Background & aims. Hemorrhagic rupture is an extremely rare complication of hepatic cyst. Its incidence, gravity and treatment modalities are inadequately covered in the literature.
Material and methods. Based on a case report concerning a 37 year-old, 13-weeks pregnant woman, presenting with hemorrhagic shock subsequent to hemorrhagic rupture of a hepatic cyst and requiring urgent surgery, a review of the literature was conducted.
Results. To date, 11 cases have been described in the literature. This complication is particularly serious with six cases of hemorrhagic shock, three of which led to death. In the majority of cases, urgent surgical treatment is required.
Conclusions. Hepatic cysts are frequent benign tumors of the liver which are most often discovered fortuitously. Hemorrhagic rupture is the rarest associated complication, yet requires to be known for it is both serious and lethal and necessitates urgent surgical intervention.
Hepatic cyst is a frequent, typically asymptomatic, benign tumor of the liver, the estimated prevalence of which ranges from 2.5 and 4.7%.1 Complications include, in order of occurrence: compression (biliary, vascular, digestive, pulmonary) in 3 to 9% of cases,2 intracystic hemorrhage in 2 to 5% of cases,3 infection in 1% of cases3 and, far rarer, intra- or extra-peritoneal cyst rupture. These complications are generally minor and are easy to treat. We report the extremely rare case of hemorrhagic rupture leading to hemorrhagic shock in a pregnant woman.
Case ReportA 37 year-old woman, in her 13th week of pregnancy attended the emergency department of a regional hospital following two weeks of pain in the right hypochondrium, accentuated over 24 h by a sensation of abnormal increase of her abdominal diameter. Her past medical history included uncomplicated vaginal delivery childbirth 1 year previously. Clinical examination revealed tenderness in the right subcostal region and hepatomegaly.
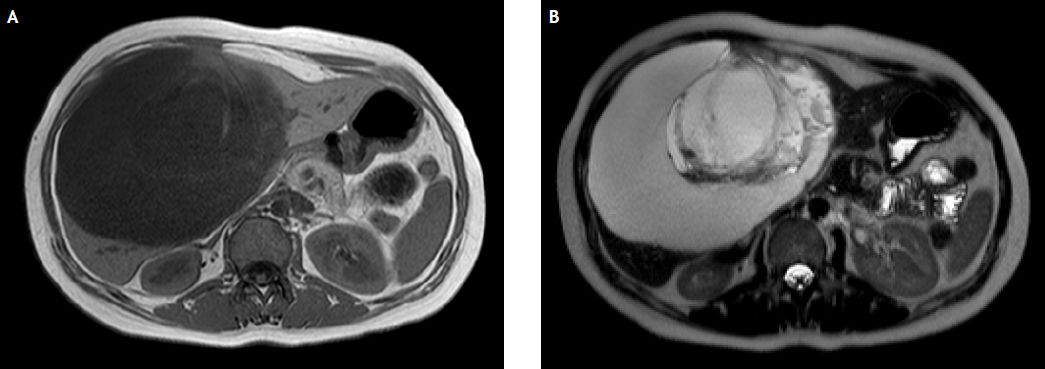
Biological analyses revealed a hemoglobin level of 11.8 g/dL, C-reactive protein (CRP) level of 15 mg/L, liver enzymes and all other analyses being normal. Abdominal ultrasonography revealed a normal evolutive pregnancy and a heterogeneous hepatic mass of a diameter of 15 cm. The patient was clinically stable and was discharged with an MRI prescription. MRI, performed the following day, revealed an 18 × 18 × 15 cm lesion in the right liver, with clear and regular contours (Figure 1), inducing upward compression of the liver. The lesion was filled with fluid and contained, in its central zone, a 7 cm heterogeneous lamellar mass. No contrasting agent was injected due to pregnancy. Radiologists concluded on a mass of unknown etiology evocative of an adenoma type benign tumoral mass and the patient was referred for specialized consultation. Two days later, she was urgently transferred to Caen University Hospital following an increase in acute pain associated with pallor and dyspnea. Upon arrival, the patient was in hemodynamic shock. Biological analyses revealed anemia (5.8 g/dL), ultrasonography confirmed the 18 cm lesion attached to segment IV with extensive intraperitoneal effusion. Urgent laparotomy was performed.
