Acute liver failure is a rare but often catastrophic illness affecting the liver and multiple organ systems. Patients with acute liver failure require a multidisciplinary approach for adequate management. With improved critical care and the availability of liver transplantation, survival has significantly improved. Hepatic encephalopathy, cerebral edema and infections are the most common complications of acute liver failure. The evaluation requires a diligent search for a specific etiology of the liver failure, since certain causes may respond well to specific pharmacological therapies. Acetaminophen and non-acetaminophen drug-induced hepatotoxicity account for more than 50% of cases of acute liver failure. Assessment of prognosis frequently (at least on a daily basis) by using various prognostic tools, allows the treating team to decide whether or not to proceed with urgent liver transplantation. Artificial liver support devices are still in evaluation and not ready for use in clinical practice. While it is determined whether or not there is sufficient hepatic regeneration, the care of the patient with acute liver failure revolves around managing the dysfunction of multiple extra hepatic systems.
Acute liver failure (ALF) is an uncommon but complex and often catastrophic illness manifesting as coagulopathy (International Normalized ratio, INR ≥ 1.5) and altered mental status (hepatic encephalopathy) due to rapid decline of liver function in a patient without preexisting liver disease. The onset and duration of illness must be less than 26 weeks duration.1 ALF is a challenging medical emergency requiring immediate attention. Progression is associated with multiple organ failure and need for urgent liver transplant, a life-saving option for many ALF patients. The incidence of ALF in the U.S. is estimated at 2,000 to 2,800 cases per year.2,3 Survival rates without liver transplant range from 10 to 40% in different centers. Survival has improved to more than 70% and reaching 90% in some studies with liver transplantation, with short-term survival exceeding 65%.2 No racial disparities with respect to mortality in ALF managed at tertiary care centers across the U.S. are observed.4 The etiology of ALF plays an important role in the management and survival of patients with ALF (see below).
Terms previously used to describe ALF included fulminant hepatic failure, fulminant hepatitis or acute hepatic necrosis. Others have described subtypes based on the time interval of onset of jaundice to the development of hepatic encephalopathy, which may be of some prognostic significance. Thus, hyperacute liver failure (< 7 days), acute (7-21 days) and subacute (> 21 days and < 26 weeks) have been proposed. However, this terminology has not been generally adopted. Hyperacute cases due to acetaminophen toxicity may have a better prognosis.5 In general, the more acute the onset of ALF, the less hepatic fibrosis and better chances of hepatic regeneration, however, with greater incidence of cerebral edema.
EtiologyAcetaminophen hepatotoxicity and idiosyncratic drug reaction account for a majority of ALF cases at 39% and 13% respectively in U.S.6 It is hypothesized that host genetic, immunologic, and environmental factors are important in the pathogenesis of drug-induced liver injury (DILI),6 which accounts for 13% of ALF.6 Acetaminophen causes a dose-dependant hepatic injury and is currently more commonly seen after unintentional overdose (OD) than intentional. Unintentional OD may cause ALF in alcoholics with even as little as 4 g/day. N-acetyl-p-benzoquinone (NAPQI), a toxic metabolite of acetaminophen covalently binds to hepatocytes, a process which is potentiated by chronic alcohol induction of P-450. Serum acetaminophen levels are not useful in ALF related to unintentional overdose.
Many prescribed and over the counter medications, nutritional supplements and herbal supplements may cause ALF.6 Other commonly implicated agents include HAART, anticonvulsants and isoniazide; methylenedioxymethamphetamine (MDMA, ectasy), an abused recreational drug has also been associated with ALF.7 A partial list of drugs which may cause ALF is shown in table 1.8 These agents cause liver injury by mechanisms such as binding to cytochrome system molecules, oxidative stress, mitochondrial toxicity, hepatocyte membrane dysfunction, immune modulation to initiate an autoimmune process, bile duct damage, allergic reaction, etc.8 About 15 to 20% of ALF occur due to no detectable cause in spite of intensive investigations. About one fifth of ALF of indeterminate cause is related to hidden acetaminophen toxicity.9 Underlying liver disorders such as chronic alcoholism increase the risk of ALF, and coexisting diabetes is an independent risk factor.6 Mushroom ingestion has been well documented as a cause of ALF, and recent reports describe ALF associated with the use of large amounts of Chinese green tea (Camellia sinensis).6,10
Drugs causing FHF.
