Standard treatment of autoimmune hepatitis (AIH) includes steroids such as predniso(lo)ne based upon study data established decades ago.1,2 Pilot studies indicate that budesonide may represent an alternative treatment option.3 Recently, this was confirmed in non-cirrhotic AIH patients showing that budesonide is capable of efficiently inducing remission in comparison to prednisone (both in combination with azathioprine) with the advantage of reduced steroid specific side effects.4 This is likely to increase the awareness of budesonide in hepatology and its administration in AIH patients.
We report a 40-year old female Turkish patient, who underwent orthotopic liver transplantation (OLT) in June 2010 with decompensated liver cirrhosis because of AIH, and hepatocellular carcinoma (HCC).In 2002, a first episode of hepatic decompensation occurred and she was seen in a referring hospital. Following the exclusion of viral or metabolic causes of liver disease, and in view of detectable smooth muscle (SMA) antibodies (titer: 1:320) as well as elevated immunoglobulin G levels (18.6 g/L) a diagnosis of AIH was established. Later, anti-nuclear antibodies (ANA) (titer: 1:320) were also detected. Autoantibodies were subsequently undetectable once prednisolone treatment (5 to 20 mg per day) had begun. In April 2009, a second decompensation episode occurred. Immunosuppression was increased to 70 mg prednisolone per day in order to induce remission. With the intention to prevent steroid specific side effects this was switched to budesonide (3mg t.i.d.). One month later she was urgently referred to our center, again with hepatic decompensation. Diagnostic work-up revealed Budd-Chiari syndrome, which had not been previously observed on CT or MRI scans performed one month prior to admission (Figures 1A, 1B). Histology confirmed cirrhosis and evidence of centrilobular sinusoidal congestion (Figures 1D, 1E). Budesonide was discontinued and prednisone therapy resumed, in addition to anticoagulant treatment with low molecular weight heparin. The patient was successfully stabilized. However, 2 months following this episode hepatocellular carcinoma was diagnosed, she was listed for OLT, which was successfully performed one year later (Figures 1C-1G).
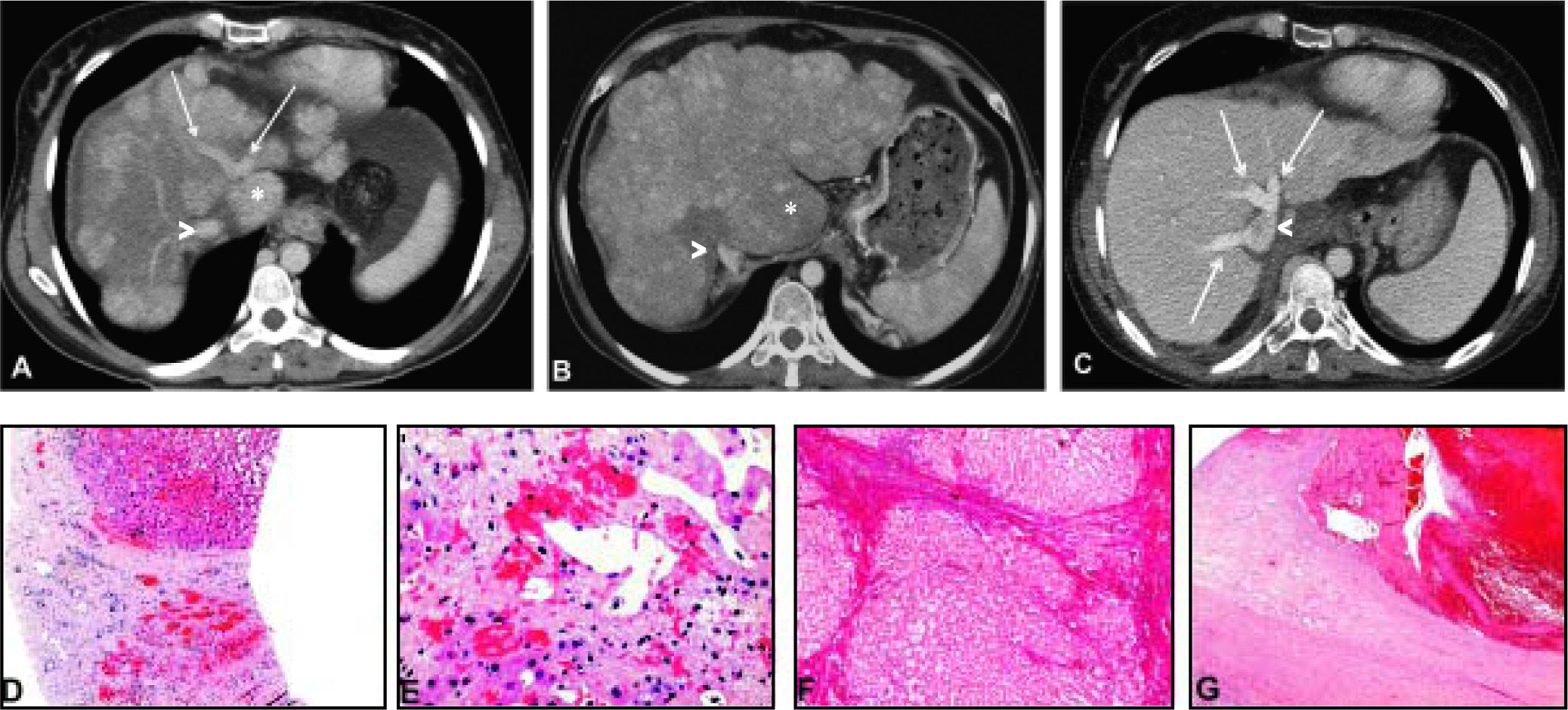
Axial contrast-enhanced CT images at the level of the confluence of the hepatic veins into the hepatic vena cava (>) and liver biopsy at the time of referral when Budd-Chiari syndrome was diagnosed. A. Demonstrates patent hepatic middle and left hepatic veins (arrows), and cirrhotic changes with regenerative nodules can be appreciated.
