Abstracts Asociación Mexicana del Hígado (AMH) 2023
Más datosIt has been reported that up to 39.7% of liver transplant recipients develop hepatic steatosis at some point during follow-up, with recurrence being more likely than de novo appearance. Specifically in patients previously known to have MAFLD, this condition is favored by the components of the metabolic syndrome (particularly being overweight), to which is added the use of immunosuppressive drugs. The objective is to determine the prevalence of hepatic steatosis by ultrasound in patients receiving liver transplants at the Hospital de Especialidades del Centro Médico Nacional La Raza.
Materials and PatientsIn this study were included liver transplant recipients treated in the period from 2017 to 2023 who had a liver ultrasound at least six months after transplantation. The diagnosis of hepatic steatosis was established by an increase in the echogenicity of the liver parenchyma, which is equal to or exceeds the echogenicity of the pancreas.
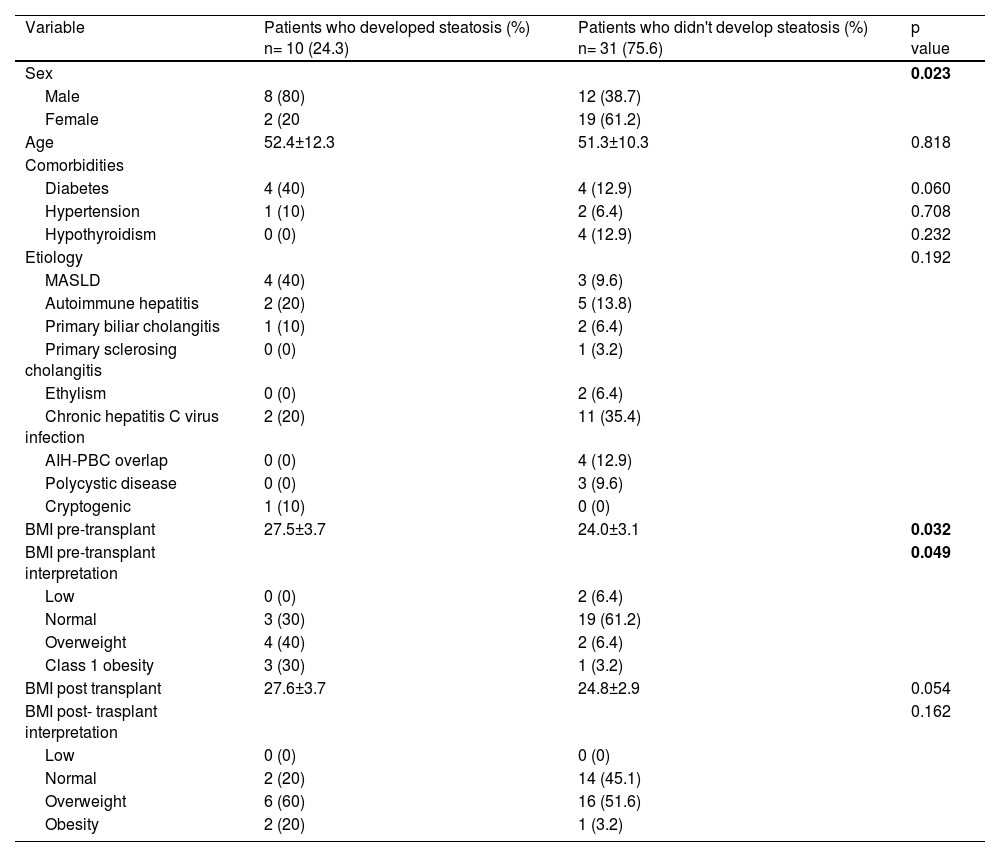
ResultsA sample of 40 patients was analyzed, 19 men (47.5%) and 21 women (52.5%), with age of 52.05 ±10.49 years. The most common causes of liver disease were hepatitis C virus infection (32.5%), MAFLD (17.5%), and autoimmune hepatitis (15%). The most frequent comorbidity was diabetes (20%)(Chart 1). Hepatic steatosis was found in 25% of cases (50% men and 50% women) (Graph 1). The most frequent etiology of liver disease in patients who developed steatosis was MAFLD (20%), while in those who did not develop steatosis it was HCV infection (40%), without statistical significance. When compared with patients without steatosis, there were no statistically significant differences in post-transplant weight and BMI (69.2 vs. 67.0 kg, p= 0.601; BMI 26.0 vs. 25.0, p=0.529) or pre-transplant MELD (14.3 vs. 16.4, p= 0.251)
ConclusionsIn our study, the prevalence of steatosis found was similar to that reported by other authors. They have not evidenced statistically significant differences in age, gender, comorbidities, anthropometry, or etiology of cirrhosis. Patients need close monitoring to identify the development of this complication in a timely manner.
Ethical statement
The protocol was registered and approved by the Ethics Committee. The identity of the patients is protected. Consentment was obtained.
Declaration of interests
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Characteristics of people who developed hepatic steatosis.
MASLD, metabolic dysfunction-associated steatotic liver disease; AIH, autoimmune hepatitis; PBC, primary biliary colangitis; BMI, body mass index.
Figure 1. Prevalence of steatosis in patients receiving liver transplantation.