| Analgesics/Anti-pyretics/Anesthetics |
| • Acetaminophen |
| • Aspirin |
| • Halothane |
| Antimicrobials |
| • Antituberculosis Therapy |
| Isoniazid Rifampicin Ethambutol Streptomycin Pyrazinamide Antibiotics Beta lactam antibiotics Ampicillin, Amoxicillin, Clavulanic acid Tetracyclines Minocycline Erythromycin, Roxithromycin Sulfonamides |
| • Antifungal |
| Ketoconazole, Itraconazole, Fluconazole |
| • Antiepileptics |
| Carbamazepine, Felbamate, Lamotrigine, Oxcarbamazepine, Phenobarbital, Phenytoin, Valproic acid, Vigabatrin. |
| • Recreational drugs |
| Marijuana, Hashish, Cocaine, Amphetamines. |
| • Slimming agents |
| Ma huang, Usnic acid, Chaso, Onshido, etc. |
| • Herbal agents (many to enumerate). |
| Miscelaneous |
| • Lisinopril, Disulfuran, Amiodarone, Metformin, Diclofenac, Nicotinic acid, Labetalol, Imipramine, Etoposide, Flutamide, Tolcapone, Allopurinol, Methyldopa, Gemtuzumab. |
Viral etiology as a cause of ALF has become relatively less common. Hepatitis B and hepatitis A account for 8% and 4% of ALF respectively.5 Hepatitis C does not appear to cause ALF.5 The utility of antihepatitis B nucleoside analogs for the treatment of ALF due to acute hepatitis B infection is controversial. In a recent review by the U.S. Acute Liver Failure Study Group, nucleoside analogues were not recommended in the treatment of HBV-related ALF.5 Patients with positive HBsAg on any type of immunosuppression are required to be treated prophylactically with a nucleoside analog to prevent reactivation of hepatitis B virus. Hepatitis E virus is of concern to cause ALF in endemic areas like Russia, Pakistan, Mexico or India, and tends to be severe in pregnant women.5 Herpes simplex virus infection is a rare cause of ALF, more so in immunosuppressed and pregnant women (in the third trimester).5 Skin lesions are observed in only about 50% of cases.5 Diagnosis is possible by serum Herpes DNA and liver biopsy. Acyclovir is initiated for suspected or diagnosed cases.5 Acute hepatitis D virus infection may be diagnosed in hepatitis B infected persons. Cytomegalovirus (CMV), Epstein Barr virus (EBV), Herpes Varicella Zoster (HVZ), adenovirus, hemorrhagic fever viruses are occasionally implicated as causes of ALF.
Metabolic disorders like acute fatty liver of pregnancy, Wilson’s disease, Reye’s syndrome, galactosemia, hereditary fructose intolerance, and tyrosinemia may cause ALF. Right heart failure, Budd-Chiari syndrome, veno-occlusive disease, ischemic hepatitis and heat stroke are among the vascular causes of ALF. Miscellaneous conditions such as metastatic malignant infiltration with lymphoma, autoimmune hepatitis can cause ALF. About 17% of ALF of undetermined cause may include non A-E viral hepatitis, other drug toxicity, and possibly unrecognized metabolic and genetic diseases.
