Wheezing/asthma in children is a complex problem due to its heterogeneous condition, with different pathogenic mechanisms, variations in duration and in severity; that make it difficult to totally understand. This relation between wheezing in infants and later development of asthma will be the result of alterations in the immune system maturation and congenital or acquired modifications of the airway. Several longitudinal studies have given us important information about the different phenotypes of wheezing/asthma that coexist in children. In this review, we analyse the recent potential mechanisms and risk factors for each of the three classic wheezing phenotypes presenting in children: transient, non-atopic and atopic; and we propose for consideration a fourth phenotype: overweight/obese girls with early menarche. A better understanding of those risk factors would be useful for the development of new strategies in wheezing/asthma management.
Epidemiological studies carried out in the US1 and UK2 demonstrated that in the vast majority of subjects, nearly 80 %, asthma initiates (incidence) in the first 10years of life, therefore we can say that this is a “paediatric disease”. Many aspects relating to the natural history of asthma remain unknown; however, longitudinal studies have cleared up certain doubts on the pathogenesis and progression of this prevalent disease. It has been determined that asthma is a heterogeneous condition, with signs and symptoms that vary according to the patient's phenotype3; and where certain clinical/functional patterns that are expressed in infancy persist into adult life4,5. Thus, for example, subjects who as children suffered mild asthma without this affecting lung function, when they become adults they will suffer mild exacerbations and without function alteration; while those children who suffered severe asthma, will continue suffering severe asthma as adults and with an important functional loss6; suggesting that the severity of asthma would not change much over time. In the first years of life asthma prevalence is greater amongst males, but after adolescence this gender differences disappear7. Risk factors for the no remission of asthma during adolescence have been determined as early allergic sensitisation, obesity, and bronchial hyperreactivity (BHR)8–10.
MAGNITUDE OF THE PROBLEMThe lack of standardisation in the definition of asthma and in the methodology used in the prevalence studies in different centres throughout the world made comparisons difficult. In the International Study of Asthma and Allergies in Childhood (ISAAC)11, which is a study employing a single methodology with standardised questionnaires and videos on respiratory symptoms, 257,800 schoolchildren (aged 6–7years) in 38 countries and 463,801 adolescents (aged 13–14years) in 56 countries were interviewed with the objective of discovering the worldwide prevalence of asthma (“wheezing in the last 12months”) between 1994 and 1995. The result was that the prevalence varies greatly from one country to another, so that we find that in schoolchildren the range was from 4.1 % in Indonesia to 32.1 % in Costa Rica, and in adolescents from 2.1 % in Albania to 32.2 % in the United Kingdom. Between 2002 and 2003, Phase III of the ISAAC study was carried out 12, which permitted a comparison of the evolution of asthma prevalence at world level during this 7-year interval. The results indicated that for the group of schoolchildren there was a change of 1standard error in asthma prevalence in almost 60 % of the centres (in most cases it increased). On the other hand in adolescents this change occurred in almost 77 % of the centres (but in only in half of these it increased and in the other half it decreased-above all in those which already had high prevalence-). In Spain, the annual change in asthma prevalence between Phases I and III was of + 0.44 for schoolchildren and adolescents; however in the region of Latin America these annual variations fluctuated from −0.13 in Panama to + 0.69 in Costa Rica for schoolchildren and from −1.06 in Peru to + 0.88 in Panama for adolescents12.
Until a few decades ago, it was not clear if the wheezing that occurred in infancy was the first symptom of asthma or if it was a transient and different event. The first epidemiological study carried out to clarify this dilemma date back to 1953 in Copenhagen, where Boesen13 demonstrated that the age at which the children had been admitted to hospital for “asthmatic bronchitis” was a determining factor for wheezing at school age; so for example if hospital admittance occurred in the first 6months of life then only 3 % carried on suffering asthma episodes at school age, while this proportion increased to 7 % if the hospital admittance was between 6 and 11months of life, to 18 % if it was between 1 and 2years, and to almost 42 % if the admission occurred after the age of 3years of life. Although in that study it was not clearly established if hospital admittance occurred during the first obstructive episode or if it was a reflection of multiple previous episodes, these findings served to infer that despite the fact that infants of less than 6months of age required hospitalisation for severe obstructive symptoms, the prognostic of continued wheezing at school age was low; and conversely said prognostic is overshadowed if the hospitalisation occurred at an older age. Later, Eisen and Bacal14 established that only 25.4 % of infants who had a single episode of bronchiolitis in their infancy suffered asthma at school age, and family history of allergy was an important risk factor. Welliver et al15 demonstrated that those children with persistent wheezing were the ones who presented an immune response with the highest levels of specific IgE against infection by respiratory syncytial virus (RSV), compared to those children with transient wheezing16. To determine that an infant who wheezes in the first years of life has a greater risk of developing persistent asthma would give us the opportunity to improve our management and thus theoretically reduce morbidity.
