An association between non-alcoholic fatty liver disease (NAFLD) and cardiovascular disease (CVD) has been recently suggested. Indeed, different studies have demonstrated that NAFLD patients present increased subclinical atherosclerosis compared to non-steatosic individuals, and are supported by the few follow-up studies revealing that CVD is the second most common cause of death in NAFLD patients. However, the nature of the relationship NAFLD/CVD is still under debate.
Non-Alcoholic Fatty Liver Disease (NAFLD) constitutes one of the most common forms of liver disease and is considered as the hepatic manifestation of the Metabolic Syndrome (MS)1 since it is also strongly associated to obesity and insulin resistance.
The severity of NAFLD ranges from hepatic steatosis alone to a triad constituted by: steatosis, hepatocellular necrosis, and inflammation; referred to as non alcoholic steatohepatitis (NASH).2
The true prevalence of NAFLD remains unknown. Among the difficulties in assesing NAFLD prevalence are the absence of signs and symptoms, the sensitivity of liver enzimes to indicate disease and the disputed need for histopatology (liver biopsy) as a gold standard for diagnosis. Depending on which specific diagnosis criteria are used, the prevalence of NAFLD is estimated to range between 10% and 24% in the general population. Variability arises from country to country; in Mexico, one of the largest NAFLD studies3 reported a frequency of 14.34% in the population between ages 15 and 80 years, compared to a prevalence of 10 to 24% reported in the United States.4
In cirrhotic patients5 liver-related causes of death are classically the main concern in clinical practice; most research is being developed in this field. The most important risk factors for the development of Cardiovascular Disease (CVD) in cirrhotic patients have been analyzed (except for those with primary biliary cirrhosis and nonalcoholic steatohepatitis), considering CVD is a new but less studied risk that will be increasingly common in this population due to the improved survival that has been observed worldwide. The first interesting finding was that the overall prevalence of MS in patients with liver cirrhosis was similar to that in patients without cirrhosis; although a lower prevalence was observed in male cir-rhotic patients. It is clear that MS is a significant clinical problem in this population, mainly because there are currently no specific guidelines for treatment of MS in patients with liver damage, and controlled clinical trials to prevent complications of MS do not include participants with liver cirrhosis.
Insulin resistance is the underlying condition that facilitates NAFLD’s occurrence and is the key patho-genetic event of obesity, type 2 Diabetes Mellitus and dyslipidemia. Recently, NAFLD has been included among components of the metabolic syndrome; condition that increases the risk of coronary heart disease and cardiovascular complications. A high prevalence of fatty liver, evaluated by ultrasound, associated with hyperinsulinemia or insulin resistance and cardiovascular disease, has been reported in the general population and in patients with documented coronary artery disease or stroke.
Carotid B mode ultrasound imaging has been used to evaluate carotid atherosclerosis. Intima-media thickness of the carotid artery, a valid parameter for detecting sub-clinical atherosclerosis, has been shown to predict myo-cardial infarction and stroke. Recently, a relationship between NAFLD and atherosclerosis has been reported in healthy man and it has been suggested to reflect the overall adverse impact of the metabolic syndrome, in particular of insulin resistance and increased visceral fat. Endot-helial dysfunction has been reported in NAFLD and re-lated to the metabolic syndrome.