Clinical Presentation and ManagementAdvanced ALF often involves dysfunction of multiple organ systems. The presenting symptoms of ALF are frequently non-specific and include fatigue, malaise, anorexia, abdominal pain, fever and jaundice. These symptoms progress in no particular order to coagulopathy preceding the development of encephalopathy, both of which are the hallmark of ALF. ALF should be managed in an ICU at a tertiary care center because of the unpredictable and rapid manner in which patients may deteriorate. Frequent neurological and hemodynamic monitoring is of primary importance.11 Multidisciplinary involvement including hepatologist, liver transplant surgeon, intensivist, psychiatrist, and social worker are required. If the patient is not at a tertiary care center with liver transplant capabilities, then early transfer should be acomplished. N-acetylcysteine (NAC) is established as a proven benefit for acetaminophen induced hepatotoxicity.11 The preferred mode of administration is intravenous, for as long as necessary to observe unequivocal improvement. NAC, due to its antioxidant effects and improvement of tissue oxygenation, has also been suggested to be beneficial in non-acetaminophen ALF. A recent multicenter double-blinded study showed benefit only in ALF patients with early, grade 1 and 2 hepatic encephalopathy.12 Metabolic causes such as Wilson’s disease and autoimmune hepatitis are often treated with emergency liver transplantation. In a recent study, steroids did not improve survival in drug induced, cryptogenic or autoimmune ALF.13
Hepatic Encephalopathy (HE) and Cerebral EdemaClinical manifestations of HE and cerebral edema can be overlapping making their diagnosis difficult. This is important because the treatment modalities are different. The severity of hepatic encephalopathy is not only a diagnostic criterion but also a prognostic indicator in ALF. Toxic substances (ammonia, benzodiazepine agonists, manganese, aromatic amino acids, mercaptans, phenols, short-chain fatty acids) absorbed from the bowel lumen are not efficiently detoxified by the liver. These toxins become available systemically and to the brain causing astrocyte swelling, leading to encephalopathy.14,15 HE is staged based on the subject’s neurological status,1 the West-Heaven classification of HE severity, as indicated on table 2.16 HE is a reversible metabolic derangement and less often fatal than cerebral edema. Cerebral edema can complicate ALF, and may confound advanced encephalopathy. Increased cerebral blood flow with impaired cerebral autoregulation and astrocyte swelling are implicated in cerebral edema, which may contribute to ischemic and hypoxic brain injury.5 The pathophysiology has not been fully identified but cytotoxic and vasogenic mechanisms have been suggested.16 Cerebral edema may be clinically recognized by systemic hypertension and bradycardia (Cushing reflex), decerebrate posturing or rigidity, disconjugated eye movements, and loss of pupillary reflex. Intracranial pressure (ICP) monitoring is used in the intensive care setting and requires a cooperating neurosurgeon, but it is the only mean to diagnose early intracranial hypertension17 and assess the efficacy of therapeutic measures. ICP is monitored by placement of an epidural or subdural sensor. ICP more than 25 mm of Hg, or cerebral perfusion pressure (CPP) of less than 50 mm of Hg, indicate reduced neurological blood flow to maintain intact brain function. CPP less than 40 mm of Hg for over 2 hours is considered a contraindication for orthotopic liver transplant due to poor prognosis post-transplantation.3,10 Jugular venous oxygen content difference may provide an indirect assessment of cerebral blood flow and oxygen consumption.16 The suggested goal is to maintain jugular venous blood saturation between 55-80%.18 The risk of cerebral edema increases to 25 to 35% with the progression of HE to grade 3, and 65 to 75% in patients with grade 4 HE.5 Uncal herniation is an uniformly fatal consequence of cerebral edema. Various treatment measures have been used for, among which mannitol is the mainstay. Barbiturates are used when most measures have not worked, often in extreme conditions.
Stages of Hepatic Encephalopathy (HE).
| Stage | Neurological status | Tremors | EEG |
|---|---|---|---|
| I | Euphoria; occasional depression; fluctuant mild confusion; slowness of mentation and affect; untidy; slurred speech; disorder in sleep rhythm. | Slight | Usually normal |
| II | Accentuation of stage I; drowsiness, but easily arousable; inappropriate behavior; able to maintain sphincter control. | Present and Easily elicitable. Flapping tremor. | Abnormal; Generalized slowing |
| III | Sleeps most of the time but is arousable; speech is incoherent; confusion is marked. | Usually present if patient can cooperate | Always abnormal |
| IV | Not arousable; may or ay not respond to painful stimuli. | Usually absent | Always abnormal |
The grade of encephalopathy generally determines the type of toxin-reducing agents used. Grade 1 and grade 2 HE patients can tolerate oral agents, while grade 3 and 4 HE patients generally need respiratory assistance. Rifaximin, an oral non-absorbable antibiotic has been an increasingly used agent for the treatment of HE. It can be given through a nasogastric tube as well. It acts by suppressing the bowel flora, reducing the production of absorbable toxins such as ammonia. Oral lactulose has long been used to reduce ammonia absorption by trapping ammonia in the bowel, consequently causing undesirable bowel distention and ileus. Its use as enemas is preferably restricted to HE grade 3 and 4.