Surgical exploration revealed abundant hemoperitoneum of a volume of 1.3 L and a voluminous ruptured right hepatic cyst filled with blood clots. After evacuation of all blood clots, extensive bleeding was observed on the cyst wall. After hemostasis, the cyst wall was resected and sent to the laboratory for analysis. During surgery, the patient received 5 packs of red blood cells, 5 packs of plasma and 1 platelet concentrate. The post-operative period was uneventful and included an ultrasound control of pregnancy revealing excellent fetal vitality and discharge was possible after 6 days.
Anatomopathological analyses described a hemorrhagic and abraded cystic lesion compatible with a modified biliary cyst.
DiscussionHepatic cysts are frequent and intracystic hemorrhagic complications are largely described in the literature. This type of bleeding, which is typically benign, generating no biological consequences, can go unnoticed or can provoke brutal and regressive pain. Diagnosis is generally easily confirmed by ultrasonography or CT scan which reveal an increase in cyst volume and intrinsic heterogeneity of the lesion. The only problem, in case of this atypical cyst, is to eliminate cystadenoma or cystic necrotic tumor.4 In our own observation, the presence of intracystic blood clots and the context of pregnancy led to the initial error in diagnosis.
Cyst ruptures are far rarer and are generally associated with a brutal increase in volume or with infection which weakens the cyst wall. Miliadis, et al., describe only 15 cases of rupture in the English literature,5,6 of which only 5 cases, with an initial clinical picture involving an acutely painful abdomen requiring urgent surgery.
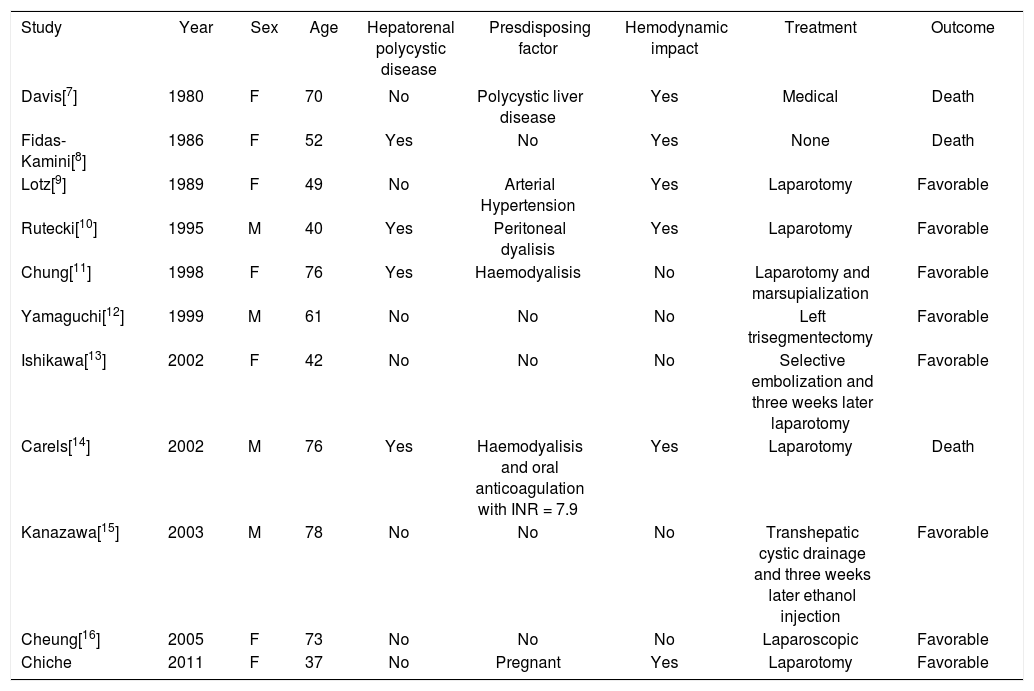
The association of cystic hemorrhage and rupture is the rarest complication of hepatic cyst. Following an overview of the literature, to our knowledge, 11 cases have been described including our patient (Table 1). The pathogenesis of this complication has not yet been clearly established. The outer layers of the cyst wall comprise a number of blood vessels. The progressive increase in cyst volume through secretion of the biliary epithelium increases intracystic pressure which probably induces necrosis in internal layers, hence exposing blood vessels to alterations in their outer wall and, consequently, intracystic bleeding.17 This bleeding, which is generally rapidly contained and stopped by intracystic pressure is no longer restrained in the case of cyst rupture and can therefore become a serious threat.
