We describe the case of a 73-year-old woman was admitted to our hospital because of constant abdominal pain in her right upper quadrant and postprandial bloating and fullness for several months. On abdominal x-ray the extrahepatic bile ducts were positive for gas and on ultrasound a gallstone in the duodenum was suspected whereas the gallbladder was not detectable. An upper gastrointestinal endoscopy confirmed a large gallstone that was impacted in the duodenal bulb (“Bouveret’s syndrome”). The gallstone was fragmented employing mechanical lithotripsy and removed. Duodenoscopy revealed a cholecystoduodenal fistula and a second gallstone in the gallbladder. The patient underwent open cholecystectomy with closure of the cholecystoduodenal fistula and made a full recovery. We conclude that in patients with upper abdominal pain and pneumobilia on x-ray the unusual complication of cholelithiasis with an impacted gallstone in the duodenal bulb should be suspected. In those rare cases of Bouveret’s syndrome endoscopic removal of the gallstone should be attempted to minimize the necessary surgical procedure whenever possible.
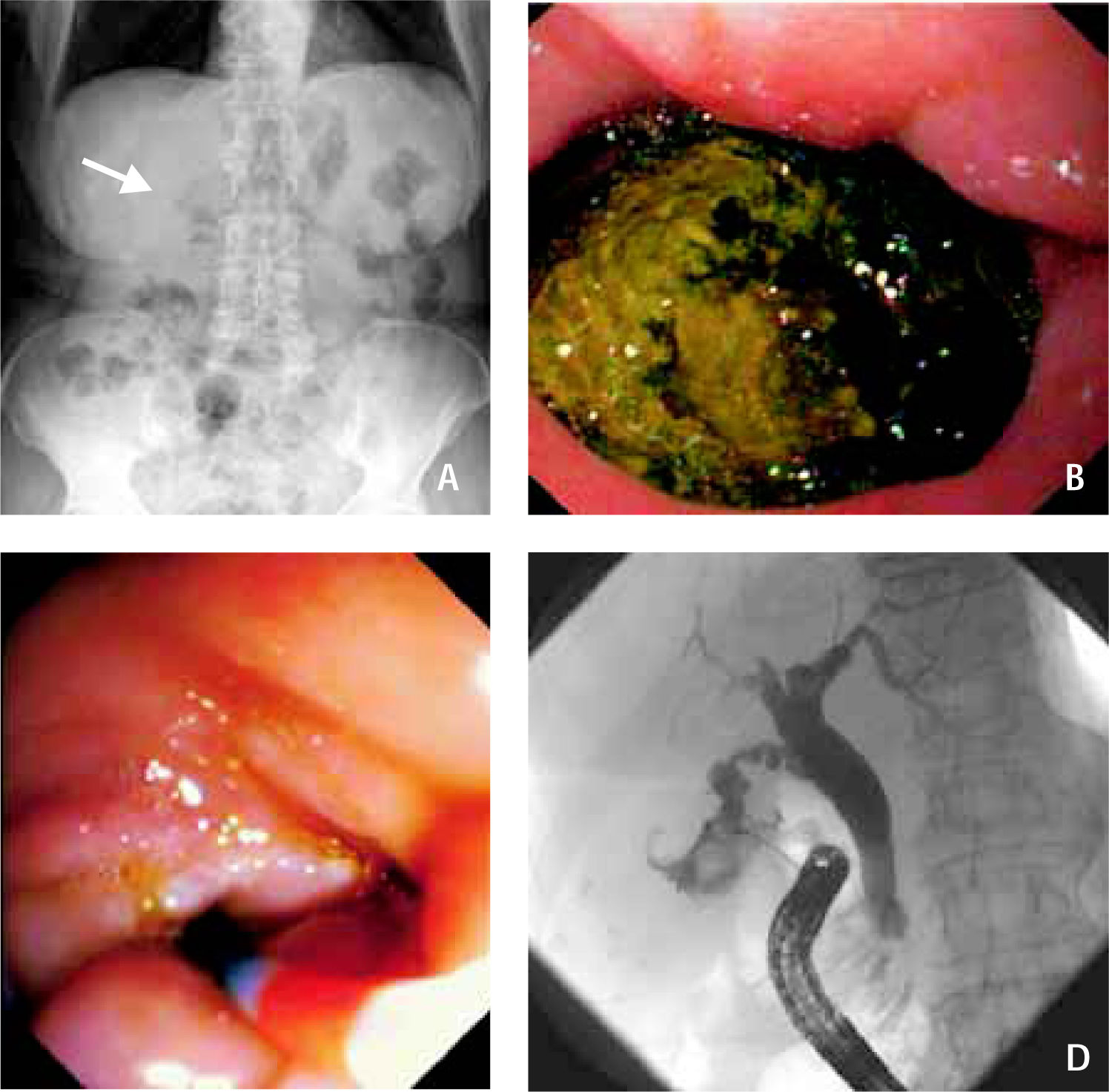
A 73-year-old woman was admitted to our hospital because of constant abdominal pain in her right upper quadrant and postprandial bloating and fullness for several months. No prior abdominal surgery was performed. The patient denied any vomiting and did not recall any episodes of fever. Her past medical history was remarkable for diabetes mellitus type II that was treated with insulin for several years and schizophrenia that was controlled with monthly i.m. injections of fluphenazin decanoate. On physical examination, the patient was overweight (BMI 28.6) and afebrile (37.0 °C). Blood pressure was 130/80 mmHg, pulse rate 84 bpm and regular. Examination of the abdomen showed tenderness of the right upper quadrant without guarding. The bowel sounds were unremarkable and there were no organomegalies. A complete blood cell count, CRP levels, liver function tests and cholestasis