Background: White phosphorus is chemical compound available in military ammunition as well as in explosive powder of recreational use. This latter form is commonly found in Latin America and Asia as a main ingredient of gunpowder used to make street firecrackers. Small firecrackers may be ingested accidentally or used as a toxic agent in suicidal attempts which may cause of acute liver failure and death; however the clinical features, incidence and outcome are poorly described in the literature.
Methods: We describe three cases of white phosphorus intoxication with acute liver failure secondary to the consumption of firecrackers. In two cases, ingestion occurred secondary to suicidal attempts and in one, ingestion occurred by accident. In one case, liver injury improved with supportive care, in the other, the patient required liver transplantation and the third case had a fatal outcome.
Conclusions: Clinicians providing care of patients with acute hepatitis of unclear etiology should be aware that the ingestion of firecrackers containing white phosphorus might cause acute liver failure that may require liver transplantation.
White phosphorus is an inorganic substance and smoke producing agent made from the chemical element phosphorus. This substance reacts rapidly with oxygen, easily catching fire at temperatures 10 to 15 degrees Celsius above room temperature. White phosphorus is used by the military in the production of ammunition and it is also used to produce phosphoric acid and other chemicals found in fertilizers, food additives, and cleaning compounds. In some countries, variable amounts of white phosphorus are used in the production of firecrackers and fireworks. In our country each firecracker contains between 4 mg to 9 mg of white phosphorus (Toxicology Laboratory of the University of Antioquia - Medellín, Colombia, unpublished data).
Intoxications and burns with white phosphorus are uncommon in the western world and they are originated mainly by labor exposure.1,2 In developing countries, intoxication can occur due to suicidal attempts or accidental consumption.3 Severe intoxications are characterized by multisystem organic failure4 with mortality rates ranging from 20 to 50%.5,6 The lethal dose after oral ingestion of white phosphorus is 1 mg/kg of body weight, although small amounts as little as 15 mg have resulted in death.7 Liver failure can occur as a consequence of white phosphorus intoxication,4,5,8 however there is scarce data of such cases. We describe three cases of white phosphorus intoxication with acute liver failure secondary to the consumption of firecrackers with a different spectrum of clinical manifestations.
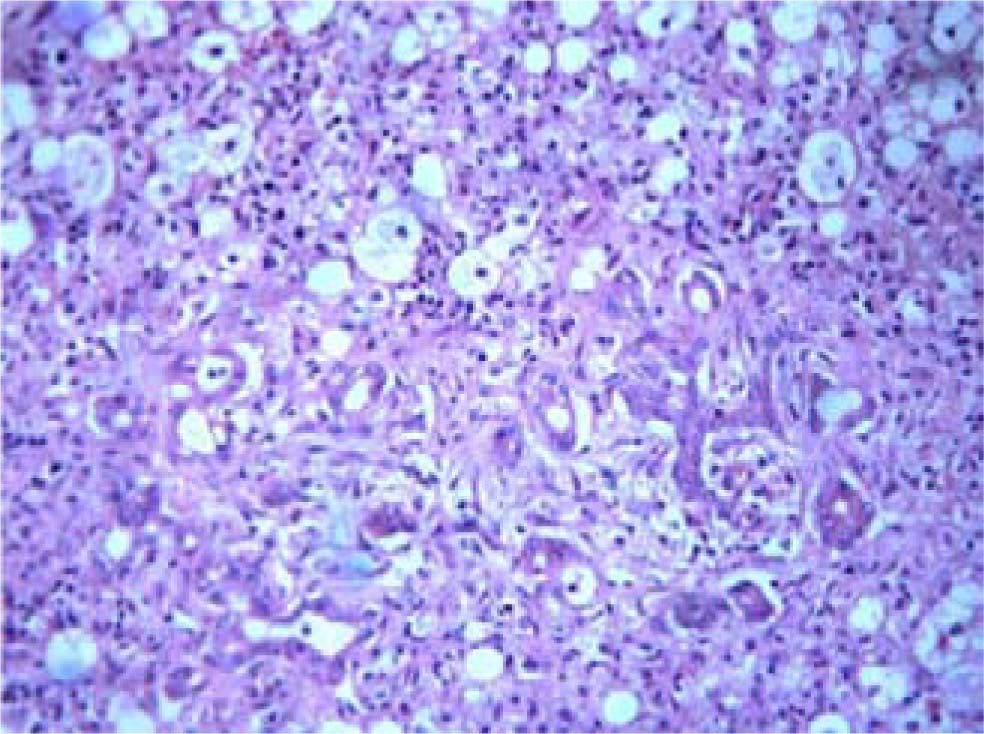
