Focal Nodular Hyperplasia (FNH) and Hepatic Adenoma (HA) are a benign tumors of the liver. The association with the use of oral contraception in women in middle age has been mentioned. This benign liver tumors are relatively rare lesions and are usually unrelated to subjective symptoms. They are increasingly being diagnosed as a result of the widespread use of ultrasound, computed tomography and magnetic resonance in the evaluation of patients with non-specific abdominal symptoms
Focal nodular hyperplasia (FNH) accounts for 8% of all primary tumors of the liver and is the second most common benign tumor of the liver after hemangioma. The prevalence of FNH is approximately 0.9%. FNH is more common in females (80%–95%) in the third or fourth decade of life. Some studies have shown that male FNH develops in median age.1
Benign liver tumors are relatively rare, but their diagnosis has increased in recent years because of increased use of ultrasound (US), computerized tomography (CT), and magnetic resonance imaging (MRI) for diagnosis of patients with nonspecific abdominal symptoms.1,2 The prevalence of FNH and hepatic adenoma has changed during recent years. Before 1989, the prevalence of these tumors was identical, but thereafter the prevalence of FNH increased because of an increase in the use of diagnostic imaging methods, such as US.3
Hepatic adenoma is extremely rare and is associated with the use of oral contraceptives, most frequently in women between 20 and 40 years of age. In a retrospective multi-institutional study conducted by the American College of Surgeons consisting of 226 benign liver tumors from 400 different hospitals, 212 (94%) of tumors were from women, of which 96 were hepatic adenomas, 58 were FNH, and 33 were hamartomas.5,6
Risk factorsUsing data collected after 1984, Drs Fitz and Baum described an association between the use of oral contraceptives and FNH. Oral contraceptives have been established as risk factors for the development of FNH and hepatic adenoma, but the pathogenesis of these associations has not been determined. As the risk for patients using oral contraceptives of developing hepatic adenoma is low, it has been suggested that genetic predisposition may play a role in this association.5,6 Some studies suggest that the duration of the use of oral contraceptives is an important risk factor; the use of oral contraceptives for 5-7 years is associated with a fivefold increase in the risk of developing hepatic adenoma, and the use of oral contraceptives for nine years or more is associated with a 25-fold increase. The significance of this association is illustrated by the fact that more than 50 million women in the United States use oral contraceptives.
Hepatic adenoma is associated with two types of synthetic estrogen and progesterone contained in oral contraceptives. The evidence indicates that estrogen consumption is the primary risk factor for development of hepatic adenoma. The growth of this type of tumor may be dependent on hormone use because some studies have shown that suspension of the use of oral contraceptives diminishes tumor size and pregnancy increases tumor size. Other risk factors for hepatic adenoma include the use of anabolic steroids and metabolic diseases such as type 1 glucogenosis.10
Whelean et al. mentioned that FNH may be caused by a congenital abnormality that causes biliary damage and that tumor growth may result from regenerative changes in such cases.8-10
Clinical manifestationsThe clinical manifestations of these tumors vary; they may be asymptomatic or may present as acute abdominal pain. Asymptomatic cases are usually detected incidentally during routine physical examinations or imaging studies. Only a third of FNH cases are diagnosed because the most frequent symptoms are epigastric abdominal pain, abdominal mass, and hepatomegaly. One of the most frequent findings in women with benign liver tumors, secondary to oral contraceptive use, is bleeding from the tumor. FNH is observed as a solitary nodule in 78% of patients and has a mean diameter of 5 cm in 84% of cases.
