted FEV1 than that in the higher activity group (103.46±18.93 vs. 96.15±19, p=0.0409) |
| Eijkemans et al. (2008) | n=305 children152 boys and 153 girls | 4–5 years | Total activity amount estimates as mean counts per minute Vigorous Activity (VA), (minutes per day with >1234 counts per 15 seconds) Moderate to Vigorous Physical Activity (MVPA) as no of times >812 Counts per 15 s for1 min | Similar significant relationships between TA, VA and MVPA and past wheezing (all geometric mean ratios – GMR-ps<0.05) for boys No statistical significant relationships between TA, VA and MVPA and recent wheezing for boys and both recent and past wheezing for girls (all GMRs p-values >0.05) |
| Priftis et al. (2007a) | n=700Greek schoolchildren | 10–12 years | Hour of TV viewing or playing videogames per day | For the boys of the study, 1h of increase of TV viewing or playing videogames increased the odds of asthma by 10% [aOR: 1,10; 95% CI 1.01, 1.04] |
| Priftis et al. (2007b) | n=700 Greek schoolchildren | 10–12 years | Lack of participation in any structured physical activity per week | aOR: 2.17; (95% CI: 1.34, 3.54) for the presence of any asthma symptoms in the boys of the study (n=373) |
| Hsin-Jen Tsai et al. (2007) | n=2290 5th grade schoolchildren | 11–12 years | Oddratios (a OR) With 95% confidence interval (CI) | Greater TV-watching time increase the risk of respiratory symptoms, while habitual physical activity decreases the risk of respiratory symptoms. Sedentary life and frequency of physical exercise are the factors that can impact on the respiratory health of children. |
| Glazebrook et al. (2006) | Asthma group n=56 Nonasthma group n=61 | 7–14 years | Standardized Physical Activity Questionnaire assessing number of total physical activities per day and number of sedentary activities per day | Mean (IQR) number of nonasthmatic vs. asthmatic children: 6 (4–10) vs. 4 (2–5), p=0.002 |
| Li-Chi Chiang et al. (2006) | n=120 children with asthma n=309 non-asthmatic | 9–11 years | Three-day physical activity logs evaluating physical activities in 9 levels: MVPA was defined as the average number of minutes engaged in physical activity at level 6 or higher, VPA was defined as the number of minutes of participation in physical activity at level 8 or 9 | Significant less asthmatic children were engaging in VPA >60min/week than the non-asthmatic counterparts (p=0.002) |
| Pianosi et al. (2004) | n=64 asthmatic children 53% female | 8–12 years | Habitual activity (Hay Activity Evaluation Scale) categorised as hours spent inactive, somewhat inactive, somewhat active and active | Lack of association between habitual activity level and Asthma Severity Class (p=0.14) |
| Lang et al. (2004) | Parents of 137 children with asthma and 106 controls | 6–12 years | Categories defined by the total minutes of physical activity per day as low (30min), medium (30–119min) and high (120min) | 34% of the children with asthma who were active at least 120min/day had moderate or severe persistent disease, compared with 56% who were active for more than 120min (p=0.01) |
| Romien et al. (2004) | n=7904 children | 2–16 years | Hours of watching television per day | aOR: 2.67; 95% CI: 0.97–7.31 for the presence of self-reported asthma |
| Nystad (1997) | Oslo 2577 childrenHallindal 831 childrenOdda 1177 children | 7–16 years | Exercise frequency (>3 times a month, 1–3 times a week, >3 times a week) Exercise hours per week (1/2h a week, 1–3h a week, >3h a week) | Lifetime asthma aOR: 1.3; 95% CI: 0.8–2.2 for >3 times a week exercise frequency Current asthma aOR: 1.1; 95% CI: 0.6–1.9 for >3 times a week exercise frequency |
In another similar study in Taiwan, gender was deemed as yet another factor which influenced the need and ultimately the choice of physical activity.17 The most statistically significant effects of asthma were on the level of VPA-Vigorous Physical Activity and perceived flexibility. Girls seemed to opt for less active or physical activities, compared to boys who tended to take up vigorous exercise through free play, in both groups of asthmatics and non-asthmatic children. Among the dependent variables, no statistically significant interactions were found between girls/boys or asthmatics/non-asthmatics in terms of physical activity and physical self-concept.17
