The pregnant woman experiences physiological changes to support fetal growth and development. Particularly the physiological changes of the liver are the results of the increment of estrogens and progesterone during the pregnancy, and also the hemodynamics changes. (hemodilution). Telangiectasia may appear in up to 60% of normal pregnancies. Liver function test (LFT) abnormalities occurs in 3% of the pregnancies, and the Preeclampsia is the most frequent cause. Most of the articles agree that in normal pregnancy the LFT are either normal or slightly increase o decrease but within normal range. Thus, an increase in serum ALT, AST and GGT activities and serum bilirubin and total bile acid concentration during pregnancy may be pathologic and should prompt further evaluation. In the same way the serum albumin levels is significantly low and the serum alkaline phosphatase concentrations are considerably higher and are a normal component of the pregnancy, and if they are within normal range, do not usually indicate the presence of liver disease. The prothrombine time and the partial prothrombine time remain unchanged during pregnancy and serum fibrinogen increase in late pregnancy. Most of the articles related to plasma lipids in pregnancy agree that cholesterol. Triglyceride and lipoprotein increase during pregnancy. Use of gestational age of the pregnancy are the best guide to the differential diagnosis of liver disease in the pregnancy.
The pregnant woman experiences physiological changes to support fetal growth and development. During the pregnancy serum estrogens and progesterone levels increase progressively and reach a maximum during the third trimester. These sex steroids have effects on metabolic, synthetic and excretory hepatic function.1
Pregnancy is associated with significant change in the functions of normal liver. Although the precise mechanisms underlying these various alterations are not clear in every case, their recognition is essential to a proper clinical evaluation of liver abnormalities during pregnancy.
Physical examinationThe liver which is normally palpated 2 cm inferior to the right costal margin, may become more difficult to appreciate because of the expanding uterus within the abdominal cavity. A palpable liver is an abnormal finding.
Telangiectasia and palmar erythema, which are classically associated with chronic liver disease, may appear in up to 60% of normal pregnancies and usually disappear after delivery, as the liver cannot metabolize quickly the large quantity of estrogen and progesterone produce during pregnancy.2
Liver Function Test (LFT)Are a panel of laboratory test that profile discrete aspect of liver function.
Liver function test (LFT) abnormalities were investigated in 4,377 deliveries during the 15 months study period. A total de 142 patients were found to have abnormal LFT (3%) of all the pregnancies.7 The most common abnormalities were:3
- •
AST elevated in 119 of 142 (84%) (median 70 U/L).
- •
GGT elevated in 56 of 142 (39%) (median 51 U/L).
- •
Bilirrubin elevated in 24 of 142 (17%) (median 17% mcmol/L).
- •
Bile acids elevated in 20 of 142 (16%) (median 50 mcmol/L.
Preeclampsia and HELLP syndrome were the most common underlying abnormalities (48% and 22% respectively).
Liver cell injury or necrosis is measured by determining the activity of alanine amino transferase. (ALT) and aspartate amino trasferase (AST). In most publish studies, ALT and AST serum activity were found to be within normal limits during pregnancy. In a recent paper of Dr. Bacq,4 Serum alanine amino transferase was slightly but significantly higher during the second trimester, but was no different during the third trimester. Values were within normal ranges. The serum AST activity was during all three trimester not significantly higher than in the control group.
An increase in AST and ALT levels was found during labor, which might be caused by contractions of uterine muscle.1,2
In general practice, it is consider than serum AST and ALT activities remain normal during pregnancy before labor, and any increase in its activities should lead to further investigations.1
Liver synthetic function is quantified by albumin levels and prothrombin time.2 Plasma volume increases by approximately 50% from the 6th to the 36th week of gestation. Red cell volume also increases, but to a lesser extent and more gradually than plasma volume. The degree of hemodilution is approximated by the decrease of hematocrit. Plasma and red cell volume decrease back to the normal range after delivery, aided by the blood loss at delivery.1,4
The blood flow in the liver itself remain the same or in some studies decreases (35% of the cardiac output in non-pregnant females and 28% of cardiac output in pregnant females).4
Because hemodilution, serum albumin levels decrease during all thee trimesters. (The decrement becomes more accentuated as the pregnancy advances.) It is necessary to bear in mind this phenomenon in the interpretation of all serum concentration values during pregnancy.
Serum alkaline phosphatase concentrations are significantly higher (up to two to four times normal) in the third trimester. During the second trimester, AP activity was significantly higher than in the first trimester. This is primarily due to placental isoenzyme production, and an increase in the bone isoenzyme rendering it a poor means of diagnosis cholestasis during the third trimester of pregnancy.1,2
Serum gammaglutamyl transpeptidase activity (GGT) is significantly lower during the second and third trimester. Hepatic synthesis of GGT could be inhibited by hormone secretion during pregnancy.1
Serum 5’ nucleotidase activity is slightly but significantly higher en the second and the third trimester than in the first trimester. The placenta contains PA and 5’ nucleotidase but the diffusion out of the placenta into the maternal circulation may be restricted because of greater molecular weight of 5’ nucleotidase.