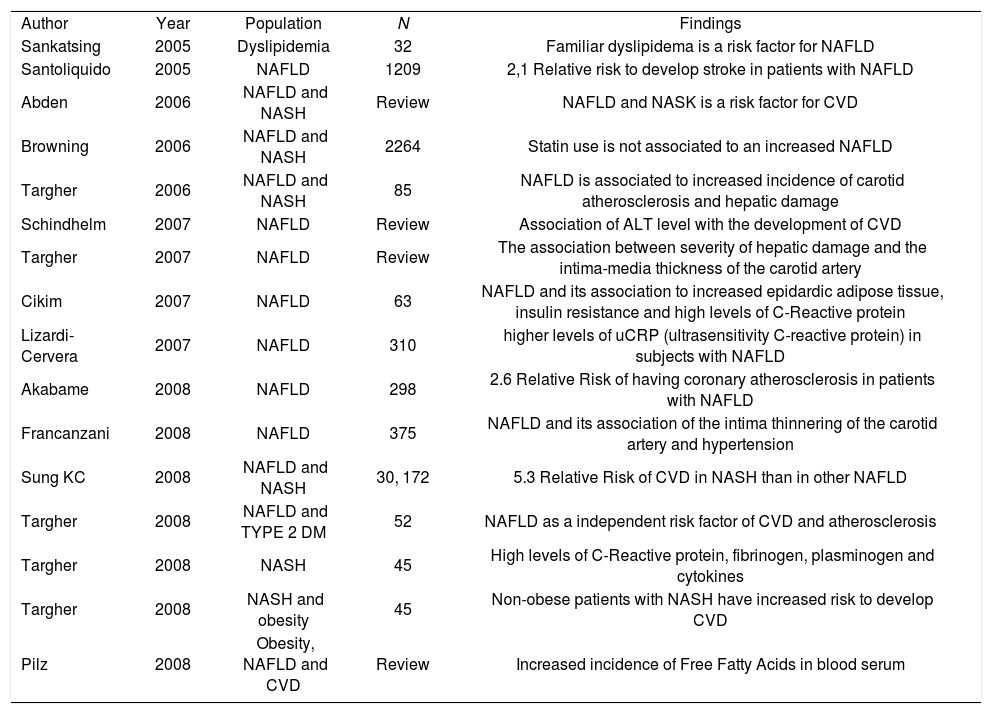
The main problemThe current importance of NAFLD and its relationship with the MS has stimulated an interest in the possible role of NAFLD in the development of atherosclerosis. Recent studies have reported the association of NAFLD with multiple classical and non-classical risk factors for CVD. Moreover, there is a strong association between the severity of liver histopathology in NAFLD patients and greater carotid artery intima-media thickness and plaque, and lower endothelial flow-mediated vasodilation (as markers of subclinical atherosclerosis) independently of obesity and other MS components.6,7Table I shows studies regarding to CVD and the presence of NAFLD and NASH.
Studies regarding to CVD and the presence of NAFLD and NASH.
| Author | Year | Population | N | Findings |
| Sankatsing | 2005 | Dyslipidemia | 32 | Familiar dyslipidema is a risk factor for NAFLD |
| Santoliquido | 2005 | NAFLD | 1209 | 2,1 Relative risk to develop stroke in patients with NAFLD |
| Abden | 2006 | NAFLD and NASH | Review | NAFLD and NASK is a risk factor for CVD |
| Browning | 2006 | NAFLD and NASH | 2264 | Statin use is not associated to an increased NAFLD |
| Targher | 2006 | NAFLD and NASH | 85 | NAFLD is associated to increased incidence of carotid atherosclerosis and hepatic damage |
| Schindhelm | 2007 | NAFLD | Review | Association of ALT level with the development of CVD |
| Targher | 2007 | NAFLD | Review | The association between severity of hepatic damage and the intima-media thickness of the carotid artery |
| Cikim | 2007 | NAFLD | 63 | NAFLD and its association to increased epidardic adipose tissue, insulin resistance and high levels of C-Reactive protein |
| Lizardi-Cervera | 2007 | NAFLD | 310 | higher levels of uCRP (ultrasensitivity C-reactive protein) in subjects with NAFLD |
| Akabame | 2008 | NAFLD | 298 | 2.6 Relative Risk of having coronary atherosclerosis in patients with NAFLD |
| Francanzani | 2008 | NAFLD | 375 | NAFLD and its association of the intima thinnering of the carotid artery and hypertension |
| Sung KC | 2008 | NAFLD and NASH | 30, 172 | 5.3 Relative Risk of CVD in NASH than in other NAFLD |
| Targher | 2008 | NAFLD and TYPE 2 DM | 52 | NAFLD as a independent risk factor of CVD and atherosclerosis |
| Targher | 2008 | NASH | 45 | High levels of C-Reactive protein, fibrinogen, plasminogen and cytokines |
| Targher | 2008 | NASH and obesity | 45 | Non-obese patients with NASH have increased risk to develop CVD |
| Pilz | 2008 | Obesity, NAFLD and CVD | Review | Increased incidence of Free Fatty Acids in blood serum |
The Free Fatty Acids (FFAs) are increased in obese patients and contribute to the development of type 2 Diabetes Mellitus, hepatic steatosis and several cardiovascular diseases. In patients with heart failure and acute coronary syndromes, elevated FFA levels are a consequence of an increased lipolysis due to a surge in catecholamines and natriuretic peptides. FFAs contribute to myocardial dysfunction and are proarrhythmic; also, their oxidation process requires more oxygen than glycolysis.8 More recently, several cross-sectional and prospective studies have demonstrated associations of this mechanism with features of the metabolic syndrome and type 2 diabetes mellitus.9
Several epidemiological studies indicate that NAFLD, especially in its more severe forms, is linked to an increased risk of CVD, independently of underlying cardi-ometabolic risk factors; Targher et al 10 found that NAFLD is not merely a marker of CVD, but it may be actively involved in its pathogenesis.