According to Priftis et al., the odds ratio of asthma symptoms for boys was 1.13 (95%CI 1.02–1.25) for a 5kg increase of body weight and 1.1 (95%CI 1.01–1.04) for a 1-h increase of watching TV or playing videogames.3 Moreover, boys with asthma symptoms are 2.2 times more likely to refuse to participate in any physical activity than boys without asthma-related symptoms.3 The PANACEA epidemiological study also mentioned that very low physical activity was reported by 16–17% of boys and girls, while 54% of boys and 46% of girls reported that they participated in moderate to vigorous physical activities during a regular week .The time spent for sports-related activities during the week was approximately 4h and a similar amount of time was devoted to non-sports related activities.3,4
The rest of the European studies focused on the physical activity between asthmatic and non-asthmatic children.1,14,16,18 Particularly Eijkemans et al. found an almost similar physical activity level in 4- to 5-year-old children with recent wheezing, compared with children who had never wheezed, in both sexes.18 For boys with past wheezing, a slightly higher activity level was observed compared with boys who had never wheezed.18 Overweight children at the age of 4–5 showed similar physical activity levels compared with children with a normal weight in all of the physical activity variables.18 Obese children showed significantly less vigorous activity and less MVPA-Moderate to vigorous physical activity for ≥1min than normal weight children.18 Pianosi et al. reported no differences on physical activity among the children in each of the various categories of degree of impairment due to asthma.14
However, according to the study by Nystad, asthmatic children were as physically active as their peers.1 There were no significant differences between the exercise frequency, either for children reported ever to have had asthma (p=0.8) or for children with current asthma (p=0.3), compared to non-asthmatics. Similar findings were observed for exercise hours per week.1 On the contrary, Bo-Li Cheng et al. found that asthmatic children in China spent fewer days per week and less time each day on exercise than healthy children specifically among the asthmatic group, 62.60% of children were exercising less than three days per week or 20min per day.19 Children with asthma in the higher activity group were of similar age and gender and had a similar course of disease. In the lower activity group, significantly more children thought that exercise might cause asthmatic symptoms, more children's parents and teachers restricted their exercise, and fewer doctors approved them participating in sports.19
The Glazebrook et al. study showed that the majority of parents (60.7%) reported that their child's asthma acts as a barrier to physical activity.16 On the contrary, only 11% of parents in the non-asthma group children, identified the child's medical condition as an obstacle.16 Furthermore, 23% of parents in the asthma group identified better control of the child's medical condition in terms of participation in physical activity compared with 8.2% in the non-asthma group.16
Similarly, 66.1% of the asthmatic children reported asthma as an obstacle to exercise, compared with only 11.5% of children in the non-asthma group, who characterised their medical condition as an obstacle.16
Lang et al., in their study, reported that in parents of asthmatic children feared that the child would get sick from exercise.15 Asthmatic children and those whose parents believed that the child got upset from strenuous play were more likely to be inactive.15 A final multinomial model supports these findings, where high activity (>120min) was less likely than low activity (<30min) in children with moderate or severe persistent symptoms of the disease, female gender, and whose parents agreed that the child gets upset when he or she plays or exercises hard. Agreement that exercise may make the child's asthma better was associated with the high activity group but the significance level was 0.06.15
DiscussionAs indicated through the systematic review, we have brought together the existing body of epidemiological evidence regarding the possible association between sedentary lifestyle and the child's bronchial asthma.
