Patients increasingly use social media to share and access health-related information and experiences. This study employed social media listening to gain patient-centric insights into metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD).
Materials and MethodPublicly available social media data was collected between November 4th, 2020, and November 4th, 2022, about MASLD from eight countries: Brazil, China, France, Germany, Japan, South Korea, Spain, and the United Kingdom. The analysis involved capturing patient conversations on their journey stages (causes-risk factors, symptoms, diagnosis, and treatment), unmet needs, and impact on patient's quality of life (QoL) from various social media platforms to gain insights associated with MASLD.
ResultsA total of 1600 patient-centric posts were analyzed. The patient journey was the most prevalent topic (92 %) mentioned, followed by comorbidities (38 %) and interactions with HCPs (26 %, health care professionals). Key causes discussed included unhealthy diet (39 %) and overweight/obese (32 %), while the most mentioned symptoms were fatigue (20 %) and pain or abdominal discomfort (20 %). Ultrasound (n=170/553, 31 %) was the most used diagnosis, followed by blood tests (n=130/553, 24 %) and liver function tests (n=91/553, 16 %). Lifestyle management techniques were mainly the standard of care, followed by treatment (n=270/1061, 25 %) and follow-ups with HCPs (n=133/1061, 13 %). Over half (54 %) of the QoL discussion (n=104/192) focused on patients’ comorbidities, and 27 % on disease severity, indicating that having MASLD in moderate to severe form with comorbidities significantly affects patients’ quality of life. An emotional analysis revealed that patients were worried and frustrated about their condition but were also hopeful and determined to improve their health. Nearly 38 % of the posts mentioned that patients were emotionally affected by negative feelings, especially those with multiple comorbidities. Lack of access to knowledgeable HCPs and treatment options were the most frequently discussed unmet needs.
ConclusionsThis analysis of NAFLD patient experiences introduces a unique approach for deriving insights into patients' experiences and their impact on QoL. These insights have the potential to complement conventional methods and foster patient-centric research.
Metabolic dysfunction-associated steatotic liver disease (MASLD), previously known as non-alcoholic fatty liver disease (NAFLD), is a spectrum of liver disease characterized by hepatic steatosis in the absence of other identifiable causes for secondary hepatic fat accumulation, such as excessive alcohol consumption [1,2]. MASLD global adult prevalence in adults has notably increased to 38 %, marking a +50.40 % rise from 25.26 % in 1990–2006. Latin America recorded the highest MASLD prevalence at 44.37 %, followed by East Asia at 29.71 % and Western Europe at 25.10 % [2].
MASLD, a heterogeneous condition, is often asymptomatic but can progress to severe stages like metabolic dysfunction-associated steatohepatitis (MASH) [3]. Furthermore, it is linked to an increased risk of cardiovascular disease (CVD) and continues to be a leading cause of advanced chronic liver disease, including primary liver cancer [4–6]. The complexity of MASLD management is compounded by under, or delayed diagnosis. Alarmingly, despite substantial progress in disease management, MASLD imposes a substantial burden from high socioeconomic costs [6,7] and an impaired health-related quality of life (HRQoL) [4,5]. Despite an extensive clinical burden, managing MASLD remains underdiagnosed, often relying on lifestyle modifications in many primary care settings [8].
Several qualitative and quantitative studies (questionnaire surveys, interviews, patient-reported outcomes) have explored the impact of MASLD and MASH on patients' lives, their unmet needs, and the burden of these conditions, including patient preferences for future therapies for NASH, lack of disease awareness, and efforts to improve quality of life (QoL) [9–13]. However, these studies were researcher-driven in controlled conditions.
