There are few studies reporting pyogenic liver abscess (PLA) caused by Streptococcus constellatus in the medical literature. S. constellatus is a comensal microorganism that belongs to the Streptococcus milleri’s bacteria group and is not considered to be pathogenic for humans. We report the case of a 23-year-old man with a 15-days history of abdominal pain in the right flank followed by daily fever, chills, nausea, vomits, sialism and jaundice. Physical examination revealed moderate jaundice (2+/4+), abdominal distention, generalized pain and tender over the right flank with positive Blumberg’s sign. Additionally, the liver was palpable 5 cm below the costal margin in the right midclavicular line. Abdominal Computerized Tomography showed multiple hypodense hepatic images suggestive of liver abscesses. The patient underwent surgical exploration of the abdomen through a sub-costal incision and, during operation ruptured abscess localized on the hepatic segment III was drained. Culture of the purulent material obtained at surgery yielded Streptococcus constellatus as the causative agent. Liver abscess is a potential life-threatening disease that must be treated as soon as possible with invasive approaches, if necessary, and bacteriological studies performed when possible, allowing isolation of causative agents and specific antibiotic therapy.
Streptococcus constellatus is an anaerobic or micro-aerophilic germ that belongs to the Streptococcus milleri’s group, usually associated with respiratory infections.1,2 These bacteria colonize the mouth, superior airways, the intestinal and urogenital tracts, and are considered to be comensal rather than pathogenic.1-4 Although, there are many reports confirming liver abscesses secondary to germs of the S. milleri’s group, only few cases have been described indicating S. constellatus as the cause of such infections.
In the present report, we describe the first case in the Brazilian Amazon region of a young-adult that developed multiple abscesses in the liver caused by S. constellatus. The patient was successfully treated with surgical drainage of the abscesses and administration of broad-spectrum antibiotics.
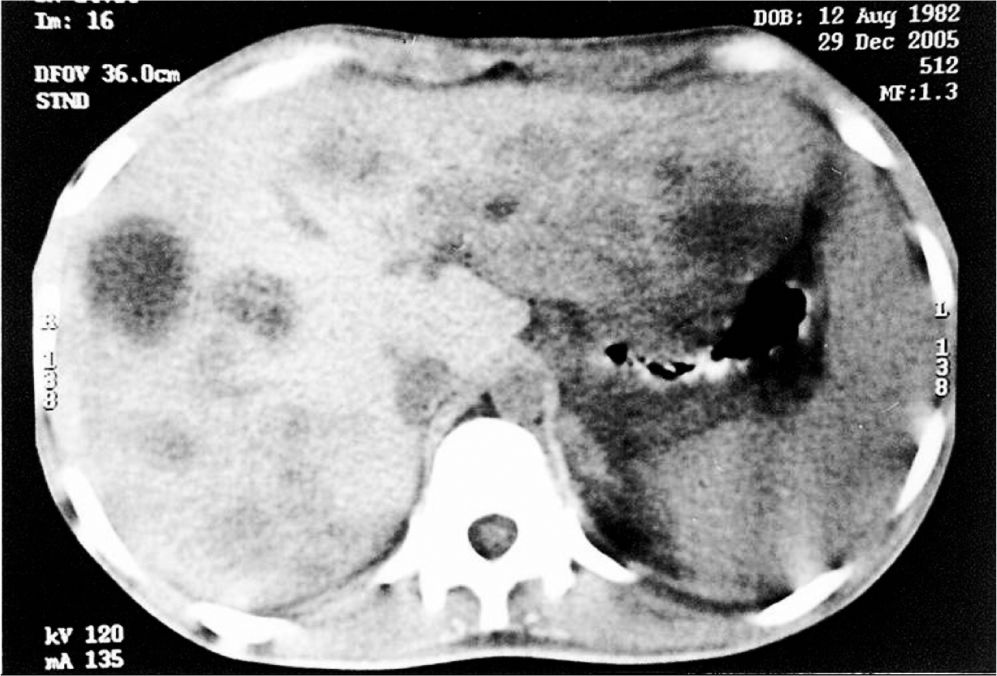
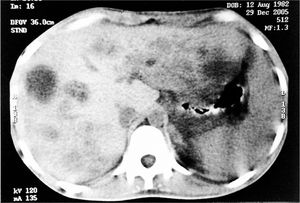
Case ReportA 23-year-old man, born and residing in the Brazilian Amazon region, was admitted presenting a 15-days history of abdominal pain on the right flank followed by daily fevers, chills, nausea, vomits, sialism and jaundice. His past medical history was unremarkable for any clinical or surgical disease. Upon physical examination, the patient demonstrated moderate jaundice (2+/4+), mucocutaneous paleness (2+/4+), abdominal distention and tender over the right flank with positive Blumberg’s sign. Additionally, the liver was palpable 5 cm below the costal margin in the right midclavicular line. Laboratory exams revealed leukocytosis and hyperbilirubinemia. Serologic investigation for hepatitis B, C and HIV were all negative. Chest radiography was normal. Ultrasonographic scanning of the abdomen showed various hypoecogenic nodular images in the liver. Abdominal computerized tomography (CT) revealed hypodense images in the liver suggestive of liver abscesses (Figure 1). As no other structural abnormality was found, a diagnosis of ruptured liver abscesses was suspected and the patient underwent urgent surgical exploration of the abdomen. A right sub-costal laparotomy was performed and, during operation, the liver was found to be enlarged with multiple abscesses of various sizes on its surface (Figure 2). A ruptured abscess was observed on the left lateral hepatic segment (Couinaud’s hepatic segment III) draining the purulent material to the peritoneum cavity (Figure 3). Drainage of most superficial abscesses was performed. After surgery, the patient was maintained with clinical support and intravenous broad-spectrum antibiotics (Ceftriaxon 1 g/day, Metronidazole 1.5 g/day and Ampicillin 8 g/day in) for 15 days. Culture of the purulent material obtained at the time of surgery yielded Streptococcus constellatus as the causative agent. The patient had an uneventful recovery and was discharged home on the sixteenth post-operative day in good clinical conditions with normal laboratorial parameters and resolving abscess seen on ultrasound. He received a 9-months course of antibiotic (Ciprofloxacin 1 g/day taken orally) with tomographic resolution seen after two years.