In 1964, a longitudinal study on asthma was started in Melbourne, Australia4,5,17. Schoolchildren of 7years of age were randomly enrolled in the cohort, and according to a questionnaire on respiratory symptoms were classified into four groups: those who never wheezed (“control”); those who had < 5 episodes of wheezing associated to respiratory infections (“mild wheezers”); those with 5 or more episodes of wheezing associated to respiratory infections (“moderate wheezers”) and those who had wheezing not associated to symptoms of respiratory infections (“asthmatics”). A fifth group of children with “severe asthma” was selected from the same cohort at the age of 10years. At 35years of age, the participants were re-evaluated and classified as: “no recent asthma” (no episodes of wheezing in the last 3years), “infrequent asthma” (wheezing episodes in the last 3years but not in the last 3months), “frequent asthma” (wheezing episodes less than once per week in the last 3months) or “persistent asthma” (wheezing once or more per week in the last 3months). The researchers reported that 77 % of those children catalogued in their infancy as “mild wheezers” were asymptomatic at 35years of age and only 23 % presented “frequent asthma” or “persistent asthma”. However, 50 % of the subjects who in their infancy had been catalogued as “asthmatics”, at 35years of age presented symptoms of “frequent or persistent asthma”; and up to 75 % of those diagnosed as having “severe asthma” at the age of 10years presented symptoms of “frequent or persistent asthma” at the age of 35years17. Thus with this information, we can conclude that the more severe the asthma during the infancy, the smaller the probability there is that the symptoms will disappear in adult life. These data support the concept of “clinical tracking of asthma”, that is to say that those children with mild disease tend to remit or continue with a mild disease when they are adults, while those children with severe asthma will continue suffering severe asthmatic exacerbations in adult life. Nevertheless, there is not just a clinical tracking, but also there is a “functional tracking of asthma”, since this same cohort demonstrated that those children with “severe asthma” presented an abnormal lung function, shown by a lower forced expiratory volume in the first second (FEV1) which did not improve when they became adults. Those children catalogued as “mild asthmatics” had a normal or slightly altered lung function throughout adult life; and those with “slight or moderate wheezing” in their childhood had a totally normal lung function at the age of 354,17. This behaviour of lung function over time makes it clear that in asthmatics there would not be an important extra loss in lung function after the age of 7–10years, which could be interpreted in two ways: that asthmatic children are born already with a lower lung function; or that they lose it some time after birth, but before they are 7–10years old and without almost any further later loss. The epidemiological studies of the Tucson cohort confirmed that the latter is what actually occurs.
In the longitudinal study in Tucson (USA), which began in 1980, the children were enrolled from birth; and at the age of 6years, according to the presence of wheezing episodes in the 3 first years of life, they were classified by Martinez et al.8 into “no wheezing or controls” (those children who had never wheezed), “transient wheezers” (wheeze on at least one occasion in the first 3years of life but not at 6years), “late-onset wheezers” (no wheeze in the first 3years of life but yes at 6years) and “persistent wheezers” (those who had wheeze at least on one occasion during the first 3years of life and at 6years continued wheezing). Lung function (maximal flow at functional residual capacity or VmaxFRC) tests carried out in the first 3years of life and prior to any episode of respiratory infection were similar in the “control” children and the “persistent wheezers”; however at 6years of age those children with “persistent wheezing” already had a significantly lower lung function (VmaxFRC), and this remained deteriorated in the spirometry (FEV1) carried out at 18years18. This made it clear that the loss in lung function in those patients with wheeze/asthma occurs after the first year of life but before 6years and that said functional deterioration persists through to adolescence. Recently, Stern et al19 reported that those children who in their first months of life had a lower lung function (lower quartile of the VmaxFRC) were those who at 22years maintained a poor lung function (lower quartile of FEV1, FEV1/FVC ratio and FEF25-75) independently of wheezing, atopy, tobacco, and parents' asthma history. Thus, a poor lung function at a very early age, almost at birth, should be recognised as a risk factor for the obstruction to airflow in early adulthood, and perhaps the prevention of chronic obstructive lung disease should be commenced in foetal life.