In recent years, social media listening (SML) has emerged as a new approach for generating real-world evidence (RWE) by capturing unsolicited patient experiences [14]. This approach complements traditional surveys and enables us to gain insights into unprompted patient-centric discussions. Social media platforms, including discussion boards and Twitter, have increasingly become platforms for individuals to share disease-related experiences. Data from these platforms have been used to understand patients' journeys and unmet needs in various therapeutic areas [15–19]. The FDAʼs 2020 guidelines recognize social media as a method for gathering patient input [20] and the International Society for Pharmacoeconomics and Outcomes Research emphasizes the value of sourcing data from social media platforms to highlight pertinent issues for patients and their families [21].
This study aimed to understand the patient journey in MASLD by exploring the perspectives of stakeholders (patients, caregivers [a person who gives care to people who need help taking care of themselves], friends & family, and healthcare professionals [HCPs]). It also sought to describe insights into the quality of impact and unmet needs.
2Materials and methods2.1Study design and data sourceThis study was a non-interventional, retrospective analysis of data collected from social media platforms that were available in the public domain across eight countries: Brazil, China, France, Germany, Japan, South Korea, Spain, and the United Kingdom (UK).
A comprehensive search of social media content was conducted across various social media platforms, including Twitter, Forums, Blogs, YouTube, Instagram, and Facebook, from November 2020 to November 2022 using online aggregator tools, Talkwalker, Synthesio, and Fanpage Karma. To evaluate the sentiment of online posts, predefined search terms (NASH [non-alcoholic steatohepatitis], NAFLD [non-alcoholic fatty liver disease], MAFLD [metabolic associated fatty liver disease], fatty liver disease, steatotic liver disease) were used. The search terms were utilized in English and translated into seven languages: Brazilian-Portuguese, Chinese, French, German, Japanese, Korean, and Spanish (language and culture-specific disease terms were also incorporated). Additionally, these keywords were combined with other search terms related to treatment, causes, and comorbidities.
2.2Ethical considerationsAs this is a retrospective analysis relying on posts from publicly accessible social media platforms, no approval from an Institutional Review Board was required or obtained. However, all data utilized and presented in this study were without accessing password-protected information and in compliance with applicable data protection laws and regulations. All data were anonymized, in accordance with data privacy obligations.
2.3Data collection and analysisThe data collection and analysis occurred in two main stages:
- Stage 1.
Data collection: A total of 2,858,277 posts were identified using predefined search terms (Fig. 1). Subsequently, including those from bots, news blogs, junk, and spam, were removed from the raw dataset through the data cleaning and filtering functions of the aggregator tools.
- Stage 2.
Manual review, coding, and analysis: The cleaned and randomized dataset underwent manual review to filter the relevant and insightful posts, relating to the study focus topics. All posts were reviewed, across all platforms, to identify patient-centric, relevant, and eligible posts. The selection of 1600 as the sample size was predefined for robust analysis. To ensure uniform country-level representation, a country-wide weighted sample was selected for coding by country, as follows: n=300 for China and Japan, n=200 for Brazil, Germany, Spain, and the UK, and n=100 for France and South Korea (total n=1600).
Posts were coded and categorized according to defined themes, with multiple codes applied if posts discussed more than one theme and/or topic. These topics included: patient journey stages, challenges, interactions with HCPs, impact on QoL, and unmet needs. Data selection, coding, and analysis were conducted by experienced social data analysts, ensuring accuracy and consistency across the process. Uniform country-level representation was ensured through a country-wide weighted sample selection for coding.
2.4Study measuresInformation on key channels, disease terminologies, stakeholders, and clinical characteristics of patients with MASLD (e.g., comorbidities, severity/stage) was identified from reviewed posts and analyzed.
Data on demographics (e.g. age, gender, comorbidities) were recorded and analyzed when available. Gender was deduced from the user's name, or the content of the message, and categorized as unknown when not determinable.
The patient journey stages were analyzed by dividing into 4 stages: understanding causes and risk factors, recognizing signs and symptoms, diagnosis and tests, and ongoing treatment (improvement or worsening). Aggregate reporting through tools included mentions of challenges, symptoms, comorbidities, diagnosis, disease severity, and interactions with HCPs.