In a study at the University of California at San Francisco in which clinical and histopathological indices of 17 patients with benign liver tumors were monitored, seven had hepatic adenomas, six had FNH, and four were not included in the dataset because of lack of information. Differences between patients with hepatic adenoma and FNH are presented in table I. Hepatic adenoma had an initial presentation of intense abdominal epigastric pain and fever in 35% of cases because of tumor rupture. In 5% of cases, the discovery of hepatic adenomas was incidental. The histopathological characteristics of hepatic adenoma include large diameter, homogeneity, encapsulation, no change in the number of hepatocytes, absence of Kupffer cells, and thin vasculature. FNH was predominant in women 22-50 years of age; the primary symptom was chronic abdominal pain, and in some cases, acute abdominal pain was present. In FNH patients, no symptoms were observed during menstruation, but in hepatic adenoma patients, all symptoms were observed during menstruation (Table II).
Clinical and histopathological differences between hepatic adenoma and focal nodular hyperplasia (FNH).
| Characteristics | Hepatic Adenoma | FNH |
|---|---|---|
| Age | 20–40 | Same for all |
| Gender | 95% women | 60% women |
| Oral Contraceptive use | Frequent | Common |
| Shock or rupture | 35% | < 1% |
| Hemorrhage | 25% | < 1% |
| Abdominal pain | Common | Common |
| Palpable mass | Common | Common |
| Incidental | 5% | > 80% |
| Appearance | Large homogeneous | Central stellar scar |
| Hemorrhage | Common | Rare |
| Fibrosis | Absent | Present |
| Capsular | Present | Absent |
| Hepatocytes | Normal | Normal |
| Biliary canalicules | Absent | Proliferative |
| Kupffer cells | Absent | Present |
| Vasculature | Large and thin with diminished intravascular space | Intimal and medial changes |
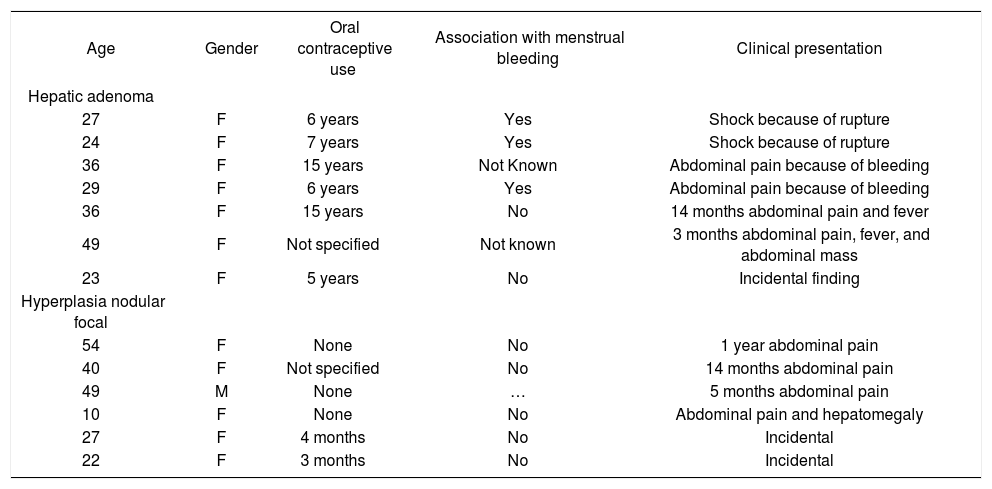
Clinical presentation of hepatic adenoma and FNH.