The longitudinal study in New Zealand10, initiated in 1972, enrolled children at birth and evaluated them on seven occasions (from 9 to 26years of age). Around 25 % of the subjects studied had “persistent wheezing” (wheezing present in all the evaluations) or with “relapses” (wheezing present in two successive evaluations, then absent in at least one or more, and then it finally reappears in two or more evaluations); 21 % presented “transient wheezing” (present in only one evaluation) and 15 % had a “remission” of the symptoms (absence of wheezing after having been present in at least two successive evaluations). Lung function (FEV1/FVC ratio) of the subjects with persistent wheezing or with relapses during this time was significantly lower than that of those who did not present wheezing. Moreover, the authors reported that the predisposing factors for the persistency or relapses in wheezing were the sensitisation to house dust, greater BHR, female gender, exposure to tobacco smoke, and the early start of the wheezing episodes.
Wheezing in infancy is, therefore, a heterogenic (phenotype) condition with probably some superposition between them. On the one hand, an important group of children exists who begin their wheezing episodes in early infancy but that these remit at school age; and on the other hand, there are those infants for whom the wheezing is the first sign of asthma. Unfortunately, unique biological or even genetic markers do not yet exist which can help us to discern if a wheezing infant will suffer asthma at school age or will not20. The diagnosis of asthma continues to be clinical, supported by the family and personal history of asthma/atopy and the elevation of serum IgE21. The combination of clinical characteristics and simple biological markers could be of use in the elaboration of algorithms which may help us to discern these two groups of children who start to wheeze at an early age. Castro-Rodríguez et al22 elaborated an algorithm