Dear Editor:
Primary sclerosing cholangitis (PSC) is a chronic, cholestatic liver disease which leads to end-stage cirrhosis, is a recognized risk factor for hepatobiliary and colonic carcinogenesis, and carries a median liver transplant (LT) free survival time of approximately 15 years.1–4 Due to its progressive and idiopathic nature, lack of effective pharmacotherapy, and paucity of predictors of adverse outcomes,5 PSC is the 5th most common indication for LT in the United States6 and a leading indication in several other countries worldwide.3,7
One of the feared and costly complications of PSC is development of colorectal cancer (CRC). CRC is the third most commonly diagnosed cancer and third leading cause of cancer-related death in men and women, and on a global scale, there are an estimated 1,200,000 million new diagnoses of CRC and over 600,000 CRC-related deaths annually, many of which could be prevented by increasing the use of established screening and surveillance tests.8,9 At particular risk of CRC are the 70% of PSC patients who also have inflammatory bowel disease (IBD),10–15 a chronic disorder of the alimentary tract which, in the United States alone, has a prevalence of approximately 1,000,000 persons and direct and indirect costs exceeding 11,000,000,000 dollars.9,16,17 IBD is associated with a 6-fold increased risk of CRC compared to the general population (with the exact risk depending on the duration and extent of IBD as well as other less understood factors),16,18 but when there is co-existing PSC, this risk rises to nearly 30-fold.10,11,14 Therefore, it is no overstatement that management of PSC-IBD and its complications, not the least of which is CRC, engenders substantial patient-level and public health burden.9,19,20
Many hepatologists will have, as part of their practice, patients with PSC-IBD. Very frequently, the consulting hepatologist oversees the management of these patients, including but not limited to laboratory monitoring, bone densitometry, and hepatobiliary and CRC surveillance; as a result, the overall health of these patients relies considerably on the hepatologist and having an informed, integrated care team.17 CRC surveillance is particularly critical in these patients given the aforementioned statistics as well as the fact that:16
- •
Mortality of IBD-associated CRC is considerably higher than that of sporadic CRC and that
- •
Age at presentation tends to be considerably younger among the former.
With these considerations in mind, members of an international multidisciplinary group recently published recommendations to encourage uniform, evidence-based practice for surveillance and management of colorectal dysplasia in IBD.21,22 Perhaps the foremost message with respect to surveillance of colorectal dysplasia in this work, known as the SCENIC consensus statement, is that standarddefinition colonoscopy, even with 32 random colonic biopsies (the recommendation up until now), is in fact sub-standard. Therefore, colorectal dysplasia surveillance should instead be performed via highdefinition colonoscopy with chromoendoscopy, which utilizes methylene blue or indigo carmine (sprayed through the colonoscope) to enhance mucosal topography and irregularity detection. This recommendation is based on the observation that, with advancements in technology, most colonic dysplasia in IBD is now endoscopically visible, thus highlighting the importance of (chromoendoscopyassisted) targeted biopsies rather than random sampling. Overall, we believe that the SCENIC consensus statement contains important information for hepatologists as well as their patients at high-risk for CRC, e.g. those with PSC complicating IBD (or other predictors of CTC, e.g. family history).
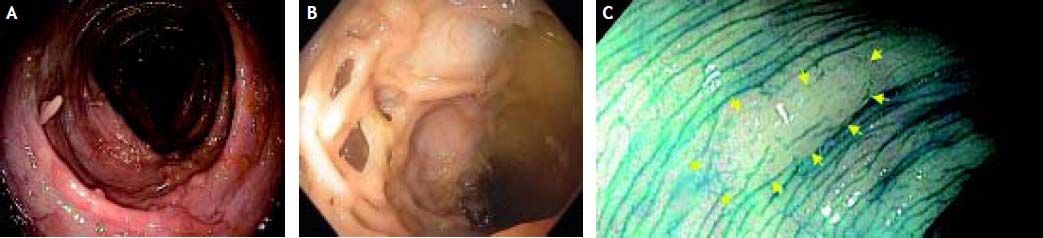
The value of the SCENIC consensus statement is illustrated, for example, in a case we recently encountered of a 48 year-old man with a 30-year history of IBD and PSC who presented for routine follow-up. He was asymptomatic and on a stable dose of mesalamine 2.4 g/day. Physical examination, serologies, and abdominal computed tomography were unremarkable. At colonoscopy, there were innumerable lesions-some demonstrating a vermiform appearance (Figure 1A), others bridging the colonic lumen with a lattice-like configuration (Figure 1B), and yet others with more typical pedunculated polyp morphology. To the inexperienced eye, these may have appeared concerning for dysplasia or even a polyposis syndrome, but in actuality they were consistent with post-inflammatory hypertrophic polyps, i.e. benign sequelae of exaggerated mucosal repair and regeneration. While benign, these hypertrophic polyps can obscure detection of dysplastic polyps, even for experienced endoscopists. Such was the case with our patient; a 1 cm flat lesion (Figure 1C) missed on standard colonoscopy just moments prior was detected with chromoendoscopy, resected, and found to harbor dysplasia.
Colonoscopic images in a patient with primary sclerosing cholangitis and quiescent ulcerative colitis. A. Vermiformappearing, post-inflammatory hypertrophic polyp. B. Post-inflammatory hypertrophic polyp with lattice-like configuration. C. Colonoscopy with methylene blue chromoendoscopy revealing a 1 cm flat lesion which was resected and found to harbor dysplasia.
Looking ahead, recommending evidence-based surveillance programs to help preserve the health of patients with PSC-IBD will likely remain a collective duty of hepatologists, gastroenterologists, and primary care providers. The SCENIC guidelines provide useful direction in this regard, and it is vitally important that PSC patients, particularly those with IBD, be referred to centers with expertise in high-resolution chromoendoscopy for CRC surveillance. These referrals should be made at the intervals established by societal guidelines and with careful risk stratification based on patient as well as family history.16,23,24 In turn, CRC surveillance should also inform hepatobiliary carcinoma surveillance, e.g. ensuring annual cholangiocarcinoma surveillance in patients with PSC, particularly those with prior colectomy for IBD-associated colorectal dysplasia.1,11,25
Until more data are generated to better guide CRC surveillance in PSC, emphasis on these recommendations by hepatologists, gastroenterologists, and primary care providers will be essential for improving patient adherence and clinical outcomes.
Abbreviations- •
CRC: colorectal cancer.
- •
IBD: inflammatory bowel disease.
- •
PSC: primary sclerosing cholangitis.
None.