The main finding from our systematic review is that sedentary life is associated with increased risk of respiratory asthma-symptoms. Along with the previously discussed factors associated with the disease, TV watching time is positively linked with seven respiratory symptoms and suspected asthma.9
These results are in line with the observation of Romieu et al. stating that schoolchildren who have a proclivity to develop asthma, would be more likely to spend more time watching TV because of feeling less energetic or for fear of triggering exercise-induced respiratory symptoms.8 Higher physical activity appears to reduce the risk of respiratory symptoms.9,16 More frequent physical exercise is negatively associated with two out of seven respiratory symptoms.9
According to Priftis et al., the prevalence of asthma symptoms among Greek children was one of the lowest in Europe.3,4 Gender was found to be a major factor influencing physical activity among children, and the prevalence of any asthma symptoms was higher in boys than girls.3,4 Children with asthma perceived themselves to be more flexible than children without asthma.17 Boys had higher scores in physical self-concept especially in endurance, obesity, and strength.17
Recently, exercise prescription has been recommended as another important component of asthma management in children in several countries.19 However, in some countries physical exercise among asthmatic children is still not recommended, for example Chinese children with asthma were less likely to participate in physical activity than their healthy peers due to the perception that the participation of children with asthma in physical activity should be performed in caution.19 Therefore, health professionals need to update their understanding and awareness of the importance of exercise in the disease of asthma.19
Parent health beliefs and stereotypes seem to play an important role in the physical activity of the children with asthma.1,15 Thankfully, very few parents agreed that children with asthma should never exercise.1,15 It is concerning, however, that one quarter of parents with children suffering with asthma, were afraid that their child would get sick if he or she exercised.1,15 The belief that the child gets upset when he or she exercises was associated with inactivity. Additionally, this belief was related to activity level even when the severity of disease was controlled.1,15
From our analysis it is clear that children with asthma do not adopt a sedentary lifestyle and they are as physically active as their peers and thus as physically fit as other children.1,18 However, sedentary lifestyle is associated with increased risk of respiratory asthma symptoms. Moreover, a sedentary lifestyle has previously been demonstrated to be the main factor that may explain low physical fitness among asthmatic children.1,18
ConclusionsThis study area is of great importance, due to the fact that long-term implications are unknown. It is therefore desirable to determine the correlation between bronchial asthma and sedentary life during childhood and identify whether preventable or treatable risk factors exist. This review applies to epidemiologists, health care specialists and the research community as interesting areas for further research work.
Relevance to clinical practice: the role of nurse as educatorAsthma can be controlled when managed properly. Nurses have a central role in asthma management since they establish and maintain a relationship with patients to help them manage their disease by setting specific goals of asthma management, such as normal activity level (including exercise), normal pulmonary function rates, and prevention of symptoms for recurrent episodes of asthma attacks.
Educating parents and children through the basics of asthma management will help paediatric patients to guide their approach to the disease following their daily therapy plan and their action plan for dealing with symptoms. Nurses should develop a specialised plan and conduct their patient education to increase the chances that their patients will follow the recommended actions. Realising the need for activity as a means to alleviate the symptoms of the disease leading to better life quality, it will help patients and their careers to avoid serious consequences which may prevent them from enjoying a natural lifestyle.20
In addition to working with patients, nurses need to build relationships with patients’ families and other health professionals to ensure that support, consistent information, and coordinated care are provided. The results of these joint efforts will be the ability to control asthma attacks, with fewer sick days, and better lives for the patients.20
The effective strategies of education will help patients and parents plan and take action. The paediatric nurse must build confidence by reaching an agreement on goals and activities required and rehearse the asthma management techniques by the following steps: describe to the patients each step they have to take (e.g., review a handout with the patient), show patients each step by doing it themselves, practice by showing patients how to take each step and provide feedback (e.g., when medications are to be taken), ask them to practice the technique (e.g., inhaler technique) at those times and ask them to demonstrate (rehearse) their peak flow and inhaler techniques at every visit.20
Moreover, according to worldwide bibliography, exercise helps asthma management. Nurses should give recommendations for exercise. All patients should be encouraged to exercise and to prevent exercise-induced asthma (referred to as EIA) which affects 70–90% of all patients with asthma as well as 40% of children with allergies but no clinical signs of asthma.21
An exercise diagnostic test helps diagnose the existence of EIA. The nurse must emphasise to patients that they should be able to exercise and ask them to contact their physician or nurse if their plan to control EIA is not working effectively.21
Ethical disclosuresConfidentiality of DataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.