called the “asthma predictive index” (API), which combines clinical and laboratory criteria to predict which subjects who suffer wheezing at preschool age will continue to suffer asthma at school age. The algorithm is positive if a child has more than 3 episodes of wheezing during the first 3years of life plus one major criterion (medical diagnostic of eczema or parents with asthma) or two minor criteria (wheezing symptoms not related to colds, medical diagnosis of allergic rhinitis, or eosinophilia in peripheral blood ≥ 4 %). Upon applying this algorithm to the Tucson cohort, this produced a specificity of 97 % (probability that the schoolchildren without asthma would have had a negative API in their infancy), a positive predictive value of 77 % (probability of the infants with a positive API of having asthma at school age, or said differently, it was unable to detect 23 % of persistent wheezers) and a negative predictive value of 69 % (probability that the infants with negative API do not have asthma at school age, or that it was unable to detect around 30 % of transient wheezers). The API, although not perfect, is to date the nearest that we have to being able to predict which infants with wheezing are going to be asthmatics during school ages. Recent randomised clinical studies with asthma controlling medication are being incorporated into this algorithm23.
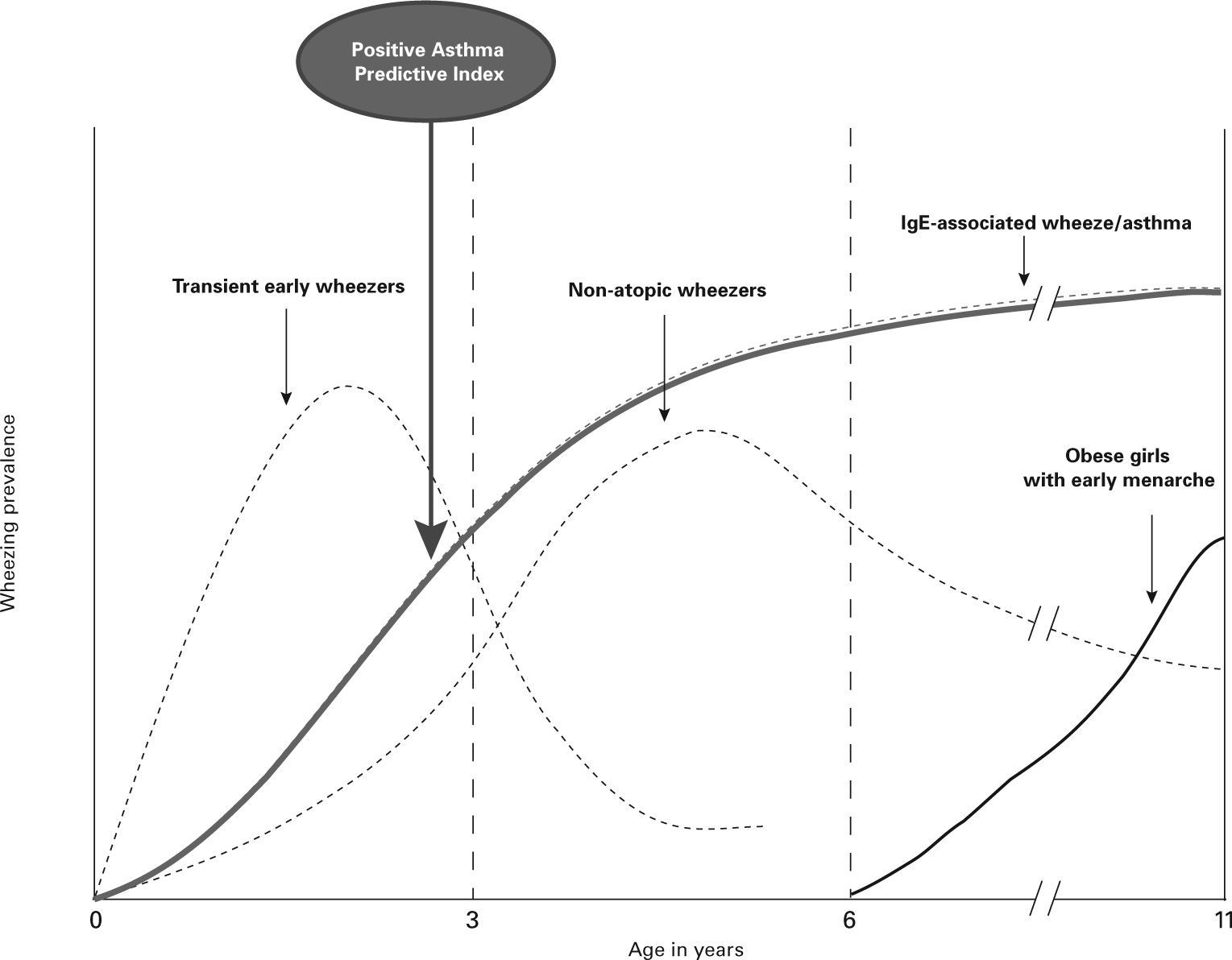
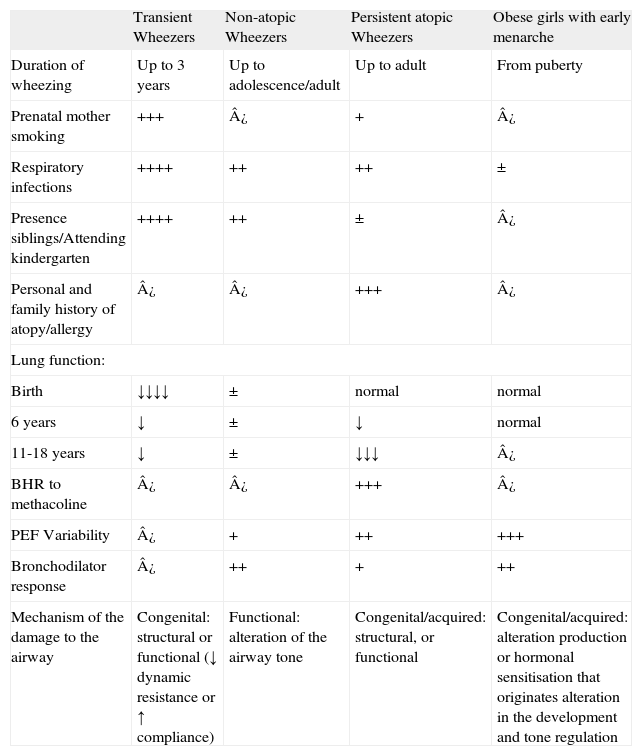
PHENOTYPES OF WHEEZE/ASTHMA IN CHILDRENThe majority of the epidemiological studies suggest that distinct phenotypes of asthma exist with heterogeneous conditions, which follow a common final way characterised by recurrent bronchial obstruction. To the three classical phenotypes previously described: “early transient wheezers”, “non-atopic preschool wheezers” and “atopic asthmatics/wheezers” we propose the consideration of a fourth phenotype: “overweight/obese girls with early menarche” (Table I and Fig. 1).