The emotional journey of the patients was mapped to patient journey stages and reported through different emotional outcomes (eg. joy, acceptance, determination). Additionally, the analysis involved examining patients' perceptions of the disease, quality of life (QoL), and unmet needs.
The records were classified as insights reported by possible patients or others either based on analysis of content (e.g. the direct mention of “self” within the content, without alluding to other subjects, was categorized as patient-reported insights; posts lacking first-person references but including mentions of a third person, such as a relative (e.g., husband, wife, son, daughter, etc.), were classified as insights reported by family members) or authors’ account information.
2.5Statistical analysisAll data were analyzed using descriptive statistics to find out the overall frequency of each activity. Categorical data were described using the number of posts and/or percentages.
3Results3.1Overview of social media postsOf the total 2,858,277 posts identified, ∼10,000 posts were reviewed across geographical regions (Brazil, China, France, Germany, Japan, South Korea, Spain, and the UK) to achieve the intended coding sample for the study. From this pool, a data sample of n=1600, derived from the defined stakeholders (patients, caregivers, friends & family, and HCPs), was selected as the basis for generating key insights.
The most common source of posts across regions was Twitter (65 %), followed by Forums (24 %). In China, Forums were the primary platform (85 %) through which patients engaged with HCPs. Patients (84 %) were the key stakeholder group, followed by HCPs (5 %) and caregivers (4 %) (Table 1).
Source, key stakeholders, and geographical distribution of posts.
| Total included posts, n (%) | 1,600 |
|---|---|
| Source | |
| 1,050 [65.6] | |
| Forums | 378 [23.6] |
| YouTube | 95 [5.9] |
| Xiaohongshu | 42 [2.6] |
| Blogs | 22 [1.4] |
| 9 [0.6] | |
| 4 [0.3] | |
| Stakeholders | |
| Patients | 1,343 [84] |
| Healthcare Professionals | 86 [5] |
| Caregivers | 60 [4] |
| Friends & Family | 43 [3] |
| Others | 68 [4] |
| Geographies | |
| China | 300 [19] |
| Japan | 300 [19] |
| UK | 200 [13] |
| Spain | 200 [13] |
| Brazil | 200 [13] |
| Germany | 200 [13] |
| France | 100 [6] |
| South Korea | 100 [6] |
In the majority of posts (77 %), the generic terms “fatty liver” or “fat in liver” were used to refer to the condition, regardless of disease type or severity. In Brazil, France, and Spain, the term “hepatic steatosis” was also utilized. Usage of the terms “NAFL” or “NAFLD” (n=180/1,600, 11 %) was more common in the UK (n=73/180, 41 %) and South Korea (n=36/180, 20 %).
3.2Patient demographics and characteristics, (n=230/1600)Patient gender was identifiable in 54 % of posts, with a majority being female (54 %) .
Patient age was identifiable in 14% of posts, with 60 % under and 40 % over 40 years of age. Notably, the UK posts showed a higher proportion of female patients (60 %) compared to other countries.
Comorbidities were discussed in 38 % of posts. Of the 857 mentions, cardiovascular disease (29 %), diabetes (26 %) and digestive disease (23 %) were more common comorbidities stated.
Among all posts discussing disease severity (24 %), 45 % of patients' expressed severity as mild. The distribution of “moderate” (38 %) and “severe” (39 %) individuals showed similar proportions.
3.3Understanding the patient journey, (n=1,479/1,600)In a comprehensive analysis of patient conversations across all regions, the patient journey emerged as the most prevalent topic, capturing the attention of 92 % of the total conversations. Among these patient stages, ongoing management (72 %) was discussed prominently. Fig. 2 depicts an empirical illustration of a patient's journey, encompassing four stages: risk factors, symptoms, diagnosis, treatment, and disease management, derived from social media posts with emotional outcomes.