Case 1A 4 year old girl without significant medical history accidentally ingested 10 street firecrackers. She initially presented with mild abdominal pain, nausea and vomiting and was taken to the local emergency room where she was found to have a normal physical exam. She received intravenous fluids and had a gastric lavage performed with saline solution. Her laboratory tests showed a normal complete blood count and normal electrolytes and therefore was discharged. The patient continued to have symptoms of abdominal pain, nausea and vomiting. Two days after the ingestion, she developed jaundice, malaise and weakness and was hospitalized. Laboratory exams showed significant elevation of serum aminotransferases and coagulapathy (Table I). An abdominal ultrasound with Doppler was normal. She also became drowsy and confused and was therefore transferred to our hospital for evaluation of orthotopic liver transplantation (OLT). On admission she was comatose. Physical exam showed jaundice, ascites, hepatomegaly, hyperreflexia, and mydriatric pupils. Serum aminotransferases and bilirrubin levels were significantly elevated, and her prothrombin time (PT) was > 100 seconds (Table I). She was diagnosed with acute liver failure due to ingestion of white phosphorus. She was listed for emergency OLT and admitted in the Intensive Care Unit (ICU). Her mental status continued to worsen and she had a self limited episode of upper gastrointestinal hemorrhage thought to be related to her underlying coagulopathy. She underwent OLT three days later with a prolonged post-transplant period complicated by nosocomial pneumonia and acute cellular rejection (treated with tacrolimus IV). Histology of the explanted liver showed signs of toxic hepatitis with extensive hepatocyte necrosis and with balloon degeneration (Figure 1). She recovered successfully and was finally discharged 45 days after admission.
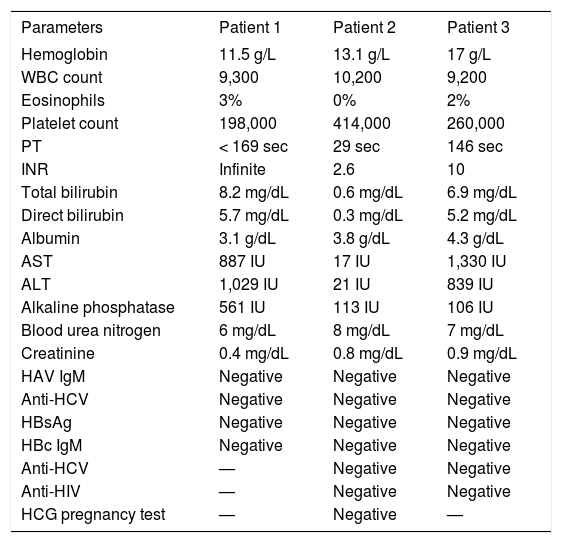
Laboratory exams on admission.
| Parameters | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Hemoglobin | 11.5 g/L | 13.1 g/L | 17 g/L |
| WBC count | 9,300 | 10,200 | 9,200 |
| Eosinophils | 3% | 0% | 2% |
| Platelet count | 198,000 | 414,000 | 260,000 |
| PT | < 169 sec | 29 sec | 146 sec |
| INR | Infinite | 2.6 | 10 |
| Total bilirubin | 8.2 mg/dL | 0.6 mg/dL | 6.9 mg/dL |
| Direct bilirubin | 5.7 mg/dL | 0.3 mg/dL | 5.2 mg/dL |
| Albumin | 3.1 g/dL | 3.8 g/dL | 4.3 g/dL |
| AST | 887 IU | 17 IU | 1,330 IU |
| ALT | 1,029 IU | 21 IU | 839 IU |
| Alkaline phosphatase | 561 IU | 113 IU | 106 IU |
| Blood urea nitrogen | 6 mg/dL | 8 mg/dL | 7 mg/dL |
| Creatinine | 0.4 mg/dL | 0.8 mg/dL | 0.9 mg/dL |
| HAV IgM | Negative | Negative | Negative |
| Anti-HCV | Negative | Negative | Negative |
| HBsAg | Negative | Negative | Negative |
| HBc IgM | Negative | Negative | Negative |
| Anti-HCV | — | Negative | Negative |
| Anti-HIV | — | Negative | Negative |
| HCG pregnancy test | — | Negative | — |
WBC: white blood cell, INR: International normalized ratio for prothrombin time (PT), ALT: alanine aminotransferase; AST: aspartate aminotransferase; HAV: hepatitis A virus, Anti-HCV: antibodies to hepatitis C; Anti-HIV: antibodies to human immunodeficiency virus, HBsAg: hepatitis b surface antigen, HBc: hepatitis B core antigen, HCG: human chorionic gonadotropin.