Streptococcus anginosus, Streptococcus intermedius and Streptococcus constellatus form the Streptococcus milleri’s group and, in normal conditions, are not associated with pathologic events in humans, except when any invasive manipulation is performed, such as endoscopy or surgical procedures.1-3 This group of microorganisms is characterized by the tendency to form abscesses in different organs and, in association with anaerobic germs, evolve diverse infectious processes, for example myocardial and pleural abscess.3 However, S. constellatus liver abscess is an uncommon event with only few reports documented in the English literature. Legout, et al.2 reported a case multiple liver abscesses secondary to diverticulitis in a woman. Brasitus, et al.5 reported two cases of liver abscesses caused by S. intermedius in patients diagnosed with Crohn’s Disease. In the present report, we were not able to identify any morbid predisposing condition that could justify a primary infectious site. The most accepted theory for the formation of liver abscesses by bacteria of the Streptococcus milleri’s group is that, since the bacteria belongs to the normal intestinal flora, the intestinal mucosa’s damage would act as a gateway for the dissemination of the microorganism through the portal blood stream, reaching the liver’s parenchyma provoking necrosis and abscesses formation.6 An interesting case was described by Paraskeva, et al.7 where the patient, after colonoscopic removal of a fish bone developed liver abscess by S. milleri. These reports support the physiopathologic theory of portal dissemination from intestinal lesion. However, other routes of bacterial dissemination through the biliary tract, by the systemic circulation through the hepatic artery and by a direct trauma to the liver may also be implicated in this disease.8
The symptoms related to liver abscesses are well known, with the patient presenting the clinical triad of fevers, pain on the right flank and hepatomegaly, eventually adding jaundice and signs of sepsis, just like oliguria, arterial hypotension and mental confusion, depending on each case. Ultrasound scanning, computerized tomography and magnetic resonance are useful in the evaluation of the patient with clinical abscesses.
Differential diagnosis of pyogenic abscesses of the liver must be done with amoebic and tuberculosis abscesses, especially in the Brazilian Amazon region, as well as with some less likely causes, such as actinomycosis. Hence, it is important to perform bacteriologic, microscopic and histologic exams of the abscess’ contents.
The treatment of pyogenic liver abscesses is still controversial and, depending on the clinical feature of the patient, it may be based on broad-spectrum antibiotic therapy for a long period, associated or not with percutaneous or surgical drainage. In our case, it was opted to perform surgical drainage due to a high clinical suspicion of abscess rupture. The treatment must be promptly instituted right after diagnosis, once the global mortality of pyogenic abscesses of the liver may reach 40% of all patients.6
In conclusion, liver abscesses must be treated as soon as possible, with invasive approaches, if necessary, and bacteriological studies performed when possible, allowing isolation of causative agents and specific antibiotic therapy.