parameters were all normal. An ultrasound examination of the abdomen did not detect the gallbladder. There was no intra-or extrahepatic cholestasis but a stone with a diameter of 30 mm was suspected in the duodenum. A plain abdominal x-ray in erect position (Figure 1A) showed no extraluminal gas or dilatation of the small or large bowel. However, the extrahepatic bile ducts were positive for gas (arrow). An upper gastrointestinal endoscopy was performed and revealed a large gallstone with a diameter of 40 mm that filled the major part of the duodenal bulb (Figure 1B) Due to the stones’ size it was impossible to extract the intact stone and a mechanical lithotripsy using a lithotripter basket was performed. This procedure was complicated by the hard structure of the gallstone but disintegration was achieved and three fragments were removed employing a dormia basket. A fourth, largest fragment of the stone was retrieved employing an overtube to protect the esophagus and only a slight maceration with self-limited bleeding occurred. Subsequently, a duodenoscopy was performed that displayed a small cholecytoduodenal fistula (Figure 1C) Application of contrast media via the fistula revealed a small contracted gallbladder containing a second gallstone of 14 mm diameter but the cystic duct, the common bile duct and the intrahepatic bile ducts were free of calculi (Figure 1D) The patient underwent open cholecystectomy with closure of the cholecystoduodenal fistula. The patient made an uneventful recovery.
Panel A displays gas in the extrahepatic bile ducts on plain abdominal X-ray in erect position (arrow). Panel B shows a large gallstone that filled the major part of the duodenal bulb upon upper gastrointestinal endoscopy. Panel C displays the opening of a small cholecytoduodenal fistula upon duodenoscopy. In figure 1D, application of contrast media via the fistula is shown. The small contracted gallbladder contained a second gallstone whereas the cystic duct, the common bile duct and the intrahepatic bile ducts were free of calculi.