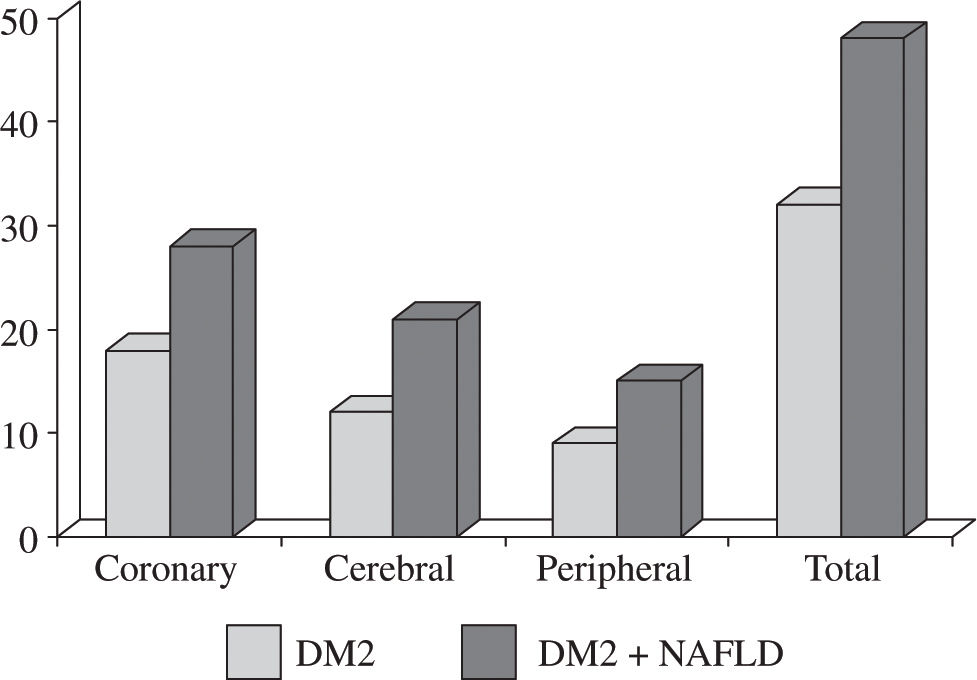
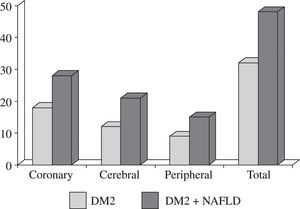
In the Diabetes Care work study from Targher,11 it was found that the prevalence of NAFLD increased with age in patients with type 2 diabetes; (65.4% in aged 40-59 years and 74.6% among those > 60 years; P < 0.001) and the age-adjusted prevalence of NAFLD was 71.1% in men and 68% in women. NAFLD patients had remarkably (P < 0.001) higher age and sex-adjusted prevalences of coronary (26.6% vs 18.3%), cerebrovascular (20.0% vs 13.3%), and peripheral (15.4% vs 10.0%) vascular disease than their counterparts without NAFLD (Figure 1).
Abdeen et al state that in the cardiometabolic syndrome (a constellation of metabolic, cardiovascular, renal, and inflammatory abnormalities in which insulin resistance is thought to play a key role in end-organ patho-genesis),12 the release of pro-atherogenic factors from the liver (C-reactive protein, fibrinogen, plasminogen activator inhibitor-1 and other inflammatory cytokines) as well as the contribution of NAFLD per se to whole-body insulin resistance and atherogenic dyslipidemia, favour CVD progression.
Plasma concentrations of high-sensitivity C-reactive protein (hs-CRP), fibrinogen, plasminogen activator in-hibitor-1 (PAI-1) activity, and adiponectin were reviewed by Targher et al in 45 overweight male patients with biopsy-proven NASH, 45 overweight male patients without ultrasound-diagnosed hepatic steatosis, and 45 healthy male volunteers;13 the lowest values were in nonobese healthy subjects, intermediate in overweight nonsteatotic patients, and the highest in those with biopsy-proven NASH; on the other hand, the highest and lowest adi-ponectin levels were found in nonobese healty subjects and in biopsy-proven NASH patients, respectively. In their review, they concluded that the presence of NASH can predict a more atherogenic risk profile in a manner that is partly independent from the contribution of visceral adiposity in adult men.