| Age | Gender | Oral contraceptive use | Association with menstrual bleeding | Clinical presentation |
|---|---|---|---|---|
| Hepatic adenoma | ||||
| 27 | F | 6 years | Yes | Shock because of rupture |
| 24 | F | 7 years | Yes | Shock because of rupture |
| 36 | F | 15 years | Not Known | Abdominal pain because of bleeding |
| 29 | F | 6 years | Yes | Abdominal pain because of bleeding |
| 36 | F | 15 years | No | 14 months abdominal pain and fever |
| 49 | F | Not specified | Not known | 3 months abdominal pain, fever, and abdominal mass |
| 23 | F | 5 years | No | Incidental finding |
| Hyperplasia nodular focal | ||||
| 54 | F | None | No | 1 year abdominal pain |
| 40 | F | Not specified | No | 14 months abdominal pain |
| 49 | M | None | … | 5 months abdominal pain |
| 10 | F | None | No | Abdominal pain and hepatomegaly |
| 27 | F | 4 months | No | Incidental |
| 22 | F | 3 months | No | Incidental |
Klastskin et al. mentioned that increased vasculature and tumoral bleeding occurs in patients using oral contraceptives (medical staff conference). In the study of Nime et al., which included 94 cases of benign liver tumor, it was shown that patients with FNH who were using oral contraceptives had large tumors with enhanced vasculature. Fibrosis and peliosis were observed more frequently in FNH patients who did not use oral contraceptives. Tumoral bleeding, peliosis, and fibrosis were observed more frequently in patients with hepatic adenoma compared with patients with FNH (Table I).11-13
Laboratory studiesAlfa-fetoprotein levels are normal in FNH and hepatic adenoma patients. Only 50% of cases have elevated levels of gamma glutamyl transpeptidase. Other laboratory indices are normal.10,11
PathogenesisThe pathogenesis of FNH is not well characterized. FNH is considered secondary to a hyperplasic response to a regenerative nonneoplasic nodule caused by a congenital vascular malformation. FNH lesions are usually solitary (80%) with diameters > 5 cm. Histological characteristics include a connective tissue central stellar scar with a large arterial vessel and a septum.
The hepatic parenchyma between the septum is composed of hepatocytes, sinusoids, and Kupffer cells. FNHs do not have tumoral capsules, but are separated from normal parenchyma by a pseudocapsule, which may surround the lesions. FNH pseudocapsules contain perilesional blood vessels and are inflamed because of parenchymal nodular compression. Proliferation of biliary ducts may be observed and the general appearance of the nodule is similar to that observed in cirrhosis.
The histopathology of the central lesions of FNH can resemble that of hepatocellular carcinoma, hemangioma, cholangiocarcinoma, or hepatic metastasis. When the size of the tumor is > 10 cm, typical symptoms and normal hepatic function are observed. Occasionally, FNHs are pedunculated; these tumors are classified as classic and non-classic, of which the classic type accounts for 80% of cases (Figure 1).2
FNHs are generally lobulate and noncapsulated. Hemorrhage and necrosis are rare. At the microscopic level, a fibrotic central zone composed of connective tissue, proliferating cells, altered biliary structures, perilesional inflammatory cells, and numerous vessels can be observed. Mallory bodies and periseptal augmented adipose tissue can also be observed in some cases.
Nonclassic FNHs constitute 20% of all lesions and are classed into three subtypes:
a) telangectasic;
b) atypical; and
c) mixed: hyperplasic or adenomatous.
Nonclassic FNH has no blood vessels, but always has biliary duct proliferation in the architecture of the nodule. The appearance of nonclassic FNH is more heterogeneous than classic FNH and is similar to that of an adenomatous pathology. Central scars are rarely observed.
Hepatic adenomas are generally solitary, of soft consistency, light brown or yellow in color, well circumscribed, and may or may not have a capsule. Occasionally, two or more tumors can be present at the same time. Tumor size is variable with a range of 1-30 cm (usually 8-15 cm) in diameter (Figure 2). These tumors usually occupy subcapsular positions, have superficial projections, are occasionally pedunculated, and are never nodular or fibrotic. Cells occasionally have acinar arrangements, and may contain eosinophilic inclusions, alfa-1-antitripsin, focal sinusoidal dilatation, and a reduced number of Kupffer cells. Low numbers of portal tracts or central veins and an absence of biliary ducts may also be observed. Blood vessels have thin walls with vascular abnormalities and occasionally have thromboses. Hepatic peliosis may also be observed.13-15
Imaging studiesDespite advances in radiological imaging (US, CT, and MRI) and the ability to detect the presence of hepatic masses, it is still difficult to distinguish between benign and malignant masses. Even hepatic percutaneous biopsy has low diagnostic sensitivity (60%–82%) for diffuse and local hepatic lesions.