Entities that can worsen HE include sepsis, gastrointestinal bleeding, hypoglycemia, hypoxemia and electrolyte abnormalities. These should be promptly identified and treated. The need for CNS depressants to control agitation may mask the prognostic value of the severity of HE. In such situations, assessment of improvement should be monitored by serial measures of prothrombin time (PT), bilirubin, Factors V and VII levels, dextrose requirement, clinical condition and complications.
Cerebral edema has a major prognostic role and is a common cause of mortality in ALF. Prompt recognition and treatment is vital. Prophylactic treatment for cerebral edema has no role at this time. The goal is to maintain ICP less than 20 mm of Hg and CPP of > 50 to 60 mm of Hg at all times.9 Factors that increase ICP need to be avoided and include high positive end-expiratory pressure, frequent movements, neck vein compression, fever, arterial hypertension, hypoxia, coughing, sneezing, seizures, head-low position and respiratory suctioning. Prophylactic intravenous lidocaine may be of value to prevent consequences of Valsalva maneuvers.11 Active interventions for the management of cerebral edema include head elevation up to 30 degree, maintain neutral neck position, avoid or minimize painful stimuli, hyperventilation to maintain PCO2 between 30-35 mm Hg, control of arterial hypertension, mannitol infusion and avoid fluid overload.9 ICP of more than 20 mm of Hg necessitates the use of mannitol provided serum osmolality is less than 310 mOsm/liter.9 Repeat mannitol boluses may be required for persistent increase in ICP. There is no role for mannitol if serum osmolality is more than 320 mOsm/liter. Mannitol is less effective if ICP is greater than 60 mm of Hg; its best use is for mild to moderate ICP. If the patient is anuric and has renal failure, dialysis must accompany mannitol use. About one fifth of the patients might respond paradoxically, with an increase in ICP following mannitol. For this reason, the early ICP response to mannitol must be assessed carefully. Those patients who do not respond (50%) or have contraindications for the use of mannitol may be treated with continuous intravenous infusion of barbiturates. CPP in response to treatment should guide the infusion rate with the goal to achieve a suppression pattern on EEG. At no point during this therapy should one entertain the diagnosis of brain death as the effects of barbiturate coma manifest similarly with the loss of brain stem reflexes. Moderate degrees hypothermia of 33 to 35 degree C has shown some benefit in preliminary series. However, hypothermia for ALF remains experimental at this time.19
Vasopressive treatment may be necessary to maintain an adequate CPP. Before dropping the patient off the transplant list, it is prudent to confirm uncontrollable intracranial hypertension and perform nuclear cerebral perfusion scan as confirmatory evidence of compromised cerebral function and/ or brain death.