Among the risk factors discussed, patients commonly cited an unhealthy diet (39 %), being overweight or obese (32 %), and the detrimental effects of medications (12 %). Regarding symptoms, fatigue (20 %) and abdominal discomfort (20%) were frequently mentioned by patients. The majority of patients (89 %) reported receiving a confirmed diagnosis, through a series of diagnostic tests including ultrasounds, blood tests, and liver function tests. Their diagnosis often began with abnormal results emerging from blood tests, prompting further investigation. Subsequently, through an ultrasound scan, a confirmed diagnosis brought clarity. Based on 160 mentions of challenges from 1479 posts, the major challenge discussed by diagnosed patients was the difficulty in adhering to lifestyle changes related to diet and exercise (64 %). Additionally, 18 % of patients expressed struggles in managing their condition through lifestyle adjustments. Other challenges included a lack of trust in HCPs due to a perceived lack of understanding or empathy, as well as feelings of frustration and disappointment when lifestyle changes did not yield improvements in weight or test results. Furthermore, some patients reported dissatisfaction with prescribed medications as they failed to improve their conditions.
The ongoing management stage involved a combination of treatment, lifestyle management techniques, and regular follow-ups with HCPs. Lifestyle management techniques, including dietary changes (64 %), exercise (46 %), weight loss management (29 %) were commonly adopted. Antidiabetic medication (10 %) was also used to treat MASLD liver. Further, supplements were the most discussed alternative treatment option across regions (46 %). When it comes to sentiments, alternative treatments were perceived positively due to efficacy and convenience, while antidiabetic medication showed the highest negative sentiment due to side effects, inefficacy and cost. Surgery (64 %) was positively reviewed for driving remission.
Patients discontinued their treatment due to the recovery from NASH/NAFLD/fatty liver, inefficacy and side effects. Disease improvement or recovery (16 %) was often expressed with joy. On the other hand, 3 % of posts mentioned disease worsening.
Examples of patient quotes of each category from the causes to ongoing management of the patient journey are provided in Supplementary Fig. S1.
3.4Understanding patient interactions with HCPs (n=419/1,600)A total of 419 posts detailed patients' sentiments following their interactions with HCPs across different stages of the patient journey. Among these, negative experiences with HCPs were predominant, being mentioned in 48 % of posts, while positive experiences were less frequently shared (26 %). Patients’ satisfaction with HCPs stemmed from clear communication, empathy, and a proper diagnosis. Although patients felt confident with their interactions, few patients conveyed a lack of empathy, not satisfied and happy with the suggestions, prompting them to look for online peer opinion after consultation (Fig. 3).
Despite patients feeling confident in their interactions, some expressed a lack of empathy and dissatisfaction with the suggestions. As a result, they sought online peer opinions after the consultation (Fig. 3).
3.5Understanding the emotional journey, (n=1,600)Over 1,600 disease mentions from patients were identified for this analysis.
Determination was the key emotion expressed in NASH/NAFLD/fatty liver conversations. Being neutral and being worried about the disease were the most frequently identified emotions. Frustration was expressed the most during the causes and risk factors stage. A feeling of worry was identified more often during the signs and symptoms and diagnosis and test stages. Positive emotions of hopefulness, relief, and joy were mainly expressed when patients witnessed the improvement of the condition (Fig. 2).
3.6Impact on QoL, (n=192/1,600)A total of 12 % of the records discussed the impact on quality of life (QoL), with emotional QoL (64 %) being the primary aspect followed by functional (34 %), social (17 %), and financial impact (4 %) (Fig. 4). Over half (54 %) of the quality-of-life impact discussion highlighted the presence of comorbidities and 27% with the severity/disease stage mentions (data not shown). Among the emotional QoL impact, 38 % of posts mentioned patients were emotionally affected by negative feelings, particularly those with multiple comorbidities. Among physical/functional impact, 55 % of posts mentioned patients experiencing pain, followed by fatigue/tiredness (38 %) being the most common. Social impacts (17 %) were also discussed, primarily related to work and employability (48 %) (Fig. 4). Financial impact was minimal (4 %), with only a few posts mentioning decreased QoL, financial support, and treatment due to their ability to work being is affected.
