Here we report a rare case of living Fasciola hepatica in biliary tract. The patient was in acute phase of infection and treated successfully with 10 mg/kg oral triclabendazole after the fluke was extracted using endoscopic retrograde cholangiopancreatography (ERCP).
Fascioliasis is a parasitic infection caused by Fasciola hepatica (F. hepatica) fluke worm which affects more than three millions of people worldwide.1 It occurs more frequently in some parts of Latin America, Eastern Europe, Far and Middle East (e.g. northern Iran) and can result in biliary tract obstruction, cholangitis, cholecystitis as well as pancreatitis and anemia.2-4
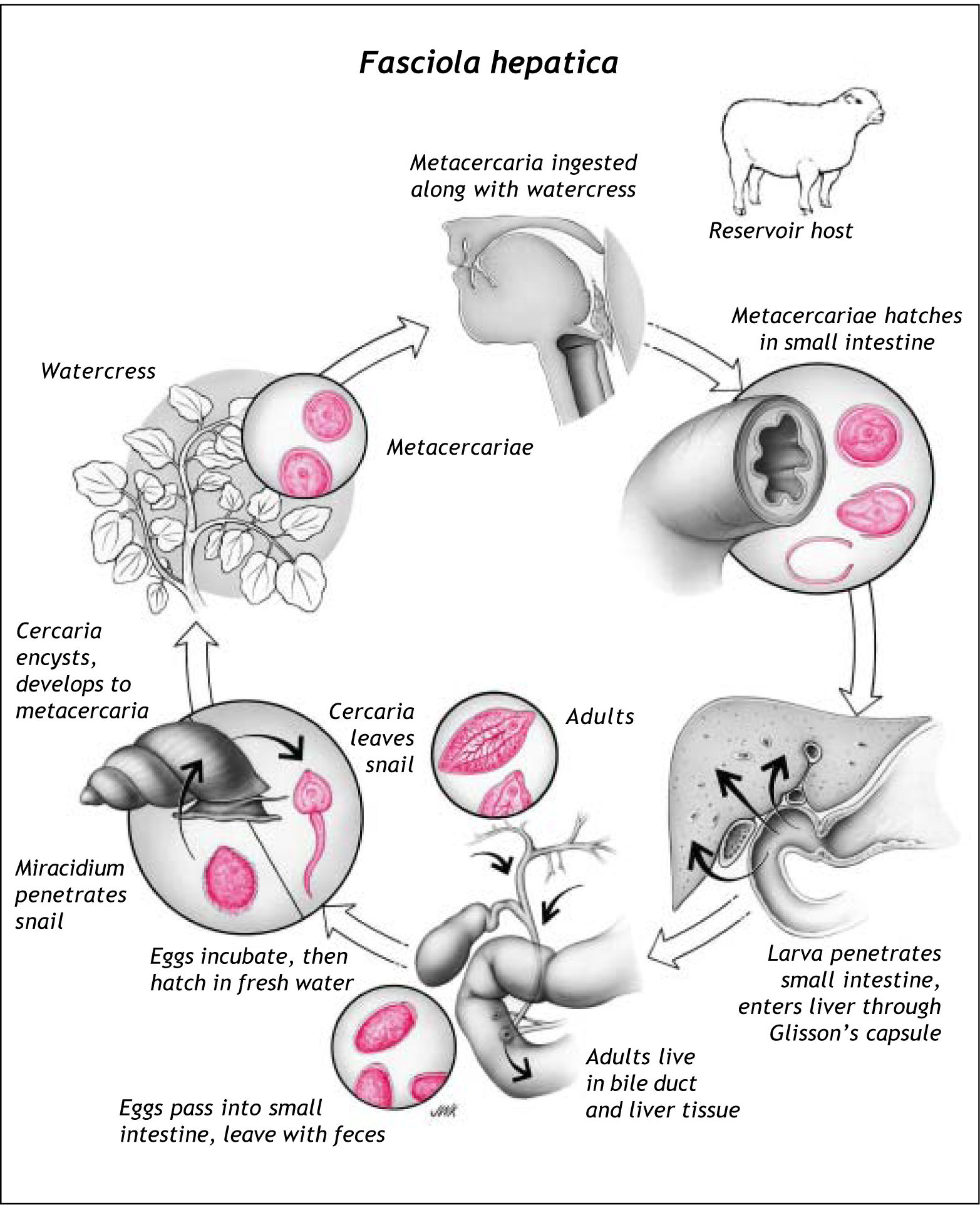
Humans may be accidental hosts of F. hepatica by ingestion of metacercariae during consumption of contaminated water or raw vegetables. In humans, maturation of metacercaria into adult fluke takes approximately 3 to 4 months (Figure 1). However, it is very rare to find a living fluke in the common bile duct (CBD) as it usually lives in gall-bladder and smaller biliary tracts.5
Herein we report a case of living F. hepatica in biliary tract without hepatobiliary damage that was found by endoscopic retrograde cholangiopancreato-graphy (ERCP).