Literature review for the association of cyst hemorrhage and rupture in hepatic cyst.
| Study | Year | Sex | Age | Hepatorenal polycystic disease | Presdisposing factor | Hemodynamic impact | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Davis[7] | 1980 | F | 70 | No | Polycystic liver disease | Yes | Medical | Death |
| Fidas-Kamini[8] | 1986 | F | 52 | Yes | No | Yes | None | Death |
| Lotz[9] | 1989 | F | 49 | No | Arterial Hypertension | Yes | Laparotomy | Favorable |
| Rutecki[10] | 1995 | M | 40 | Yes | Peritoneal dyalisis | Yes | Laparotomy | Favorable |
| Chung[11] | 1998 | F | 76 | Yes | Haemodyalisis | No | Laparotomy and marsupialization | Favorable |
| Yamaguchi[12] | 1999 | M | 61 | No | No | No | Left trisegmentectomy | Favorable |
| Ishikawa[13] | 2002 | F | 42 | No | No | No | Selective embolization and three weeks later laparotomy | Favorable |
| Carels[14] | 2002 | M | 76 | Yes | Haemodyalisis and oral anticoagulation with INR = 7.9 | Yes | Laparotomy | Death |
| Kanazawa[15] | 2003 | M | 78 | No | No | No | Transhepatic cystic drainage and three weeks later ethanol injection | Favorable |
| Cheung[16] | 2005 | F | 73 | No | No | No | Laparoscopic | Favorable |
| Chiche | 2011 | F | 37 | No | Pregnant | Yes | Laparotomy | Favorable |
This exceptional complication appears to occur preferentially in hepatorenal polycystic patients: 4 out of 11 cases in our review. The multilesional nature of polycystic disease and the long-term evolution of associated cysts is probably one of the factors explaining the greater frequency of cystic complications. Furthermore, underlying kidney disease can require anticoagulant treatment, which involves an increased iatrogenic risk. Carels, et al. describe a patient receiving acenocoumarol with major overdosage of anti-vitamin K (international standardized ratio = 7.9), which probably contributed towards the severity of intracystic bleeding.
In our review, it appears clear that hemorrhagic ruptures are particularly serious. Six patients presented with hemodynamic decompensation which led to death in 3 patients. This was the case in our own patient who presented with a severe clinical picture including massive and rapid deglobulization which, without urgent surgical intervention, would very probably have been fatal.
It consequently transpires that surgical intervention is a necessity in the case of hemodynamic decompensation. The absence of surgery led to 2 of the aforementioned deaths. To our knowledge, our patient is the only pregnant woman to have presented with hemorrhagic cyst rupture. Pathogenesis of increase in volume of cyst in pregnant women is unknown, as there are no datas in literature but probably linked to hormonal changes as it is reported in case of hepatorenal polycystic disease.18–20 In fact in this genetic disease, an overexpression of estrogen receptors has been demonstrated in the hepatic cysts epithelium which is involved in cholangiocyte proliferation. Besides, patients treated with post-menopausal hormonal replacement therapy or oral contraceptive have an increase in size and number of hepatic cysts, and pluriparae are at greater risk to develop hepatic cysts than multiparae.20
An fortitious detection of a large hepatic cyst during pregnancy is therefore difficult to manage. Close ultrasound follow up is safe to recommend, with education of pregnant women to non-specific symptoms such as pain and hemorrhage signs. In case of symptomatic or increasing size cyst in pregnant woman, surgical treatment should be discussed.
The risk of rupture of the cyst wall is related to the intracystic pressure by secretion of the biliary epithelium, but not to the abdominal pressure.17 C section in case of discovery of a large cyst in a pregnant woman should not be mandatory.
Hepatic cysts are frequently benign lesions, rarely requiring surgery when complication free. Hemorrhagic rupture is a rare and serious complication which must be taken into account for it is potentially lethal and requires urgent surgical intervention.
Conflict of InterestThere is no conflict of interest statement for all authors.