Hypertonic saline to target serum sodium levels between 145 to 155 are suggested but also need further study.11 Vasopressors and hepatectomy have been used with varying success.20
CoagulopathyThe liver has a central role in the synthesis of most coagulation factors and some inhibitors of coagulation and fibrinolysis.16 Deficiencies of fibrinogen, factors II, V, VII, IX and X, and platelet are often present in ALF. Reduced levels of coagulation inhibitors such as antithrombin, protein C, and protein S fail to completely balance their effect on coagulopathy.16,21 Consumption of clotting factors and platelets occur especially when associated with disseminated intravascular coagulation. These derangements are manifested as prolongation of prothrombin time, which is widely used as an indicator of the severity of hepatic injury. Infusion of fresh frozen plasma is indicated only for control of active bleeding or during invasive procedures such as insertion of intracranial pressure monitor, to maintain an INR < 1.5.11 Cryoprecipitate can be administered if fibrinogen levels are < 100 mg/dL.10,11 Platelet transfusion is indicated only to aid in controlling active bleeding or during invasive procedures if the count is < 50 x 109/L or prophylactically if < 10-20 x 109/L.10 Increased ICP due to volume overload is a concern with liberal transfusion of blood products. Factor VII replacement is promising but in need of further studies to assess its safety. Vitamin K, 5 to 10 mg subcutaneous should be administered to correct any underlying vitamin K deficiency. Risk factors for gastrointestinal bleeding include mechanical ventilation for more than 48 hours and coagulopathy in critically ill ALF patients. Other risk factors include renal failure, sepsis and shock.5 Proton pump inhibitors and H2 blockers have been proven to be effective in decreasing the risk of significant bleeding.5
Renal Failure and HemodynamicsAcute renal failure is multifactorial in the setting of ALF. Acute renal failure denotes a poor prognosis and contributes to mortality.5 Hypovolemia, low systemic vascular resistance, acute tubular necrosis (ATN), GI blood loss and hepatorenal syndrome are among the most important associated entities.5 Acid-base derangements and lactic acidosis are particularly common in acetaminophen toxicity and denote a poor prognosis.11 Prompt fluid resuscitation with crystalloids for low arterial pressure, or colloids in pre-hepatorenal syndrome along with midodrine and octreotide, have been suggested. Renal toxic agents should be avoided. In situations not responding to volume resuscitation, inotropic or pressor support may be required to maintain a mean arterial pressure of 50-60 mm of Hg. An optimal systemic arterial pressure is desired to avoid detrimental effects on CPP as discussed earlier. Dopamine is associated with increased systemic delivery of oxygen, but others like norepinephrine and epinephrine should be used as needed, to maintain vital organs perfusion. Worsening renal failure needs to be addressed with continuous veno-venous dialysis to avoid further hypotension. Citrate anticoagulant may be preferred over heparin.
InfectionInfectious complications are a leading cause of mortality in ALF patients. 80% develop bacterial, and about 20 to 30% of patients develop fungal infection during hospitalization.11 High vigilance with blood cultures, urine cultures and sputum cultures must be performed at admission and as indicated clinically. Particularly, venous line infection has to be looked for in these patients. All ALF patients with ascites, unexplained fever and leukocytosis need a diagnostic paracentesis. Broad spectrum antibiotics (quinolones or third-generation cephalosporin) are generally used to cover common organisms such as staphylococcal species, streptococcal species, or gram-negative rods. Poorly absorbed oral antibiotics to decontaminate the bowel have not shown survival benefit. Empirical broad-spectrum antibiotics should be administered to patients with acute liver failure who develops signs of systemic inflammatory response syndrome, or unexplained progression to higher grades of encephalopathy.22 Prophylactic antibiotics are not recommended in spite of the speculation that they reduce infection and the fever impact on ICP.5
Nutritional and MetabolicALF is a high catabolic state and maintaining adequate nutrition is important. Early enteral feeds should be initiated. If enteral feeds are contraindicated, parenteral nutrition is an option although associated with risk of line infections. Adequate nutrition with 1–1.5 g of protein/Kg body weight, preferably with branched chain amino acids is recommended. Caloric goal for patients with ALF should be approximately 25 to 30 kcal/kg/d.10 Early nutrition may reduce the risk of stress induced gastrointestinal bleeding in critically ill patients. Involvement of a nutritionist may be considered. Hyperglycemia should be avoided, because it impairs control of ICP.10 Hypoglycemia can confound the hepatic encephalopathy and should be managed with continuous infusion of 5 or 10% glucose along with frequent monitoring. Hyponatremia is a poor prognostic indicator and the desirable levels are above 125 mEq/L. Phosphate, potassium and magnesium are frequently low, requiring repeated supplementation.