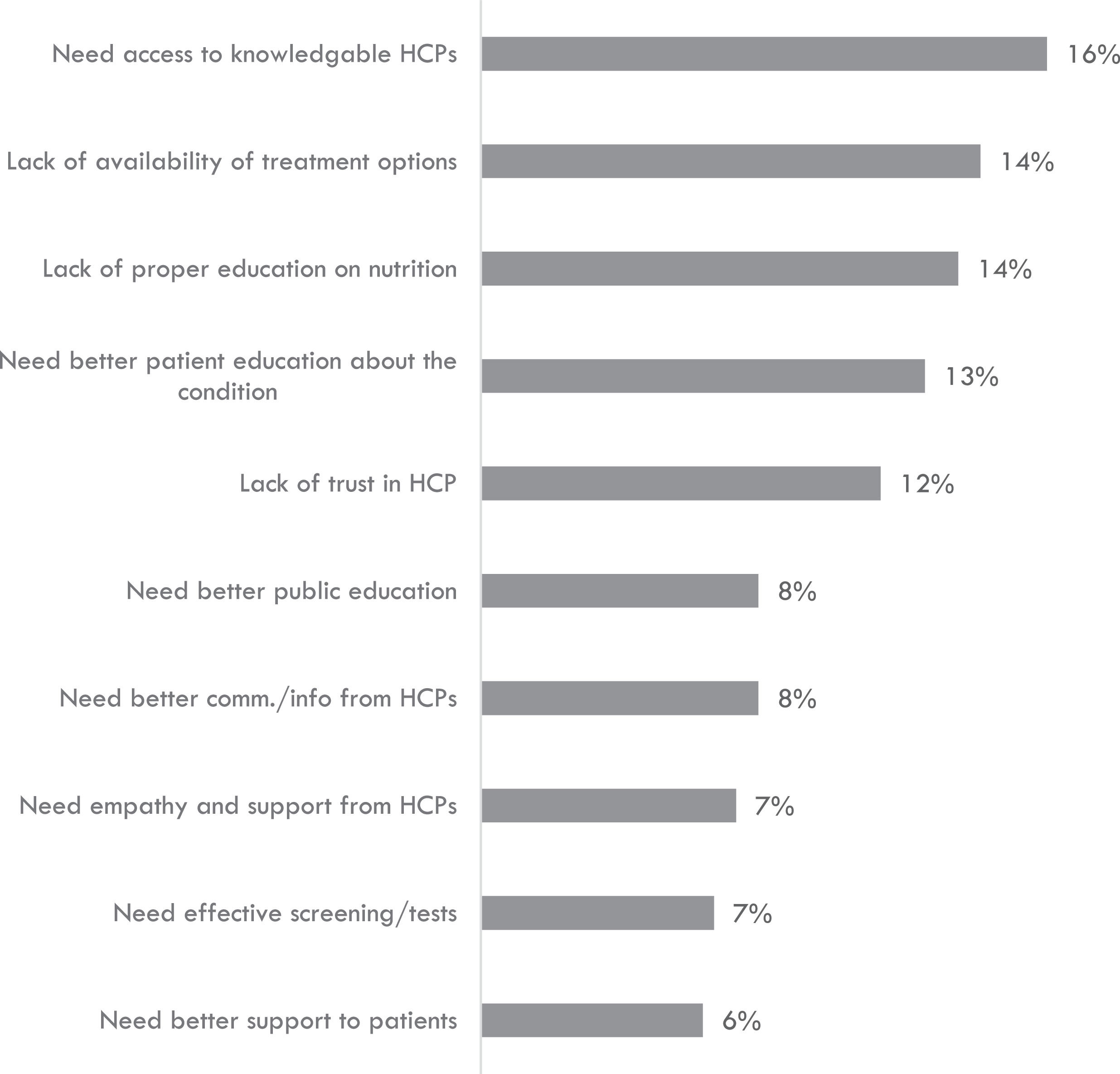
3.7Understanding key unmet needs, (n=311/1,600)The unmet needs revealed insights into the understanding of patient journey stages, treatment access, and diagnostic challenges among individuals living with MASLD. Access to knowledgeable HCPs (16 %), limited availability of treatment options (14 %), and a lack of patient education about the condition (14 %) were identified as the primary unmet needs (see Fig. 5).
