Focal nodular hyperplasia (FNH) and hemangioma are benign and generally asymptomatic hepatic tumors. With distinctive imaging findings on dynamic computed tomography (CT) and magnetic resonance imaging (MRI), differentiation of these benign hepatic tumors from metastases can be made. We described imaging findings of these hepatic lesions in a 57-year-old man who presented with rectal adenocarcinoma for staging.
Focal nodular hyperplasia (FNH) and hemangioma are benign and generally asymptomatic hepatic tumors that are increasingly being discovered as incidental findings with the use of imaging tests.1 These two types of benign hepatic tumors sometimes coexist. Knowing the imaging findings of FNH and hemangioma is important to differentiate them from each other and from the other malignant pathologies. In this report we described computed tomography (CT) and magnetic resonance imaging (MRI) findings of FNH and hemangioma in a patient.
A 57-year-old man was referred to our department for staging of his endoscopically proved rectal adenocarcinoma. IV and rectal contrast-enhanced abdominopelvic CT was performed. In the early arterial phase images there was a homogenously enhancing lesion in segment 2 and a hypodense lesion in segment 1 (Figure 1). For characterization of the lesions, dynamic contrast-enhanced MRI was performed. On T2-weighted HASTE images, the lesion in segment 2 was isointense compared to liver parenchyma and the lesion in segment 1 was strongly hyperintense (Figure 2). On T1-weighted non-enhanced images the first lesion was iso-hypointense with a hypointense central scar and the second lesion was hypointense (Figure 3). In portal phase images there was peripheral capsular and central scar enhancement in the first lesion and peripheral noduler enhancement in the second lesion (Figure 4). Based on these signal characteristics and contrast enhancement patterns of the lesions, the diagnosis of the first lesion was FNH and the second lesion was hemangioma.
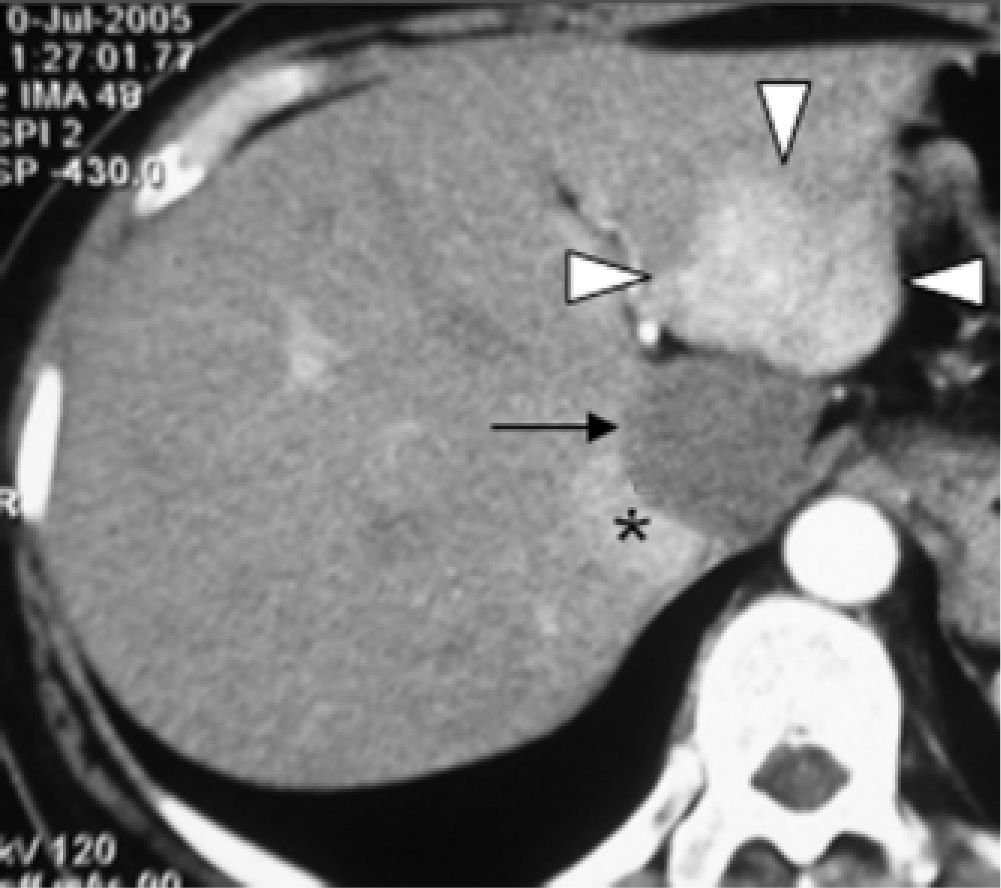
T1-weighted precontrast FLASH 3D MR image shows isoor mildly hypointense FNH lesion (arrowheads). Moreover there was a hypointense lineer central scar (white arrow) in the FNH. MR image shows hepatic hemangioma (black arrow) to be hypointense to surrounding liver parenchyma. Vena cava inferior (*).
Gadolinium-enhanced T1-weighted FLASH 3D MR image obtained during portal venous phase shows isointensity of FNH lesion (arrowheads) with enhancement of pseudocapsule and central scar (white arrow). The same image shows peripheral nodular shaped filling of hemangioma (black arrow). Vena cava inferior (*).
The liver is the most common site of metastases that arise from gastrointestinal malignancies.2 Differentiating metastasis from benign pathologies is very important for staging the primary disease. On CT most metastases are revealed as low- or isoattenuating masses. On MRI metastases are commonly appear hypointense on T1-weighted images and slightly hyperintense on T2-weighted images. Most metastases are hypovascular like colorectal carcinoma metastases. In dynamic CT and MR images during the arterial phase metastases show complete ring of enhancement whereas during the portal venous phase of imaging, thickened rind enhances progressively but to a lesser extent than liver.3,4
In our case the lesion in segment 1 demonstrates nodular peripheral enhancement on early-phase images with subsequent fill-in centrally which is a characteristic feature for hemangiomas that helps to differentiate them from metastases showing complete ring enhancement. The other lesion in segment 2 is isointense on T1 and T2 weighted images. In dynamic images the lesion shows intense homogeneous enhancement in the arterial phase and enhancement of the central scar in the later phases which is characteristic for FNH.5
These distinctive features of hemangioma and FNH that also help to differentiate them from metastases are clearly demonstrated in our case with these two benign lesions adjacent to each other.