Duodenal obstruction due to a gallstone is an unusual complication of cholelithiasis. The condition is named after the french physician Léon Bouveret who documented a case of a gallstone leading to an obstruction of gastric outlet in 1896.1 Most gallstones in the intestine pass through the common bile duct and may cause cholestasis, cholangitis and biliary pancreatitis. In contrast, larger gallstones in the intestine usually indicate a fistula between the gallbladder and the bowel, most commonly the duodenum.2 Cholecystoenteric fistula occurs in < 1% of cases with gallstones and is further complicated by bowel obstruction in up to 20% of patients only.3 Due to the smallest diameter of the intestine at these sites, the most common locations of bowel obstruction are in the terminal ileum and at the ileocecal valve2 causing classic gallstone ileus. However, impaction of a gallstone at other sites is possible but obstruction of the duodenum is a rare event.2 In addition to signs and symptoms of ileus, most frequent radiological findings in cases of enterolithiasis are air in the biliary system as in our case ("pneumobilia"), bowel obstruction and the detection of an atypically located gallstone on plain abdominal film4 or on a computed tomographic scan.5 However, in only 50% of patients with enterolithiasis the diagnosis is made preoperatively,2 possibly because only approximately 15% of gallstones are radio-opaque on x-ray. In the patient described in our case, obstruction of the duodenal bulb was incomplete and given the large size of the gallstone caused only subtle signs of abdominal discomfort. Notably, bilious vomiting and gastric dilatation, the typical presentation of Bouveret’s syndrome, did not occur. Nevertheless, findings on abdominal ultrasound and pneumobilia on plain abdominal X-ray suggested the correct diagnosis that was confirmed by endoscopy.
The gross appearance of the fragmented gallstone in our case was a stone with a pigmented nucleus surrounded by light yellow material with a darker shell. The different appearances of the stones’ core and shell are probably due to their distinct chemical compositions and illustrate the pathophysiology of the fistula. Most likely, a noninfectious cholesterol gallstone had originated in the gallbladder and caused chronic cholecystitis. Chronic inflammation probably led to bacterial hydrolysis of biliary phospholipids and biliary pigments that precipitated as calcium salts of sparingly soluble lipids and calcium bilirubinate and formed the stones’ shell.6 This chronic inflammation of the gallbladder containing the large gallstone most likely led to adhesion of the gallbladder to the duodenum and facilitated the erosion of the stone through the gallbladder and duodenal wall and the formation of the fistula.
Gallstone ileus and Bouveret’s syndrome predominate in females and are diseases of the elderly with a mean age of 65-75 yrs.2 Surgical treatment with a one-stage or two-stage procedure consisting of enterolithotomy and cholecystectomy are the treatment of choice in most cases. However, this approach is associated with a substantial morbidity and mortality due to frequent comorbidities in this age group. Therefore, less invasive treatment is desirable and this renders endoscopy not only useful to confirm the diagnosis of Bouveret’s syndrome but also for endoscopic extraction of the stone. Subsequently, only cholecystectomy and closure of the fistula is required and in selected cases this may be achieved by laparoscopic surgery. The extent of surgery necessary in Bouveret’s syndrome is under debate but most authors agree that af-ter extraction of the gallstone from the intestine further treatment is required to prevent additional complications.2 In our case, cholecystectomy and closure of the fistula was necessary due to a second gallstone in the gallbladder that may have caused recurrence of gallstone ileus. Other possible complications in patients with cholecystoenteric fistulas include cholangitis, cholecystitis and possible malabsorption and weight loss. Furthermore, it appears that gallbladder cancer risk is increased among patients with fistulas versus patients undergoing cholecystectomy.7 To date, endoscopic treatment of Bouveret’s syndrome has been described employing electrohydraulic lithotripsy,8 extracorporal shock wave lithotripsy,9 and laserlithotripsy,10 as well as other endoscopic means. In our case it was possible to extract the gallstone following mechanical lithotripsy and this procedure proved to be safe and is applicable with standard equipment of interventional endoscopy. We conclude that in patients with upper abdominal pain and pneumobilia on x-ray the unusual complication of cholelithiasis with an impacted gallstone in the duodenal bulb should be considered. In those rare cases of Bouveret’s syndrome endoscopic removal of the gallstone should be attempted to minimize the necessary surgical procedure whenever possible.