Fifteen year old female with a previous history of substance abuse and depression was seen in the outpatient clinic after she ingested 9 firecrackers in a suicidal attempt. One day after the ingestion she developed several episodes of nausea, vomiting and abdominal pain. On physical exam she was alert and well oriented with normal vital signs. There was no jaundice. Heart and lung examination were normal. Her abdomen was soft and nontender with no hepatomegaly or splenomegaly. Her neurologic examination revealed mild asterixis. Laboratory exams revealed a prolonged PT, with normal liver and renal tests (Table I). An abdominal ultrasound with Doppler flow showed no outflow obstruction or liver masses. A presumed acute liver failure secondary to white phosphorus was diagnosed. Therapy with IV fluids was begun and the patient was transferred to the ICU for monitoring. On day 3 the PT rose to 86 seconds, with a significant elevation of aminotransferases elevation and bilirrubin (Table II). Physical exam remained unchanged. She was listed for OLT after a thorough discussion with her psychiatrist who gave clearance for the procedure. However, on day 4 the PT remained at 90 seconds, and her clinical status unchanged without any evidence of hepatic encephalopathy. Her liver tests continued to improve slowly over the next 10 days. The patient was discharged after two weeks.
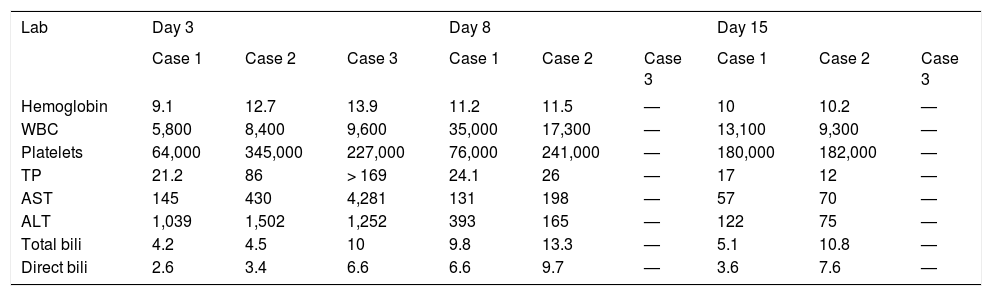
Laboratory exams during admission.
| Lab | Day 3 | Day 8 | Day 15 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 1 | Case 2 | Case 3 | Case 1 | Case 2 | Case 3 | |
| Hemoglobin | 9.1 | 12.7 | 13.9 | 11.2 | 11.5 | — | 10 | 10.2 | — |
| WBC | 5,800 | 8,400 | 9,600 | 35,000 | 17,300 | — | 13,100 | 9,300 | — |
| Platelets | 64,000 | 345,000 | 227,000 | 76,000 | 241,000 | — | 180,000 | 182,000 | — |
| TP | 21.2 | 86 | > 169 | 24.1 | 26 | — | 17 | 12 | — |
| AST | 145 | 430 | 4,281 | 131 | 198 | — | 57 | 70 | — |
| ALT | 1,039 | 1,502 | 1,252 | 393 | 165 | — | 122 | 75 | — |
| Total bili | 4.2 | 4.5 | 10 | 9.8 | 13.3 | — | 5.1 | 10.8 | — |
| Direct bili | 2.6 | 3.4 | 6.6 | 6.6 | 9.7 | — | 3.6 | 7.6 | — |
WBC: white blood cell count, PT: prothrombin time, AST, aspartate aminotransferase; ALT: alanine aminotransferase, bili: bilirubin.
A 32 year old male on a suicidal attempt ingested 12 firecrackers and 12 hours later developed abdominal pain, nausea and vomiting. Two days later he was seen at his local hospital with worsening abdominal pain and continuous vomiting and was therefore transferred to our hospital for further evaluation. On admission, he had jaundice, minor changes in mental status and asterixis. Heart and lung examination were normal. His abdomen was nontender without hepatomegaly or splenomegaly. Laboratory tests revealed direct hyperbilirubinemia (total bilirrubin 6.9 mg/dL), and increased AST and ALT > 20 times upper limit of normal, PT of 146 seconds (Table I). An abdominal ultrasound with Doppler showed no abnormalities. He was managed as acute liver failure secondary to white phosphorus. He was transferred to the ICU for monitoring and supportive treatment. The following day he had worsening of renal function, oliguria and severe metabolic acidosis. He was placed on veno-venous dialysis. His liver function continued to worsen and he developed grade II encephalopathy (West-Haven criteria). The patient’s clinical status remained unchanged and despite improvement of his acidosis, his renal and hepatic function worsened. He progressed to grade III encephalopathy, developed severe coagulopathy with upper gastrointestinal bleeding requiring mechanical ventilation and vasopressor therapy. Despite all these measures the patient died 3 days after admission.