Characteristics of the Phenotypes of Wheezing/Asthma in Childhood
| Transient Wheezers | Non-atopic Wheezers | Persistent atopic Wheezers | Obese girls with early menarche | |
| Duration of wheezing | Up to 3years | Up to adolescence/adult | Up to adult | From puberty |
| Prenatal mother smoking | +++ | ¿ | + | ¿ |
| Respiratory infections | ++++ | ++ | ++ | ± |
| Presence siblings/Attending kindergarten | ++++ | ++ | ± | ¿ |
| Personal and family history of atopy/allergy | ¿ | ¿ | +++ | ¿ |
| Lung function: | ||||
| Birth | ↓↓↓↓ | ± | normal | normal |
| 6years | ↓ | ± | ↓ | normal |
| 11-18years | ↓ | ± | ↓↓↓ | ¿ |
| BHR to methacoline | ¿ | ¿ | +++ | ¿ |
| PEF Variability | ¿ | + | ++ | +++ |
| Bronchodilator response | ¿ | ++ | + | ++ |
| Mechanism of the damage to the airway | Congenital: structural or functional (↓ dynamic resistance or ↑ compliance) | Functional: alteration of the airway tone | Congenital/acquired: structural, or functional | Congenital/acquired: alteration production or hormonal sensitisation that originates alteration in the development and tone regulation |
BHR: bronchial hyperreactivity; PEF: maximum forced peak expiratory flow.
These are children with symptoms only during the first three years of life and whose principal characteristics are the absence of family and/or personal history of atopy; and that they are born with a lower lung function compared to the controls8. Lung function, according to a recent report on the Tucson cohort, remains diminished until 18years of life, although with a slight improvement19. Other studies, although without following up for such a long time as the above study, reported similar findings24,25. The children of this phenotype do not have a greater BHR measured with methacholine provocation tests, nor do they have greater variability in their maximum forced peak expiratory flow (PEF) measured at 11years of age3. Thus it is postulated that the reduced lung function observed in these infants would be explained by structural or functional changes in the airway (a reduced resistance of the airway or an increase of the dynamic compliance, more than an increase in the lability of the airway) which would predispose these subjects to wheeze when they have symptoms of acute respiratory infections26.
Other risk factors for transient wheezers include prematurity, since this conditions a smaller airway27 and the exposure to siblings and/or contact with other children in the kindergarten (their greater exposure to respiratory infections would cause a change in the production of Th2 lymphocytes)28. Passive smoking is also a risk factor which contributes to having a lower lung function25,29; especially in utero exposure to tobacco smoke is closely associated to a greater risk of wheeze at school ages30. Stein et al31 demonstrated that maternal prenatal—but not postnatal-smoking was associated with a higher prevalence of transient wheezing in the first three years of life, but not after that age. Another risk factor, described by Martinez et al32 is the younger age of the mother, although the explanation of this fact is not very clear, it is postulated that the cause would be a lower lung function that these children are born with. The younger age of the mother was not related with atopy33.
2Non-atopic wheezersThis phenotype is composed by children who present recurrent wheezing that starts in late infancy or preschool age and continue beyond the age of 6years, but with a tendency to disappear in pre-adolescence3,34; probably this category contains a subgroup of the transient wheezers whose symptoms did not cease at the age of 3years. The children of this phenotype do not have personal and/or family history of atopy/allergy34, and thus they are also called “persistent non-atopic wheezers”. As with the first phenotype, acute respiratory infections are the principal factor which trigger the obstructive symptoms. However, the prevalence of smoking during gestation is not a risk factor. On the other hand, these children have a lung function from birth to 11years of age which is slightly lower in comparison to healthy subjects, and do not present BHR to methacoline but do present greater variations in the PEF than healthy subjects3. Thus it is postulated that the mechanism is probably due to a functional alteration in the regulation of the motor tone of the airway.