A large trial performed in Asia with 30,172 subjects studied the severity of NAFLD, characterized a nonobese population and analyzed the prevalence of CVD risk factors and used the Framingham risk score for CVD; the odds ratio for 10-year risk by total Framingham risk scores > 10% was 5.3 times higher in NASH groups. CVD risk was significantly greater in patients with NASH than in patients with either steatosis or raised ALT alone.14
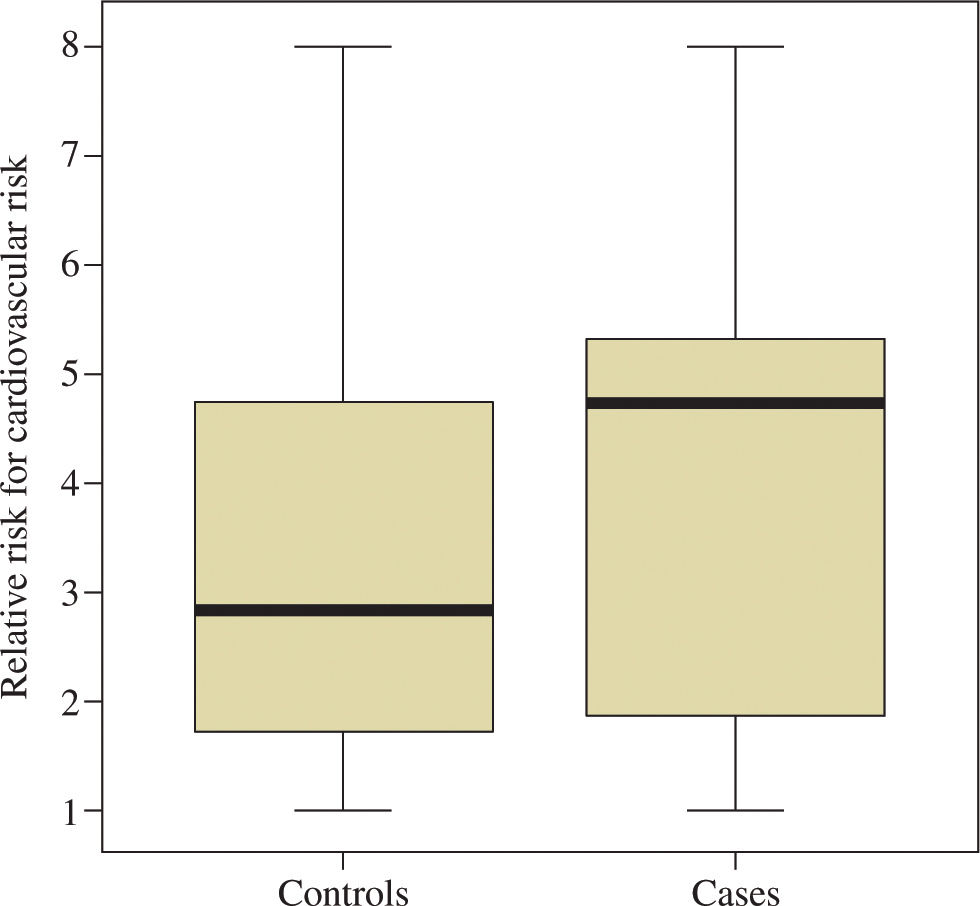
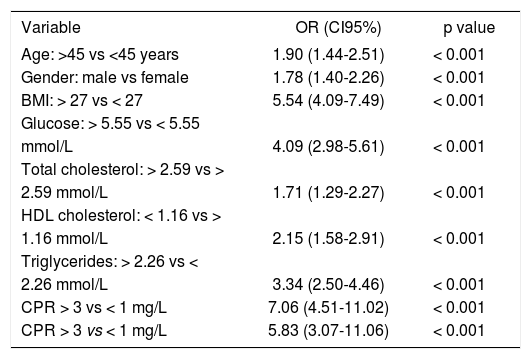
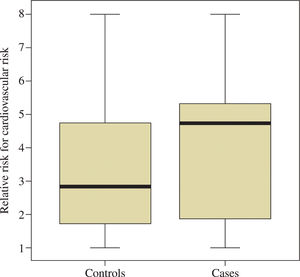
Lizardi-Cervera et al15 demonstrated that subjects with NAFLD had several forms of metabolic disturbances and a high prevalence of MS. They found higher levels of uCRP (ultrasensitivity C-reactive protein) in subjects with NAFLD and observed in this subjects had more metabolic abnormalities and a higher prevalence of MS; which explained the higher concentrations of uCRP. They compared 310 subjects with ultrasound-demonstrated steatosis to 610 control cases. They found statistically significant differences between both groups; the frequency of MS was 66.4% in the study population compared to 26.7% found in the control group (P < 0.001). Patients in the steatosis group were older, had higher BMIs, glucose, total cholesterol and triglycerides (P < 0.001), as well as mean uCRP concentrations (4.5 vs 2.79 mg/L; P < 0.001) (Table II). Cardiovascular risk was also higher in subjects with NAFLD (4.7 vs 2.8) (Figure 2).