B. A CT study three months after (A) shows complete obliteration of the hepatic veins with the absence of contrast enhancement. The liver is diffusely hypodense and hypertrophy of the caudate lobe (*) is present as a consequence of Budd-Chiari syndrome.
C.A CT study 3 weeks following OLT shows regular parenchymal liver enhancement with patent hepatic veins. There is established cirrhosis [D, hematoxylin eosin (HE), ×100] as well as centrilobular congestion with sinusoidal dilatation, hemorrhage into the space of Dissé and centrolobular necrosis (E, HE, × 400). Examination of the explanted liver confirmed cirrhosis (F, elastin van Gieson, × 100) as well as organising thrombi in large hepatic veins: Budd-Chiari syndrome (G, HE, × 100).
Budesonide is a synthetic steroid with a low rate of systemic side effects because of considerable (90%) hepatic first-pass metabolism. Compared to prednisolone, it exhibits greater than 15-fold higher glucocorticoid receptor5 binding. This feature and reported budesonide studies have attracted the attention of physicians treating patients with AIH. However, although a recent randomized controlled trial has demonstrated the efficacy of this drug in non-cirrhotic AIH patients,4 the present case illustrates that cirrhosis and portal hypertension may pose considerable risks for this treatment option. Budesonide has been reported as a treatment option in primary biliary cirrhosis (PBC), however plasma concentrations were observed to be increased in PBC stage IV when compared to stages I/II.6 Importantly, in that study 2 out of 7 patients with PBC stage IV developed portal venous thrombosis as a serious complication.6 In our patient, Budd-Chiari syndrome was diagnosed only a few weeks after budesonide (3 mg t.i.d.) was administered (Figures 1B, 1E). Other potential causes of thrombophilia including haematological disorders (JAK2 mutation, activated protein C resistance, factor V mutation) were excluded.7 In addition, HCC (1.5 cm nodule, pT1pN0G2) did not reveal signs of vascular invasion upon post-OLT histology (not shown).
To our knowledge Budd-Chiari syndrome following the initiation of budesonide therapy has not previously been reported. Although this case does not provide an absolute causal link of budesonide and Budd-Chiari syndrome in patients with portal hypertension it expands on the observation of portal venous thrombosis in advanced stages of PBC treated with budesonide. This indicates that the administration of budesonide in patients with established cirrhosis may increase the risk of serious complications.
Financial DisclosureMM and CPS have received speaker honoraria from Dr. Falk Pharma, Freiburg, Germany. The remaining authors have nothing to disclose.





![Axial contrast-enhanced CT images at the level of the confluence of the hepatic veins into the hepatic vena cava (>) and liver biopsy at the time of referral when Budd-Chiari syndrome was diagnosed. A. Demonstrates patent hepatic middle and left hepatic veins (arrows), and cirrhotic changes with regenerative nodules can be appreciated. B. A CT study three months after (A) shows complete obliteration of the hepatic veins with the absence of contrast enhancement. The liver is diffusely hypodense and hypertrophy of the caudate lobe (*) is present as a consequence of Budd-Chiari syndrome. C.A CT study 3 weeks following OLT shows regular parenchymal liver enhancement with patent hepatic veins. There is established cirrhosis [D, hematoxylin eosin (HE), ×100] as well as centrilobular congestion with sinusoidal dilatation, hemorrhage into the space of Dissé and centrolobular necrosis (E, HE, × 400). Examination of the explanted liver confirmed cirrhosis (F, elastin van Gieson, × 100) as well as organising thrombi in large hepatic veins: Budd-Chiari syndrome (G, HE, × 100). Axial contrast-enhanced CT images at the level of the confluence of the hepatic veins into the hepatic vena cava (>) and liver biopsy at the time of referral when Budd-Chiari syndrome was diagnosed. A. Demonstrates patent hepatic middle and left hepatic veins (arrows), and cirrhotic changes with regenerative nodules can be appreciated. B. A CT study three months after (A) shows complete obliteration of the hepatic veins with the absence of contrast enhancement. The liver is diffusely hypodense and hypertrophy of the caudate lobe (*) is present as a consequence of Budd-Chiari syndrome. C.A CT study 3 weeks following OLT shows regular parenchymal liver enhancement with patent hepatic veins. There is established cirrhosis [D, hematoxylin eosin (HE), ×100] as well as centrilobular congestion with sinusoidal dilatation, hemorrhage into the space of Dissé and centrolobular necrosis (E, HE, × 400). Examination of the explanted liver confirmed cirrhosis (F, elastin van Gieson, × 100) as well as organising thrombi in large hepatic veins: Budd-Chiari syndrome (G, HE, × 100).](https://static.elsevier.es/multimedia/16652681/0000001100000001/v1_201906201317/S1665268119315005/v1_201906201317/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)