Patients voiced several unmet needs related to their treatment. Firstly, they expressed worries about the lack of treatment options beyond dealing with potential side effects. Additionally, they highlighted alternative and management-related unmet needs, indicating a desire for more effective and feasible treatment options. Furthermore, patients conveyed a lack of trust and a strong need for knowledgeable and improved communication from HCPs. Another unmet need centered around the requirement for effective screening tests as part of their diagnosis-related necessities (Supplementary Fig. S2).
3.8Country specific insightsOverall, the study findings were generally consistent across the focused countries, with a few noticeable regional-level differences. In Germany, the causes and risk factors stage garnered the most discussion, whereas the ongoing management stage mentions topped in all other regions. The overall interaction with HCPs was found to be negative across all regions, while Spain exhibited the highest proportion of HCPs discussing the condition. Ultrasound was the most mentioned diagnostic test type across the European markets, and the majority of posts referenced antidiabetic medication in those markets. Interestingly, Chinese media posts mentioned alternative treatment as a key treatment option, with a focus on traditional herbal medicine and patent medicine. Expressions of joy related to disease improvement or recovery were common across all regions, especially among patients in China and Germany. Unmet needs, particularly those related to treatment and HCPs, were frequently identified in European countries. Japanese patients commonly expressed a lack of proper education on nutrition as a key unmet need.
4DiscussionThis study marks the first-use of data from broader social media platforms, complementing previous research on emotions and stigma related to the disease [22].
Listening to real-time patient voices through SML is distinct from traditional survey studies. This study utilized, SML, acknowledged by the FDA as a valid method for capturing unfiltered real-time disease and treatment experiences of patients [23]. On the other hand, survey studies offer structured, standardized in-depth information from targeted samples within controlled environments. While both methods have their strengths, they are often used in combination to gain a comprehensive understanding of a topic or community.
Posts related to the journey of patients with MASLD primarily focused on disease management, testing and diagnosis, as well as causes and risk factors. The study's findings revealed that unhealthy diets, overweight/obesity, and harmful medication effects were the most frequently discussed causes and risk factors. However, patients also expressed that effectively managing their condition was hindered by inadequate support and communication from HCPs.
The study results align with and validate a few of the findings from previous non-SML research on MASLD [24–26]. For instance, earlier studies have highlighted that an unhealthy lifestyle, characterized by an unhealthy diet and a lack of physical activity, was considered a significant factor in the development of the disease. These studies also emphasized the considerable impact of the disease on patients' quality of life. Moreover, the indiscriminate use of the generic term fatty liver and infrequent use of specific medical terms such as NAFLD, NASH, and MAFLD by patients, regardless of their disease stage, points to a lack of awareness regarding the progressive nature of the disease. This gap in understanding was noted in both this study and in previous qualitative and quantitative research focused on comprehending the patient's perspective on the disease [24,26]. Additionally, this study revealed that patient frustrations stemming from communication gaps with HCPs manifested in an overall negative sentiment towards their interactions, a lack of trust in the HCPs, and dissatisfaction with the guidance and support in managing the condition. These sentiments mirror those observed in previous studies, indicating a consistent lack of effective communication between HCPs, leading to significant knowledge gaps among patients.