FNH US characteristics include a hypoechoic or isoechoic mass with displacement of vessels and a lobulated outline. A central scar is detected as a thin hyperechoic zone and is only observed in 20% of cases. Doppler US is useful for determining the presence of this tumor and facilitates detection of central arteries with typical spokes (arterial hypervascularity and centrifugal filling to the periphery).
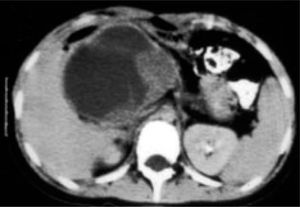
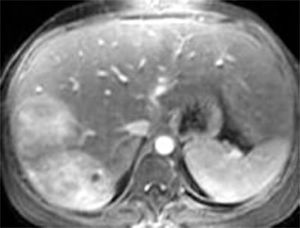
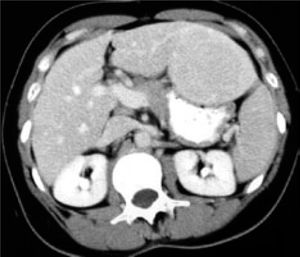
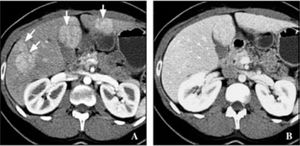
Contrast abdominal CT shows a focal hypodense or isodense mass. A helicoidal CT finding typical of FNH is the presence of a mass with a homogeneous pseudocapsule and a central scar (Figures 3,4,5and6).16,17
US and CT will usually identify the lessions without difficulty in hepatic adenoma bacause of its lake Kupffer cells, it will present as a defect on radiactive sulfur colloid scan. There are no diagnostic findings on ultrasound of CT. The lesion is hypervascular which can be noted on MRE. Angiography may demonstrate large peripheral vessels with centrifugal flow, central avascular scar may be present due to internal hemorrage (Figures 4and5). However, some adenomas will be hypovascular.
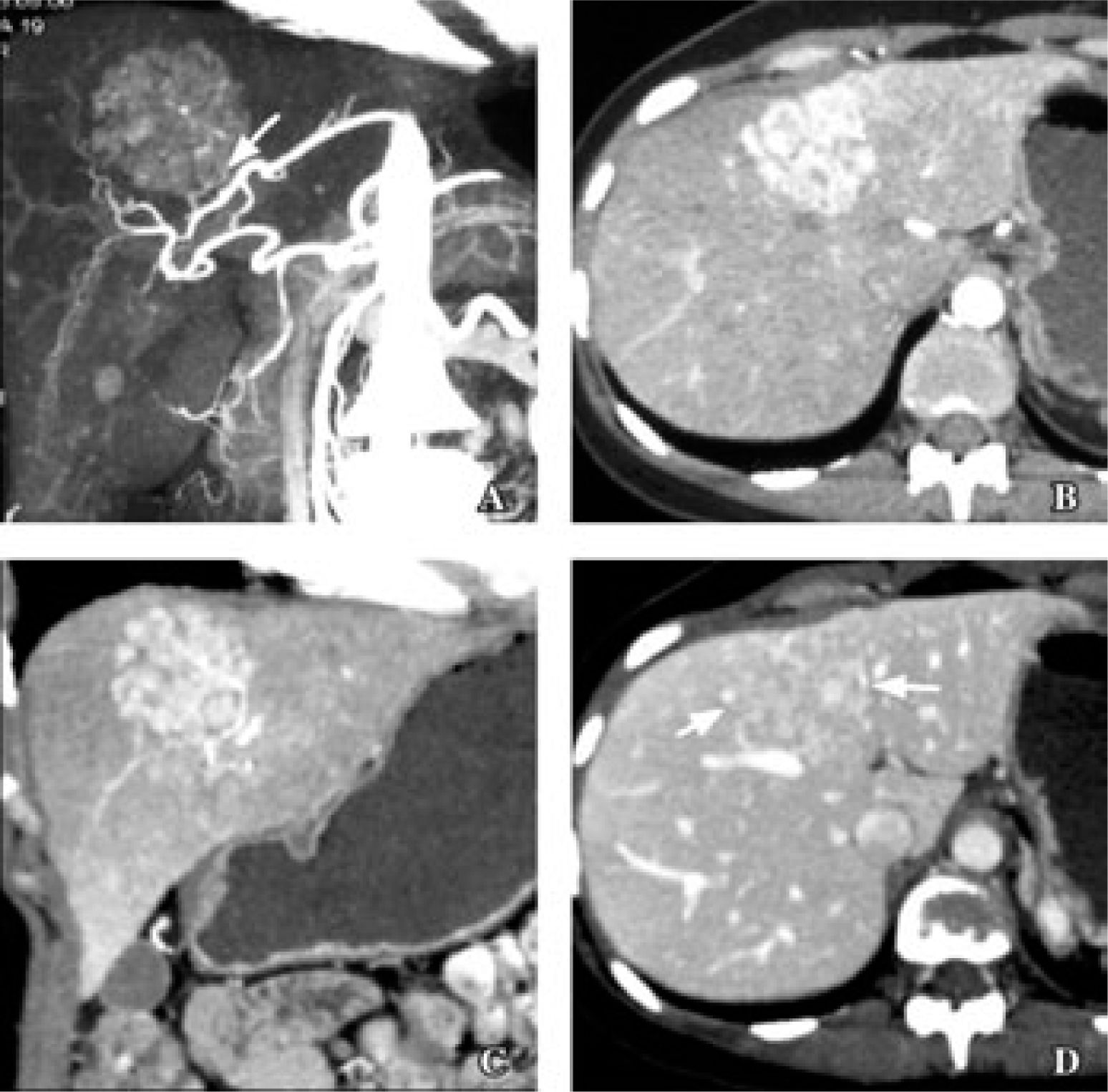
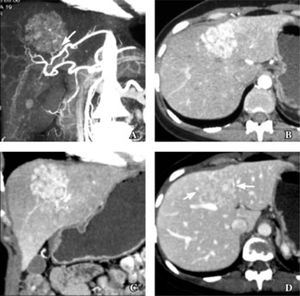