Univariated and multivariated analysis of anthropometric and metabolic variables and C reactive protein values according to cardiovascular risk.
| Variable | OR (CI95%) | p value |
|---|---|---|
| Age: >45 vs <45 years | 1.90 (1.44-2.51) | < 0.001 |
| Gender: male vs female | 1.78 (1.40-2.26) | < 0.001 |
| BMI: > 27 vs < 27 | 5.54 (4.09-7.49) | < 0.001 |
| Glucose: > 5.55 vs < 5.55 | ||
| mmol/L | 4.09 (2.98-5.61) | < 0.001 |
| Total cholesterol: > 2.59 vs > | ||
| 2.59 mmol/L | 1.71 (1.29-2.27) | < 0.001 |
| HDL cholesterol: < 1.16 vs > | ||
| 1.16 mmol/L | 2.15 (1.58-2.91) | < 0.001 |
| Triglycerides: > 2.26 vs < | ||
| 2.26 mmol/L | 3.34 (2.50-4.46) | < 0.001 |
| CPR > 3 vs < 1 mg/L | 7.06 (4.51-11.02) | < 0.001 |
| CPR > 3 vs < 1 mg/L | 5.83 (3.07-11.06) | < 0.001 |
With regard to carotid atherosclerosis, a significant difference in mean values of intima-media thickness (0.89 + 0.26 vs 0.64 + 0.14 mm, P = .0001) and prevalence of plaques (26 [21%] vs 15 [6%], P < .001) was observed between nonalcoholic fatty liver disease patients and controls in a study performed by Francanzani et al16 in 375 patients (125 patients with NAFLD and 250 controls).
Steatosis was the strongest variable independently associated to intima-media thickness and to an increased risk of atherosclerosis in subjects with metabolic syndrome. It is important to mention that the strongest independent risk predictor of vascular damage was steatosis followed by age and systolic blood pressure.
It was recently shown that patients with NAFLD have endothelial dysfunction potentially responsible for cardiovascular disease in the long term17. Enhaced oxidative stress, inflammation with release of inflammatory cytokines, and abnormal lipoprotein metabolism could account for the proatherogenic effect of NAFLD; in addition to this, increased levels of ox-LDL in patients with higher intima media thickness. Visceral fat, even in normal weight or slightly overweight subjects with steatosis, could play a direct role in the development of atherosclerosis through multiple secreted factors.18
Also, a Turkish study by Cikim19 evaluated the relationship between hepatic steatosis, epicardial adipose tissue (EAT) and insulin resistance in obese patients. They found EAT was high in all groups, suggesting that hepatic steatosis should be assessed as a predictor that reflects the increments of whole body fat mass as well as abdominal adiposity.
The Study of Chavez-Tapia et al in Mexico City an-alized 1,421 subjects with NAFLD and MS. Among these patients a systolic blood pressure > 130 mmHg was associated with a positive treadmill test with an OR = 4.705 (95% CI 1.285-17.231). Interestingly, waist circumference an MS remained as risk factors related to positive treadmill tests (OR = 8.750, 95%CI 1.83041.843; and OR = 3.802, 95% CI 1.121-12.987, respec-tivetely). They concluded that subjects with NAFLD and high systolic blood preassure are at increased risk to develop CVD.20
ConclusionsToday’s lifestyle represents a huge challenge for health-care providers. Most meals are full of carbs, lipids and have high caloric contents; thus helping to increase the prevalence of MS and its consequences such as NAFLD and increased CVD-related mortality.
As mentioned above, NAFLD is associated to an increased risk to develop cardiovascular disease which augments as the hepatic damage progresses. The presence of NAFLD would predict a higher atherogenic risk regardless of the other components of the MS. It is proba-ble that NAFLD may not be a marker of CVD, but it may certainly be involved in its pathogenesis; more studies are needed to prove this hypothesis. Patients with NAFLD regardless of their liver function tests should be considered at a higher risk to develop complications from CVD.
What we see today is yet the top of the iceberg of what could be one of the main diseases for the years to come since the incidence of both MS and NAFLD will increase. It is of serious importance to take an aggressive preventive measures in this group of patients.