Total and free bilirrubin concentration are significantly lower than controls during all three trimesters, as were concentrations of conjugate bilirrubin during the second and third trimester. Hemodilution could at least partly responsible for the decrease of bilirrubin concentration because albumin is the protein transport bilirrubin.1
Total Bile Acid. (TBA). Previous investigations observed a significant increase from the first to the third trimester. In the study of Dr. Bacq,1 the concentrations did not differ from the control group.
These findings suggest than in normal pregnancy most liver biochemical test are either normal or slightly increased or decreased but within normal range. Thus, an increased in serum ALT, AST and GGT activities and serum bilirrubin and total bile acid concentration during pregnancy may be pathologic and should prompt further evaluation.2
On the other hand, hypoalbuminemia and an elevation in serum alkaline phosphatase may be a normal component of pregnancy and, if within the normal ranges, do not usually indicate the presence of liver disease.1
The prothrombin time and partial thromboplastin time remain unchanged during pregnancy and serum fibrinogen increases in late pregnancy.4
Plasma lipids. Cholesterol and triglycerideMost of the articles related to plasma lipids in pregnancy agree that both increase during pregnancy, as well as lipoprotein (Table I).
Plasma cholesterol and triglyceride changes during pregnancy and in the puerperium.
| N | Cholesterol* | Triglyceride | |
|---|---|---|---|
| Nonpregnant | |||
| Women | 15 | 202 | 95 |
| First trimester | 11 | 200 | 100 |
| Second trimester | 32 | 274 | 168 |
| Third trimester | 48 | 310 | 300 |
| Delivery | 35 | 312 | 296 |
| Dat 5 postpartum | 43 | 283 | 174 |
Potter J. and Nestel J.P. (5).
The cholesterol levels show an overall 53% increase during pregnancy, two thirds of which occurred within the second trimester.
The plasma triglyceride concentration increased threefold during the pregnancy. Most of this increase took place in the last trimester of the pregnancy.
The cholesterol decrease 15% within 12 to 24 hours of delivery, but at day 5 of postpartum some rebound occurs and al 6 to 7 week of postpartum the women had still a significant raised cholesterol levels.5
Many diseases can occur during pregnancy and require diagnosis in the context of expected physiological changes.
Two recommendations are critical for the diagnosis of liver diseases during pregnancy.1
A. An understanding of the physiological and biochemical changes that occur during normal pregnancy that may have bearing on the pathogenesis and diagnosis of hepatobiliary disease.
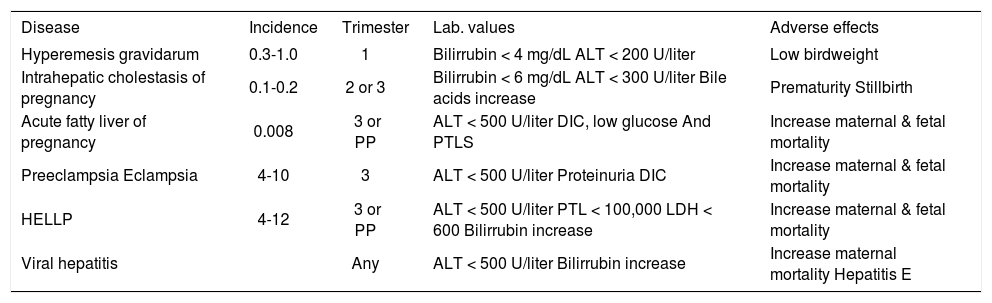
B. An understanding that specific diseases are far more likely in certain trimesters, although there may by exceptions and overlap. Use of gestational age of the pregnancy are the best guide to the differential diagnosis of liver disease in the pregnant woman6(Table II).
Characteristics of liver disease in pregnancy.
| Disease | Incidence | Trimester | Lab. values | Adverse effects |
|---|---|---|---|---|
| Hyperemesis gravidarum | 0.3-1.0 | 1 | Bilirrubin < 4 mg/dL ALT < 200 U/liter | Low birdweight |
| Intrahepatic cholestasis of pregnancy | 0.1-0.2 | 2 or 3 | Bilirrubin < 6 mg/dL ALT < 300 U/liter Bile acids increase | Prematurity Stillbirth |
| Acute fatty liver of pregnancy | 0.008 | 3 or PP | ALT < 500 U/liter DIC, low glucose And PTLS | Increase maternal & fetal mortality |
| Preeclampsia Eclampsia | 4-10 | 3 | ALT < 500 U/liter Proteinuria DIC | Increase maternal & fetal mortality |
| HELLP | 4-12 | 3 or PP | ALT < 500 U/liter PTL < 100,000 LDH < 600 Bilirrubin increase | Increase maternal & fetal mortality |
| Viral hepatitis | Any | ALT < 500 U/liter Bilirrubin increase | Increase maternal mortality Hepatitis E |
Knox, A. Tamsin.6