The vast majority of exacerbations or asthmatic exacerbations in children, and between half and three quarters in adults are associated with viral infections, with the rhinovirus being the most frequently reported pathogen, and thus many studies have explored the relation between virus and asthma35–37. Stein et al38 in a longitudinal study demonstrated that those children who had an infection by RSV in the first 3years of life had a greater risk of wheeze only up to the age of 11years, independent of atopy. Moreover, these children with RSV infections had a significantly lower FEV1, and a greater response to bronchodilators, in comparison with those without infections. These findings would indicate that these children were born with reduced lung function or that there was an interaction between their immune system and the virus at a crucial moment in their life which altered lung growth or indeed that both factors were present.
As we shall point out below it is probable that, depending on the environment, the prevalence of non-atopic wheezers or asthmatics is the same or even greater than that of atopic wheezers/asthmatics.
3Persistent atopic wheezers/asthmaticsThis third phenotype is composed by children who start obstructive symptoms in the first three years of life (also triggered by viral respiratory infections) and who continue wheezing during school age. It is important to stress that these children have personal and family histories of asthma/atopy and who are born with a lung function which is similar to those subjects who never wheezed or to healthy controls, but which declines sharply and significantly at 6years of age, and then remains diminished until the age of 18years8,9; so it can be inferred that the decisive changes in the airway would commence very early on in life.
Although amongst schoolchildren with persistent asthma, the fact that they had the first wheezing episode under the age of 3years is associated to an increase in the severity of the disease and greater BHR, the relation between BHR in infancy and the subsequent development of asthma is not very clear. For example, there are studies in which the BHR measured at early ages of life, but after the first wheezing episode, did not bear relation with the BHR measured at later ages 39,40; however, other reports suggest that the BHR measured very early on in life does correlate well with the BHR and the prevalence of asthma at 6years of life41. Another study 42 which evaluated lung function and BHR in the first months of life of children with a family history of atopy, demonstrated that the level of lung function predicts which boys are going to wheeze, while BHR predicts the girls who will wheeze. Although the authors do not suggest it, these gender differences could be due to the fact that the girls with BHR already presented an inflammation in the airway.
Frequently the type of asthma that starts at an early age in childhood is associated with atopy, that is to say a genetic predisposition for the sensitisation to allergens42. Therefore, allergic sensitisation would play an important role in the genesis of the persistent school age asthma. A study carried out on Australian children enrolled between 8 and 10years of age demonstrated a significant correlation between allergic sensitisation and asthma symptoms43. That population was divided into three groups: those sensitised upon entering the study, those who became sensitised during the study, and those who were never sensitised. The prevalence of persistent obstructive symptoms (wheezing, exercise induced wheezing and nocturnal cough) was the same in the children sensitised during the study as for the never sensitised children (11 % vs. 12 %). However, those sensitised at the start of the study had a prevalence of respiratory symptoms significantly higher (40 %) than the other two groups.
Although the high levels of total serum IgE at birth (umbilical cord) are a risk factor associated to a greater development of allergic conditions such as infant atopic dermatitis44, they are not so for persistent wheezing. Thus, the measuring of serum IgE in the umbilical cord would not be a sensitive marker of the foetal immunological characteristics which could predispose to the later development of asthma8. However, atopic dermatitis in infancy is in itself a risk factor for “persistent wheezing”8,22. Curiously, these infants with “persistent wheezing” present elevated levels of serum IgE at 9months of life, which would induce us to think that close to that age the immune system acquires the characteristics of the older asthmatic child. It is not known if these subjects with “persistent wheezing” are already sensitised to the same allergens during the moment in which they start to develop the first wheezing episodes or if this sensitisation will play a role in the subsequent develop of bronchial asthma. What is known from prospective studies is that the children who will develop asthma symptoms have a greater probability of being sensitised to foods at early stages in their life as compared to non-asthmatics45. It would seem that this “atopic march”46 starts with a pattern of sensitisation to different antigens according to the different ages of the children, and that initially in the infant stage it is due to food antigens (and perhaps by certain viral antigens) to later continue with aeroallergens prevalent in the zone in which they live; for example: house dust in coastal region47, cockroaches in poor zones of the US 48, olive in Spain, and fungi in desert zones49.
Some factors which are protective or reduce the risk of asthma or persistent wheezing have also been identified, such as the exposure to other children in the home or attending a kindergarten28, presence of pets50,51, exposure to farm animals52,53, and greater consumption of the Mediterranean diet54,55.