While non-SML observational studies primarily focused on patients aged between 40 and 60 [24,25], it is noteworthy that the most prevalent age groups in this study were in their 20s and 30s, signaling a greater tendency for younger generations to frequently utilize social media platforms [27].
While discussing ongoing disease management, patients often viewed lifestyle techniques, specifically dietary modifications and regular exercise, as the primary methods for doing so. The overarching issue of insufficient HCP involvement in condition management, including nutritional education and the oversight of alternative treatments like dietary supplements, underscores potential areas where HCP support, education, and interventions are lacking. To address these gaps, we propose promoting open communication, enhancing HCP education, establishing clear guidelines, encouraging multidisciplinary approaches, and utilizing technology and events for education. These measures aim to ensure a more comprehensive and evidence-based approach to patient care.
Emotional support is crucial for patients, especially those in severe disease stages, due to factors like the lack of MASH-specific treatment and their sense of loss around their health. Nonetheless, despite the hopelessness that patients may feel, it is important to recognize that they can also often remain motivated to manage their condition once diagnosed. HCPs can thus seize this opportunity to leverage patients' determination by providing better communication and guidance to empower them to adopt a more proactive approach to lifestyle management and engage relevant stakeholders [28] in the process.
Overall, the study findings remained consistent across the focus countries, although some variations were noted. Patients in Asian countries often mentioned receiving early diagnoses due to annual health checkups provided by local governments and mandatory health screenings for employment, while late diagnoses were more frequently reported among European patients. Furthermore, patients from Brazil, France, and the UK expressed a greater need for empathetic and supportive HCPs, citing dissatisfaction with the level of support received in managing their condition and a lack of clear guidance or advice post-diagnosis. To enhance education and support from HCPs, multiple approaches can be adopted, including utilizing educational avenues such as health conferences, workshops, and webinars to engage both future and practicing HCPs.
4.1LimitationsIt is important to note that this study primarily represents internet users, mainly younger generations, and may not provide a comprehensive view of the entire patient population. Nonetheless, it offers a valuable opportunity to gain insights from age groups that have previously been overlooked. Furthermore, findings on patients’ disease management challenges and needs, no matter their age, can help to inform the development of more effective, patient-centered MASLD and MASH interventions [29].
Access to some social media platforms was limited due to a lack of application programming interface (API) access. For instance, TikTok and LinkedIn data were not accessible. Furthermore, Instagram and Facebook data were obtained through official APIs, which were limited to public pages only and did not include posts by individual users or closed media channels. Therefore, the data gathered in this way does not comprehensively represent all patient experiences from these channels.
The unstructured and unsolicited nature of the data gathered and analyzed via social media listening, as opposed to traditional market research methods like surveys and focus groups, can make it challenging to derive structured insights and may introduce biases due to the lack of control over the information being shared.
5ConclusionsIn summary, some patients with MASLD are actively sharing their experiences and seeking information on social media. This study provides unfiltered insights into patients’ experiences with the disease, covering areas such as positive lifestyle modifications, coping with the emotional impact, and finding supportive HCPs. These insights underscore the significance of enhancing HCP empathy and support, offering better nutritional information, and improving treatment options to assist patients in managing their condition. Such insights can inform better patient care strategies and guide future studies focused on better-understanding patient perspectives, ultimately aiding the healthcare community in developing more effective ways to support and manage people living with MASLD.
FundingThis study was funded by Novo Nordisk Healthcare.
Author contributionsAll authors contributed to the design of the study, participated in the interpretation of the data, and drafting of the manuscript. All authors reviewed and approved the final, submitted version.
Medical writing support was provided by Rekha Raghuram, MSc., from Novo Nordisk Global Business Service India, Global Medical Affairs, Bengaluru, India. Analysis and insight generation support was provided by Abhinab Bhanja, Head of Pharma Insights, Convosphere, India.