DiscussionWhite phosphorus is a highly toxic element that can be absorbed by the gastrointestinal tract, the respiratory tract, the skin, and the mucous membranes. It is evenly distributed and incorporated in several tissues, particularly the liver.9,10 A dose of 15 mg can be highly toxic and if more than 50 mg are ingested it is fatal (1 mg / kg on the average).7 The toxicity of white phosphorus may occur due to alteration of the ribosomal function and the synthesis of proteins,13 loss of regulation of the blood glucose and the glycogen deposits14 and to the alteration of lipoprotein synthesis and secretion of triglycerides, leading to intracellular accumulation and fatty degeneration of multiple organs, especially the liver, the kidney, the heart and brain.7,11,12 White phosphorus intoxication produces multiple signs and symptoms which have been divided in stages.4 Stage I (General symptoms): Occurs during the first 24 hours after ingestion and is characterized by epigastric abdominal pain, profuse diarrhea, nausea, vomiting and in some cases fever. The breath, vomit and burps have garlicky scent but this not always this present. The laboratory tests in this stage are normal. Stage II (Asymptomatic): Occurs between 24 and 72 hours after ingestion. It is an asymptomatic period; however the histology of liver in this stage demonstrates early changes of toxic hepatitis and laboratory data shows mild elevation of aminotransferases and bilirrubin. Stage III (Advanced): After 72 hours until the resolution of the symptoms or death. This stage is characterized by multisystemic organic failure. There is acute hepatitis; liver histology shows steatohepatitis and necrosis.8 Patients may present with acute liver failure with encephalopathy, coagulopathy and abnormal liver tests.6-8,11 In some patients, depending on the ingested quantity of white phosphorus and for unknown reasons; the initial insult resolves spontaneously.13 In some cases renal failure ensues and patients develop with oliguria and acute tubular necrosis. The effects on the central nervous system are mainly the alteration of the mental status with irritability, confusion, psychosis, allucinations and coma. Patients may also develop hypotension, tachycardia, arrhythmias and cardiogenic shock.11,14
There is no specific diagnostic test and blood phosphorus levels are not useful.4 Thus diagnosis is one of exclusion after taking a detailed history and physical exam. In these three cases described above, viral, autoimmune, metabolic, and other hepatotoxic causes were excluded, and additionally abdominal ultrasonography with Doppler showed no liver masses, outflow obstruction, or biliary tract obstruction. We performed an extensive work-up to exclude other causes of acute severe hepatitis and only after all tests were negative we suspected white phosphorus to be the cause of hepatotoxicity. The temporal association between the ingestion of firecrackers, the development of symptoms, the elevation of liver enzymes and bilirubin (in case 1 and 3) as well as the exclusion of other causes suggested the possibility of an acute toxic-induced hepatitis.
Unfortunately there is no antidote or specific treatment for white phosphorus intoxication. Gastric lavage (with saline solution and potassium permanganate which can oxidize the phosphorus) should be performed in all cases if possible.4 Other substances for lavage such as solutions of copper sulfate and mineral oil, have been recommended but their clinical utility has not been well demonstrated.5,6 Since severe intoxications with white phosphorus can evolve quickly to an acute liver failure and multisystemic organic failure, it is recommended patients be admitted to the ICU with continuous monitoring and supportive measures. Liver transplantation should be performed in suitable candidates according to previous defined criteria (i.e. King’s College) for acute liver failure.15 Intravenous steroids and exchange transfusion were previously used in 49 patients with an acute intoxication due to white phosphorus; however this treatment strategy did not appear to prevent the onset of coma in this type of liver injury and did not increase survival after development of coma.16
In conclusion, ingestion of firecrackers containing white phosphorus may cause non-specific gastrointestinal symptoms and acute hepatitis with severe prolongation of the prothrombin time that may resolve spontaneously, require liver transplantation or result in death. Physicians caring for patients with acute hepatitis of unclear etiology should be aware that the ingestion of firecrackers containing white phosphorus might cause liver failure that may require liver transplantation.