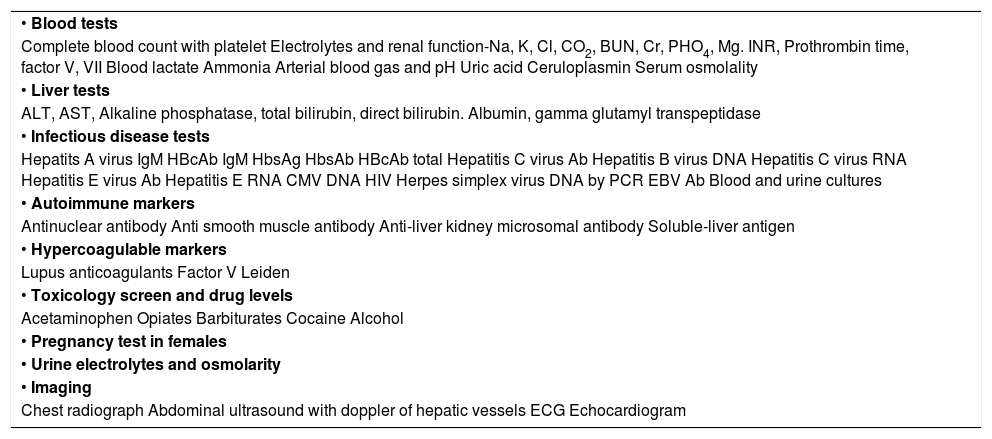
Evaluation of Patients with ALFA through work up of patients with ALF is important. Not only does the etiology help in management but also serve in predicting the prognosis and potential need for liver transplant. A suggested list of baseline testing is presented in table 3.10
Evaluation of ALF.
| • Blood tests |
| Complete blood count with platelet Electrolytes and renal function-Na, K, Cl, CO2, BUN, Cr, PHO4, Mg. INR, Prothrombin time, factor V, VII Blood lactate Ammonia Arterial blood gas and pH Uric acid Ceruloplasmin Serum osmolality |
| • Liver tests |
| ALT, AST, Alkaline phosphatase, total bilirubin, direct bilirubin. Albumin, gamma glutamyl transpeptidase |
| • Infectious disease tests |
| Hepatits A virus IgM HBcAb IgM HbsAg HbsAb HBcAb total Hepatitis C virus Ab Hepatitis B virus DNA Hepatitis C virus RNA Hepatitis E virus Ab Hepatitis E RNA CMV DNA HIV Herpes simplex virus DNA by PCR EBV Ab Blood and urine cultures |
| • Autoimmune markers |
| Antinuclear antibody Anti smooth muscle antibody Anti-liver kidney microsomal antibody Soluble-liver antigen |
| • Hypercoagulable markers |
| Lupus anticoagulants Factor V Leiden |
| • Toxicology screen and drug levels |
| Acetaminophen Opiates Barbiturates Cocaine Alcohol |
| • Pregnancy test in females |
| • Urine electrolytes and osmolarity |
| • Imaging |
| Chest radiograph Abdominal ultrasound with doppler of hepatic vessels ECG Echocardiogram |
The etiologies of ALF are the same as in non-pregnant individuals but some are specific to pregnancy. Viral hepatitis is the most common and accounts for 40% of jaundice during pregnancy. The outcome of acute fulminant hepatitis E virus infection in pregnancy is poor for unknown reasons. Up to 25% of these tend to become fulminant with high mortality and probably influenced by malnutrition. Diagnosis is made by serology and serum hepatitis E RNA by PCR. Supportive care is advocated and termination, caesarean, or discouragement of breast feeding are not indicated. Hepatitis E is rare in U.S. but endemic in Asia, Africa, and Central America.
HELLP syndrome is a complication of severe preeclampsia and manifests as hemolysis (H), elevated liver tests (EL), and low platelets (LP). Treatment includes emergent delivery which is the only definitive treatment, along with antepartum stabilization of hypertension and DIC, seizure prophylaxis and fetal monitoring. Pregnant ALF patients might require caesarean section.23
Acute fatty liver of pregnancy is a sudden catastrophic illness occurring mostly in the third trimester, where metabolic disruption in the fetus causes microvesicular fatty infiltration in the mother resulting in encephalopathy and hepatic failure.10 It is precipitated by abnormal intramitochondrial fatty acid oxidation. Early recognition with immediate termination of pregnancy and intensive supportive care is essential for maternal and fetal survival.23
Prognosis In Acute Liver FailureMany systems to assess the prognosis of ALF have been proposed (Table 4).24 Due to the involvement of multiple organ systems in ALF, the predictive ability of survival in ALF is limited.