Recently, the results of 16-MDCT angiographic studies, in which angiographic characteristics of lesions can be determined, were reported. In one study in which the primary objective was to determine image features characteristic of FNH, the patients received 750 mL of water as a contrast 15 minutes before the study, 250 ml of water immediately before the study, and then 120-140 mL (2 mL/kg body mass) IV iohexol for more precise diagnosis (Figures 7and8).
35 years old woman with focal nodular hyperplasia. A. Coronal maximum intensity projection image in arterial phase shows small branch from replaced left hepatic artery (arrow) supplying dome lesion. B and C. Axial (B) and coronal (C) multiplanar reconstruction in arterial phase show reticular patern of enhancement typical of focal nodular hyperplasia. D. Reticular pattern in less conspicuous in portal venous phase (arrows).
Once a FNH of the liver is diagnosed, there are many direct strategies available for treatment, including surgical intervention. Symptoms are difficult to associate with the presence of a hepatic mass and have to be distinguished from those of extrahepatic pathologies. Generally, the presence of symptoms such as abdominal pain, obstructive jaundice, tumor rupture, and bleeding indicate a need for surgical intervention. When the presence of a malignant tumor cannot be excluded, a hepatectomy is suggested.18-20
Historically, hepatic surgery has been associated with higher rates of morbidity and mortality. Currently, advances in anesthesia, surgical techniques, and postoperative care have resulted in a better prognosis after hepatic surgery, the primary treatment for benign symptomatic tumors of the liver.21