Case ReportA 37-year-old woman referred to our clinic, Razi Hospital affiliated to Guilan University of Medical Sciences, Rasht, Iran, complaining of dull right upper quadrant (RUQ) abdominal pain for the last two weeks. There were no other symptoms like anorexia, weight loss, nausea, vomiting, cough, diarrhea, jaundice, urticaria, pruritus and arthralgia. On physical examination, mild RUQ tenderness and normal liver span were noticed.
In addition, laboratory findings revealed mild leu-kocytosis (WBC: 10,600/mm3) with remarkable eosi-nophilia (25%). Serum bilirubin, gamma-glutamyl transpeptidase (GGT), aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase (ALP) were within normal limits.
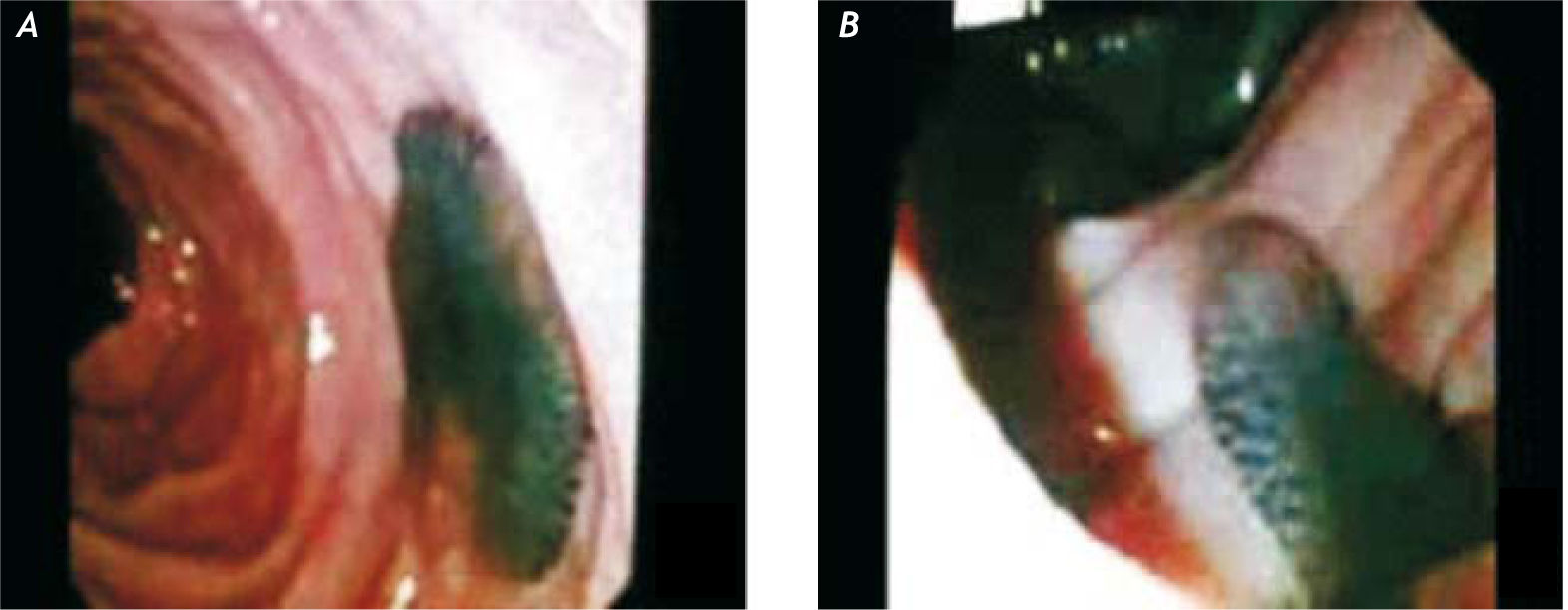
Ultrasonographic findings denoted normal hepatic parenchyma with dilated CBD. In ERCP, multiple irregular filling defects, some of which floating, were detected in the dilated CBD. After sphinctero-tomy and balloon extraction, a live fluke (F. hepatica) with some fragmented particles, suggestive of eggs, were detected in hepatopancreatic ampulla (Figure 2). The diagnosis was confirmed by increased titer of anti-Fasciola hepatica antibody.6
Therefore, a single dose of oral triclabendazole (10 mg/kg) was administered. Screening test using anti-Fasciola hepatica antibody was done for the patient’s family which found no parasitic infection within the family.
Two months later, symptoms improved and the patient had no symptoms with normal CBC and ul-trasonography.