Garcia-Marcos et al54 reported that a high consumption of the Mediterranean diet, a diet rich in antioxidant cis-monounsaturated fatty acids (due to the high consumption of vegetables, fruit, pulses and grains; and moderate consumption of meats and dairy products) was a protective factor for severe asthma in Spanish schoolgirls. Chatzi et al55 also demonstrated the protective effect of the Mediterranean diet on asthma and allergic rhinoconjunctivitis in schoolchildren in Greece. Recently, Castro-Rodriguez et al56 studied Spanish preschoolers and reported that the Mediterranean diet is a protective factor for recurrent wheezing.
Ball et al28 demonstrated, in the Tucson cohort, that those children who had older siblings in the home or who went to day care during the first 6months of life had significantly more wheezing during the first 3years of life, but less development of asthma and atopy at school age compared to children without older siblings or who did not attend a créche. Hesselmar et al50 demonstrated that Swedish children exposed to pets in the first year of life had a lower incidence of rhinitis and asthma at school age. Remes et al51 reported that those children in Tucson who were exposed to the presence of dogs at home in the first months of life had a significantly lower risk of developing frequent wheezing at school age, this was especially evident in children without paternal history of asthma; however the exposure to said pets was not a protective factor for later atopic sensitisation. Ernst et al52 in a study carried out on Canadian schoolchildren reported that those children from rural areas who grew up on farms had a lower risk of wheezing/asthma, lower BHR and lower allergic sensitisation during adolescence compared to those children from urban zones (not exposed to the farm), independently of the number of siblings. This was subsequently corroborated53. However, doubt is raised as to whether the difference in asthma/wheezing prevalence is due to a greater early exposure to the bacterial lipopolysaccharides in the animal faeces in the farms or to the greater environmental pollution in the urban zones.
Gereda et al57 reported that exposure early on in life to the endotoxin of house dust is a protective factor against the development of allergic sensitisation. These investigators found that the children who lived in houses with high concentrations of endotoxins had an increased proportion of interferon gamma (IFN-gamma) and T lymphocytes, but not of interleukins (IL-4, IL-5 e IL-13). This suggests that early exposure to endotoxins could protect against allergic sensitisation by increasing the TH1 immunity, confirming the so-called “hygiene theory” (where greater exposure to infections would produce a lower prevalence of allergic diseases and asthma). Guerra et al58 demonstrated that those children with lower production of levels of CD14 (at birth) and lower IFN-gamma (at 3months of life) had a greater risk of developing recurrent wheezing in the first year of life. As we know, CD14 acts like a recognition pattern for the endotoxins and the production of IFN-gamma has been positively related to the level of exposure to endotoxins. This was confirmed by Stern et al59 who established that the risk of wheezing between 2 and 13years of life increases significantly in those subjects with a low production of IFN-gamma, measured at 9months of life, compared to those subjects with high levels of IFN-gamma, and this relation was not present if the wheezing appeared after 6years of life. That is to say that the characteristics of the immune system present in the first year of life can anticipate the risk of developing wheezing, or expressed in another way, susceptibility to asthma is established very early on in life.
Co-existence of atopic/non-atopic asthmaUntil a few decades ago it was thought that the immense majority of asthmatic children belonged to this phenotype of “atopic asthma” and that in those less-developed countries due to the fact that there are more infections there must be a lower prevalence of asthma. Anderson60 reported that in Papua New Guinea there were almost no children and adolescents with asthma, but on the other hand the incidence of upper respiratory infections was up to 4 times greater than that reported in English schoolchildren. Von Mutius et al61 found that the prevalence of rhinitis, asthma, and BHR were significantly higher among the children of the ex-West Germany versus that of the ex-East Germany; but the incidence of bronchitis or respiratory infections was greater in the latter. A study in the Fiji isles62, demonstrated that the children from the populations with a greater economic income had a significantly higher prevalence of frequent wheezing than those with lower incomes, but curiously the latter had a higher rate of respiratory infections or chronic cough. Another study carried out in Ethiopia63, reported that in the children from urban zones the atopy was strongly associated to asthma, which was different to those from the rural zones where there was no positive skin test among the asthmatics. Finally, Penny et al64, demonstrated in Peruvian schoolchildren that atopy was present in only 28.6 % of the asthmatic children. This leads us to speculate about the possibility that a large proportion of the asthmatics in those poor countries are “non-atopic asthmatics”.
