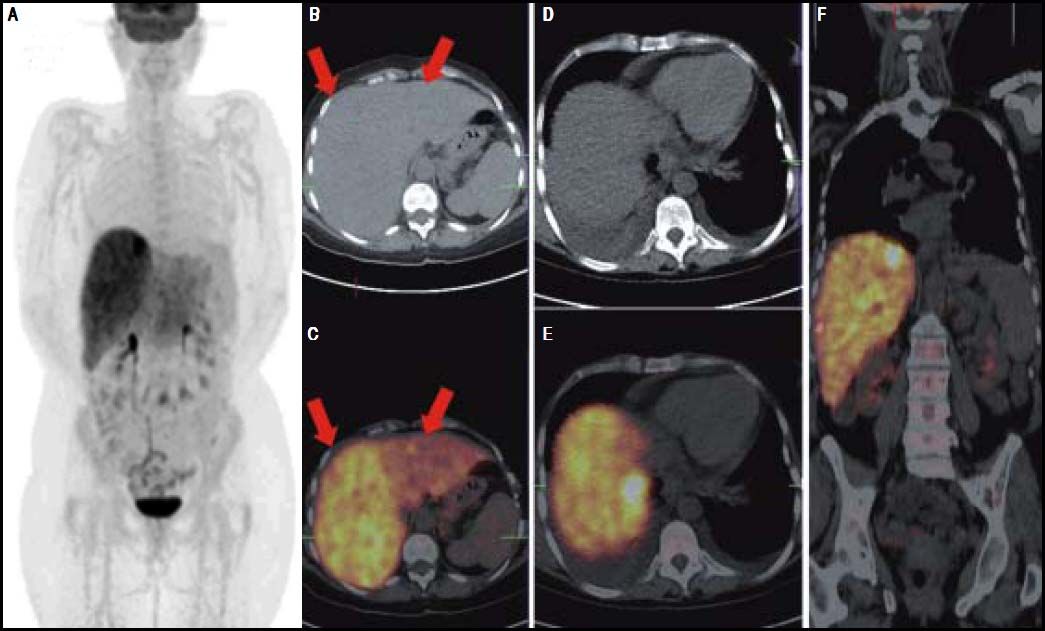
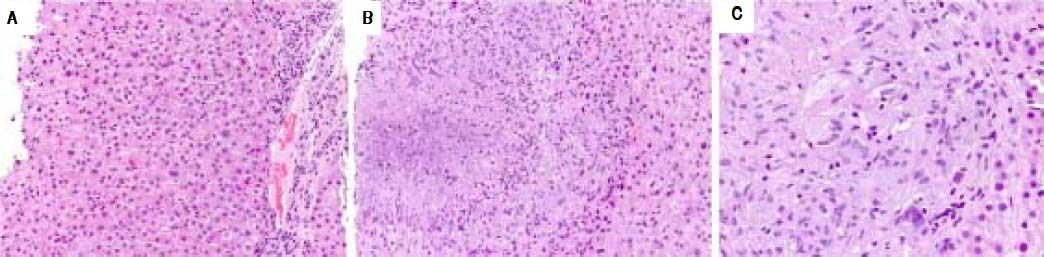
A 50 years-old female was presented to our attention complained for a 3 weeks recurrent chilling fever accompanied, productive cough and dyspnea. An initial laboratory evaluation showed a C-reactive protein (CRP) level of 183 mg/L [reference value (rv) < 5 mg/L], hemoglobin (Hb) level 97 g/L, glutamic oxaloacetic transaminase (GOT) and glutamic-pyruvic transaminase (GPT) respectively of 39 and 43 U/L (rv GOT < 36 U/L and GPT < 37 U/L). A serological test to investigate hepatitis was negative. Patient performed an abdominal ultrasonography showing signs of cholecystitis, a chest X-ray showing thickening of basal lung parenchyma with bilateral pleural effusion. Initial anti-inflammatory treatment followed by a broad-spectrum antibiotic therapy failed with increase of inflammatory parameters. Cytology obtained by thoracentesis and bronchioloalveolar washing was negative for pneumonia, cytomegalovirus, respiratory viruses and bacteria, tuberculosis cultural growth. The patient performed a contrast-enhanced CT and a 18F-FDG-PET/CT, in order to exclude a possible oncological genesis: a preferential uptake of the right hepatic lobe (Figures 1A-1C) with a focal uptake in the segment VIII was observed (Figures 1D-1F). On the basis of these findings a tru-cut biopsy was performed revealing a necrotizing granulomatous hepatitis (mild lymphohistiocytic inflammation and epithelioid granuloma with multinucleated langhans cells) (Figures 2A-2C). Any viral or mycobacterial (included TBC) origin was excluded, confirming an idiopathic granulomatous hepatitis. Colchicine was administered for seven days with rapid regression of inflammatory syndrome and liver dysfunction.
Granulomatous hepatitis (GH) seems to be a common cause of fever of unknown origin (FUO) mainly caused by biliary cirrhosis, sarcoidosis, tuberculosis, chronic active hepatitis, drugs’ hypersensitivity, Hodgkin’s disease, adenocarcinoma and radiotherapy and chemotherapy late effects.1 Idiopathic granulomatous hepatitis (IGH) is less frequent representing about 10% of liver granulomatosis.1,2 Diagnosis is confirmed by liver biopsies in 15-30% of cases, by using special microbial stains or polymerase chain reaction (PCR) or microscopy.3 IGH histology is characterized by focal accumulations of macrophages caused by the stimulation of helper T cells with undefined etiology making more complex the treatment strategy and presenting as main clinical manifestation a FUO.3,4 International literature has consolidated 18F-FDG-PET/CT as imaging tool of choice to evaluate patients with FUO, providing early diagnostic information. As a whole body imaging, it may highlights common causes of FUO such as infections, noninfectious inflammatory causes and tumors due to their high glucose turn-over identifying a potential lesion and helping in the etiological diagnosis.5 In our case, we described a FDG intense focal uptake in the hepatic segment VIII with a SUVmax of 22 and a bottom preferential uptake in the right liver. This finding led to a diagnostic biopsy getting the IGH diagnosis excluding a tumor or a lymphoma.
Conflicts of InterestThe authors declare no conflict of interest.
DisclosureNone.