DiscussionFascioliasis has uniquely crossed the borders of its origin, Europe, and resulted in WHO re-emerging programs in recent years.7 This can be due to the tremendous capability of the organism to live in very different regions, from the Andean mountains to the Caspian Sea and Southeast Asia. Moreover, climate and environmental changes induced by humans’ destructive processes may have affected snail-mediated parasitic infections.8
When an individual accidentally ingests the meta-cercariae on cyst-laden vegetables or in contaminated water, the excysted metacercaria, having survived from gastric acid and enzymes, penetrates the duodenal wall and invades the liver through peritoneum and Glisson’s capsule. After 5-6 weeks, the fluke immigrates to one of the liver’s bile ducts where it achieves sexual maturity. Thereafter, cross fertilization occurs in the bile ducts of the host and after about 12 weeks from first penetration to the host, encapsulated embryos are released into the bile capillaries from where they reach the intestine and are transported with feces. The embryos may survive for a few months in wet feces but without any development, which only takes place when the capsules come in contact with water. In optimum temperature (30 °C) the encapsulated embryo differentiates into miracidium larva within eight days.
Inside specific intermediate snail’s bodies, which lucky miracidium larvae reach, and after various changes, the sporocyst larva develops and then cercaria, which leaves the snail to surrounding water. Afterwards, it settles down on plant leaves where it turns to encysted cercaria called metacerca-ria. This young fluke may live for a year at low temperature and for two or three weeks at 25°C. Metacarearia grows up into adult fluke only inside its definitive host.
Fascioliasis comprises two main stages: acute or liver phase occurs for about eight weeks when immature larvae migrate from the small intestine to the liver and sometimes other organs through the peritoneum. At this stage, the excretory-secretory products synthesized by the fluke are responsible for anemia, diarrhea, eosinophilia and non-specific symptoms and signs. Chronic or biliary phase begins after the former phase during which immature larvae grow up and release eggs. In this period migrating metacercariae cause liver damage and therefore, necrosis and fibrosis can be observed in migratory tracks.9,10 The mature fluke can reach a width and length of 13 and 30 mm, respectively, and cause complications from recurrent cholangitis and anemia to biliary obstruction and hepatic abscesses or metastasis.11
In 2003, Ozer, et al. from Turkey reported a 52-year-old woman suffering from epigastric pain and some other non-specific symptoms. Additionally, she had elevated AST, ALT, ALP, GGT, WBC, conjugated bilirubin but no eosinophilia. In that case, three living F. hepatica were projected to the duodenum after sphincterotomy was performed by ERCP. Three years before, actually, she had presented with acute cholecystitis and thence, during cholecystec-tomy, a collection of F. hepatica had been noticed inside the gall-bladder and treated with a therapeutic oral agent.12 Similarly, Goenka, et al. reported a 28-year-old woman with raised liver function test (LFT) but not leukocytosis.13 Tang, et al. presented another 28-years-old woman from South America with elevated LFT, trivial eosinophilia but non-indicative biliary ultrasound.11 These findings were similar to the report of Ezzat, et al. as well, whose 38-year-old female patient from Sulaimanyah, Iraq, presented with raised LFT as well as dilated CBD but normal intrahepatic ducts.14
In contrast, our patient did not present hepatomegaly, cholangitis or elevated hepatic enzymes. She underwent ERCP due to the unexplained biliary dilatation observed in ultrasonography. Extraction of the fluke was necessary to prevent probable obstruction of CBD. Our report represented a patient with hepatobiliary fascioliasis with remarkable eosinophi-lia but no liver damage. In addition, her primary symptoms had started two weeks prior to admission, which is a little shorter than the time necessary for maturation of F. hepatica. Likewise, Keshishian, et al. reported a patient of biliary fascioliasis with normal laboratory findings.15
Additionally, Al Teimi’s 5 of 6 cases had long-term history of recurrent cholangitis and/or biliary colic,16 however, in a case series published by Sezgin, et al., only 1 patient from the 9 cases experienced this symptom.17
Apart from that, 10-year history of recurrent epigastric pain in a patient with pancreatitis reported by Veerappan, et al. reflects the potential creeping nature of this parasitic infection18 as el-Newili, et al. noted that a mature fluke can live in biliary tree up to 10 years.19
From the approach to treatment standpoint, positive outcomes of endoscopic treatment of hepatobi-liary fascioliasis from available brief reports and case series suggest it, along with oral triclabendazo-le, as the treatment of choice,9,17 even though adequacy and safety of endoscopic treatment of biliary fascioliasis has not been yet assessed through narrower studies.
This report means to draw the attention of clinicians worldwide to infection with living flukes in the biliary system that should be considered irrespective of duration of infection and range of abnormalities in clinical and paraclinical findings.
AcknowledgmentsThe authors are grateful to staff of Farzan Clinical Research Institute.
Abbreviations- •
ERCP: endoscopic retrograde cholangiopancrea-tography.
- •
F. hepatica: Fasciola hepatica.
- •
CBD: common bile duct.
- •
WBC: white blood cells.
- •
GGT: gamma-glutamyl transpeptidase.
- •
AST: aspartate aminotransferase.
- •
ALT: alanine aminotransferase.
- •
ALP: alkaline phosphatase.
- •
CBC: complete blood count.
- •
WHO: World Health Organization.
- •
LFT: liver function test.