Pearce et al65 after analysed several studies worldwide concluded that only 58 % of asthma cases were attributable to atopy (measured as a positive skin test) and suggest that the importance of the atopy/allergy as a cause of asthma has been overestimated. Garcia-Marcos et al66 in a population study reported that only 62.4 % of asthmatic Spanish schoolchildren were atopic; and that the risk factors for atopic asthma and non-atopic asthma are different (male gender and parents with asthma for the case of the atopic asthmatics, whilst mother smoking in the first years and the presence of damp in the home for the case of the non-atopic asthmatics). Castro-Rodriguez et al67 in a study carried out in a population selected from a Chilean tertiary centre, demonstrated that 62.5 % of the asthmatic children were atopic. These atopic asthmatics had more severe symptoms (more emergency appointments and oral corticosteroid use) compared with non-atopic asthmatics, who in turn had an earlier start in their symptoms, more respiratory infections and greater exposure to tobacco than the atopic asthmatics. Finally, Mallol et al68 recently demonstrated that the wheezing in Chilean adolescents from a socioeconomic disadvantaged population was related to BHR but not to allergic sensitisation.
All this evidence would explain why the ISAAC study 11 reported that the highest rates of prevalence of asthma/wheezing occurred in children from developed countries (25 % in Australia and New Zealand) as well as from developing countries (23 % in Brazil, 32 % in Costa Rica and 24 % in Panama) and the same was true for adolescents (28 % in Australia and 24 % in New Zealand versus 20.7 % in Oman and 28 % in Peru). This immediately leads us to wonder whether the “hygiene theory” is a universal theory to explain the recent increase in asthma prevalence at world level, since according to this theory there should be fewer cases of asthma in the less-developed countries, which we have seen is not what happens. It is most likely that in schoolchildren and adolescents these two types of asthma (atopic and non-atopic) coexist, and that perhaps in places where respiratory infections are still very prevalent (such as in developing countries) the high asthma rates are due to the existence of cases of “non-atopic asthma”, as opposed to the most industrialised countries where the high prevalence of asthma is due to the cases of “atopic asthma”.
4Overweight/obese girls with early menarcheCastro-Rodríguez et al69 reported that in the Tucson cohort the girls, but not the boys, who became overweight/obese between the ages of 6 and 11years had 7 times more risk of developing asthma (incidence) than those who remained eutrophic, independent of the physical activity and the allergic condition; moreover these overweight/obese girls presented a greater bronchodilator response (measured by FEV1) and greater variations in PEF than the eutrophic ones. However, this greater prevalence of asthma amongst the girls who became obese occurred exclusively among those who had menarche before the age of 11years and not in those with later menarche. This would tell us that the obesity alters the production (or peripheral sensitisation) of the hormones related to puberty in girls and that an increased production of feminine hormones (or their sensitivity) would alter lung development and the regulation of the tone of the airway in girls in puberty (shown by a greater bronchodilator response) and thus triggering wheezing/asthma.
Subsequently, Varraso et al70 in a study in France, confirmed this finding, reporting that the association between obesity and asthma was more evident amongst women with an early menarche. Herrera-Trujillo et al71 demonstrated that those obese Mexican girls with menarche before the age of 11years had significantly more risk of asthma than those who had menarche after the age of 11years. Recently, Garcia-Marcos et al72, in a study carried out on Spanish schoolchildren, reported that obesity was a risk factor for severe recent asthma (in the last 12months) but only in those without associated allergic rhinoconjuntivitis. A new revision confirms that neither allergy, nor BHR are present in the association between obesity and asthma73. It is important to stress that being overweight/obese at 11years of age and early menarche were risk factors for the persistence of asthma after puberty9. For all of the above, we propose this group of obese, non-atopic girls with early menarche as a fourth phenotype of paediatric asthma74 (Table I and Fig. 1).
CONCLUSIONSAsthma/wheezing in children is a complex problem, where different pathogenic mechanisms can result in the appearance of wheezing symptoms at different ages and with different durations throughout childhood. It is probable that asthma is the result of alterations in the maturity of the immune system, congenital and acquired disorders of the airway where the environment plays a predominant role. To the three classical phenotypes of asthma/wheezing in children already known (transient, atopic, and non-atopic), we propose the consideration of a fourth phenotype: obese/overweight girls with early menarche. A better understanding of said factors will be extremely useful for the development of strategies for the treatment and prevention of recurrent bronchial obstruction /asthma in infants and older children.
We thank Mr. Anthony Carlson for his editorial assistance.