Prognostic indices used in ALF.
| King’s College Criteria (KCC):24 |
| • Acetaminophen |
| ° Arterial pH < 7.30 or |
| ° All of the following: |
| INR > 6.5 S. Creatinine > 300 μmol/L Grade 3 or 4 encephalopathy |
| • Non-Acetaminophen |
| ° INR > 6.5 or |
| ° 3 of the following |
| Age < 10 or > 40 years Non-A/non-B hepatitis, drug induced ALF Duration of jaundice to encephalopathy > 7days INR > 3.5 S. bilirubin > 300 μmol/L |
| Other prognostic systems in ALF:24 |
| • Clichy criteria |
| • MELD |
| • Edinburgh (non-acetaminophen) |
The King’s college criteria (KCC) were developed from a combined retrospective cohorts of patients with ALF who were medically managed. Variables were selected for acetaminophen and nonacetaminophen induced ALF. In the acetaminophen group, arterial pH < 7.3 or INR > 6.5, serum creatinine of > 3.4 mg/dL, and grade 3 or 4 encephalopathy had prognostic significance. In nonacetaminophen group, INR > 6.5 or three or more of the following five were independent outcome predictors:
- i.
Unfavorable etiology (non-A, non-B, Drug induced liver injury [DILI]),
- ii.
Jaundice for more than 7 days prior to encephalopathy,
- iii.
Age under 10 years or over 40 years,
- iv.
INR higher than 3.5,
- v.
Serum bilirubin > 17.5 mg/dL.
Generally, KCC faired better than Paris, Birmingham and Pittsburg models.24
Etiology of ALFCertain etiologies of ALF have shown poorer outcomes. Idiosyncratic drug injury, acute hepatitis B, autoimmune hepatitis, mushroom poising, Wilson’s disease, Budd-Chiari syndrome and indeterminate causes are among those to have an undesirable outcome.
Severity and onsetThe severity of encephalopathy (grade 3 and 4), associated with cerebral edema and coagulopathy have inverse correlation with survival. Time from jaundice to encephalopathy were previously proposed but not substantially proven to predict survival of ALF.
Model for End-Stage Liver Disease (MELD)In spite of the widespread use of this tool in chronic liver disease patients, MELD has not shown the same conclusive benefits in ALF patients.24 The MELD score is undergoing further evaluation in ALF at this time.
Other criteria have shown less promise include the Clinchy criteria, APACHE II, lactate, Gc globulin and factor V. Prothrombin time and renal failure are reasonable monitoring tools to follow improvement. Phosphate levels, cytokines, arterial ammonia and adrenal function are additional targets for further study.5,15 Alpha-feto protein (AFP) levels that do not increase by one day after ALT levels have peaked had a good negative predictive value, but low positive predictive value. Hence, serum AFP levels cannot be recommended as a critical prognostic factor at this time.
Liver TransplantationLiver transplantation is the only intervention with known survival benefit in patients with ALF. The outcome of liver transplantation is determined by the pretransplant condition of the patient and the quality of graft used. 5 year survival post transplant for ALF (70%) has been lower than transplantation for chronic liver failure (85%) due to the emergent nature and condition of the recipients. Comorbid cardiovascular, respiratory and systemic conditions have a negative affect on patient outcomes. Psychosocial and family support for compliance and substance abuse have important role in patient evaluation for transplant. The United Network for Organ Sharing (UNOS) has developed a system to rapidly distribute donor livers for life-saving transplantation by designating status 1, those patients at highest risk of short term death. Patients with onset of illness less than 8 weeks, Wilson’s disease and transplant recipients with primary graft nonfunction or early hepatic artery thrombosis are included in this status 1. Grafts are allocated to status 1 patients based on blood type, geography and waiting time.