In 1723 Vater and Ezler carried out the first anatomic description of a bile duct cyst. In 1852 Douglas performed the first clinical description, in which he hypothesized than biliary duct cysts were due to a congenital weakness of the common hepatic duct’s walls. In 1924 McWhorter performed the first resection of a common hepatic duct cyst. Alonso-Lej et al classified this pathology for the first time in 1959. This classification was broadened by Todani et al. in 1977 to include intra-and extra-hepatic cysts.1
Incidence is approximately 1:100,000 to 1:150,000 in the West. However, incidence is significantly higher in Eastern countries such as Japan and China, where it reaches approximately 1: 1,000. This disease is four times more common in women than in men, and represents 1% of all benign biliary tract lesions. 20% of cases arise in adults.2
The aim of this case report is to describe this variant of biliary duct cystic dilatations and their surgical treatment, as well as to propose its introduction as subtype Id into Todani’s Modified Classification, so as to include all possible variations of biliary duct cystic dilatations.
The present case is a fifty year old female patient was studied after presenting a single previous episode of jaundice, without pain or signs of cholangitis. The physical exam and the liver functions tests were normal.
Ultrasonographic examination revealed a bile duct cystic stricture. An extra hepatic dilatation without anomalous pancreatobiliary junction was observed in the CT scan. The cyst was above the junction of the common hepatic and cystic ducts. MRI showed a biliary cyst, most likely a Todani type Ib (Figure 1). A normal pancreatic duct was found during endoscopic retrograde cholangiopancreatography (ERCP), but complete evaluation of the biliary tree could not be performed.
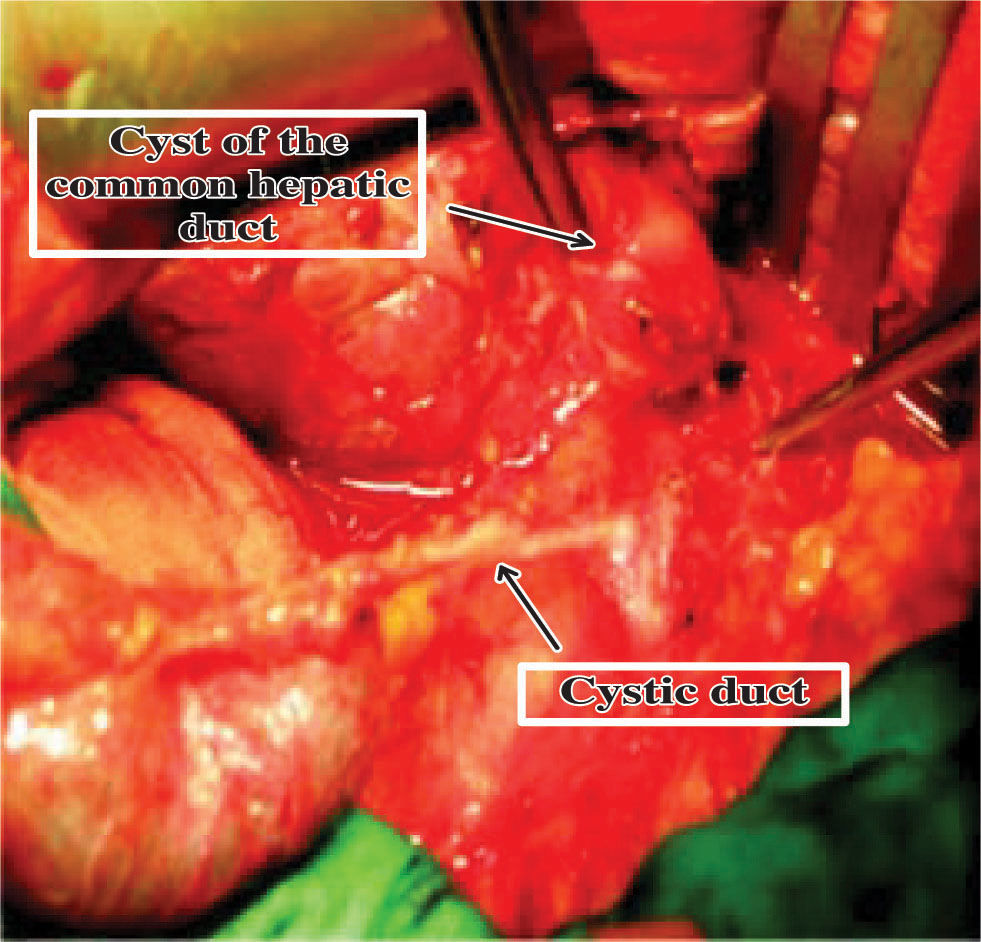
During surgical exploration a cystic dilation of the biliary tree limited only to the common hepatic segment was found (Figures 2and3). This finding was confirmed by cholangiography.
Cholecystectomy and complete resection of the cyst was performed, and reconstruction was carried out with a Roux in Y hepatoyeyunostomy. The patient’s postoperative course was uneventful.
Although the precise etiology of biliary tract cysts is unknown, the most embraced theory attributes these pathologic variants to anomalous unions of the pancreatic duct and the biliary tract. These variants can be found in 21 to 90% of cases and can condition a reflux of pancreatic enzymes to the biliary tree, as well as inflammation, ectasis and elevated pressure, which may result in cyst formation.3
Patients usually present jaundice, nausea, and vomiting. A palpable abdominal mass is usually found in children, whereas adults tend to present epigastric or right upper quadrant pain.5
Several imaging techniques can help in the diagnosis of this pathology, including ultrasonography,4 CT,6 ERCP,7 and Magnetic Resonance.8
The most commonly found hepatobiliary pathology associated to biliary tract cysts is cystolithiasis, although cholangitis, pancreatitis, cholescystitis, hepatic cirrhosis, portal hypertension, and portal vein thrombosis may also be found in association to this disease. Carcinoma of the hepatic duct can be found in up to 28 to 30% of adult patients, with cholangiocarcinoma being the most common variant.9
Treatment is surgical in all cases. The cystic lesion must be completely removed and biliodigestive reconstruction is performed according to the type of lesion found. For type I cysts either: hepatoyeyunal or hepatoduodenal reconstruction may be performed, by laparoscopy or open surgery. Type II cysts, also known as supraduodenal diverticulum, are treated with either open or laparoscopic excision of the cyst.10 Type III cysts, or choledococele, are treated by endoscopic sphinterotomy.11,12 For type IV or V cysts surgical treatment depends on the degree of damage to the intra or extrahepatic biliary tract, and it can go from localized hepatic resection and excision to liver transplant.13
Cystic dilatation of the biliary tract, be it intra or extrahepatic, combined or segmentary, is an unfrequent disease that generally manifests in an early age with episodes of jaundice and cholangitis, and whose diagnosis is usually performed with diverse imaging techniques. Medical literature tends to refer to this entity as «Cysts of the Common Hepatic Duct», possibly due to the fact that the original classification only considered cysts found in the extrahepatic biliary tract.
In the currently used modified classification made by Todani, 5 variations of biliary tract cysts are described, and they include both the intra and extrahepatic biliary ducts. Type I includes three subtypes.
We propose introducing this variant as type Id in Todani’s Modified Classification of biliary duct cysts so it includes every type of cystic dilatation described as well as their surgical treatment (Figure 4).