Introduction: Nonalcoholic steatohepatitis (NASH) is common cause of chronic liver disease strongly associated with insulin resistance leading to fibrosis. No factors that determine increasing fibrosis have been well recognized. Liver biopsy is considered as gold standard for diagnosis and prognosis of this disease.
Aim: To identify independent predictive factors of liver fibrosis in patients of NASH with diabetes.
Material and methods: During the year 2001 and 2002 total 36 patients of NASH associated with diabetes were included in the study. The diagnosis of NASH was based on 1) presence of steatosis, inflammation and ballooning on liver biopsy 2) Intake of alcohol < 20 gm of ethanol per week 3) Exclusion of other liver diseases. Patients were labeled as diabetic if random glucose was > 200 mg/dL or fasting glucose more than 140 mg/dL on 2 occasion or having documented use of oral hypoglycemic medications or insulin. Clinical and biochemical variables such as age, sex, obesity, hypercholesterolemia, AST, ALT and AST: ALT were examined for predictors of fibrosis using univariate and multiple regression statistical analysis. Obesity was defined as BMI > 30 for both males and females. Hypercholesterolemia was considered when fasting cholesterol level was above 95th percentile of normal on at least 2 occasions. Fibrosis was noted as present or absent on histology.
Results: Of 36 patients 17 were females and 19 males with age range of 25 to 75 years, mean age 50.8 years. Fibrosis was present in 11 (30.5%) and absent in 25 (69.4%) patients. Univariate and multiple correlations co-efficient failed to detect significant association of fibrosis with above mentioned variables. However multiple regression and logistic regression analysis (MLR) detected statistical significance for AST, ALT levels and AST: ALT ratio between fibrosis and no fibrosis in 80.6% patients.
Conclusion: There is no definite noninvasive test that helps to predict liver fibrosis however AST, ALT levels and AST: ALT ratio may help to determine the fibrosis in patients of NASH with diabetes in majority of cases.
Nonalcoholic steatohepatitis (NASH) is recognized increasingly as one of the cause of chronic liver disease.1 It is characterized by elevated liver enzymes with findings of steatohepatitis on histology.2 Sustained liver injury leads to progressive fibrosis and development of cirrhosis.3 It may be cause of cryptogenic liver cirrhosis.4,5 Various risk factors have been suggested such as obesity, type 2 diabetes mellitus, hypercholesterolemia, drugs and toxins. Insulin resistance is an important factor associated with NASH.4 With urbanization and changes in life style, type 2 diabetes mellitus has become very common in India. The increase in incidence of diabetes is associated with obesity, insulin resistance, hepatic steatosis and NASH.5 About 30 to 60% patients of NASH have underlying diabetes mellitus.2 The histological spectrum of liver disease in cases of NASH with diabetes ranges from simple steatosis, steatohepatitis to development of fibrosis and cirrhosis. The patients showing progressive liver disease are commonly associated with these predisposing factors. Though various laboratory and noninvasive techniques are available such as Ultrasonography, CT scan and magnetic resonance imaging (MRI) there is no definite test that determines increasing fibrosis in such patients. In recently published report it was shown that patients of NASH with normal alanine aminotransferase (ALT) could have bridging fibrosis and cirrhosis. In this study diabetes was the only factor independently associated with fibrosis. 8 Hence the aim of this study was to find the predictive factors for fibrosis in patients of NASH with diabetes mellitus.
Material and methodsThirty-six biopsy proven cases of NASH who had associated diabetes mellitus presented during year 2001 and 2002 were included in the Patients were labeled as diabetic if random blood glucose was more than 200 mg/dL or fasting blood glucose more than 140 mg/ dL on two occasions or if patients were taking insulin or oral hypoglycemic medications for diabetes. The diagnosis of NASH was established in all patients based on following criteria: 1) Elevated liver enzymes 2) Liver biopsy showing macrovesicular steatosis (>10%) as well lobular and or portal inflammation and variable fibrosis 3) appropriate exclusion of other liver disease such as alcoholic liver disease, viral hepatitis, autoimmune hepatitis, drug induced liver disease, biliary disorders, hemochromatosis, Wilson’s disease and alpha 1 antitrypsin - associated liver disease. The alcohol intake in all patients was less than 20 gm per week. Clinical and biochemical variables were examined in all patients for the predictors of fibrosis using univariate and multivariate regression statistical analysis. Statistical test used for analysis was student’s unpaired t test. These were age, sex obesity, hypercholesterolemia, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and AST: ALT > 1. Obesity was defined as BMI (body mass index) > 30 for both males and females.
Hypercholesterolemia was considered when fasting cholesterol level was above 95th percentile of normal on at least 2 occasions. Fibrosis was noted as present or absent on histology.
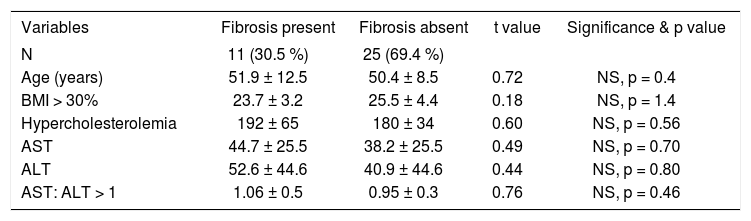
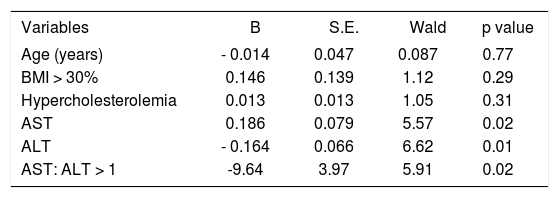
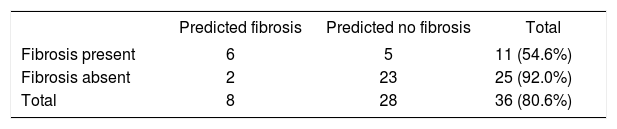
ResultsOut of 36 patients, 17 (47.2%) were females and 19 (52.7%) males with the mean age of 50.8 ± 7.4 yrs ranging from 25 to 75 years. Mean BMI was 24.9 ± 4.7 which was calculated as weight in kg/height in meters. BMI was 30 and above in 7 (19.4 %) patients. Mean cholesterol, AST and ALT levels were 183.4 ± 34.8 mg/dl, 40.2 ± 17.1 U/L and 44.4 ± 21.7U/L respectively. AST: ALT ratio ranged from 0.41 to 1.85 with mean of 0.98 ± 0.26. On liver biopsy all patients showed macrovesicular steatosis of different degree and parenchymal inflammation of varying severity. Fibrosis was present in 11 (30.5%) and absent in 25 (69.4%) cases. As the main objective was to identify parameters indicating fibrosis, statistical analysis was done for age, sex, obesity, and hypercholesterolemia, AST, ALT and AST: ALT ratio. Univariate analysis failed to detect significant association of fibrosis with above mentioned variables (Table I). Multiple correlation co-efficient also failed to detect significant difference between fibrosis and no fibrosis cases. However more powerful statistical technique multiple regression analysis and multiple logistic regression analysis (MLR), however detected statistical significance for AST, ALT levels and AST: ALT ratio between fibrosis and no fibrosis cases. (Table II) MLR could predict fibrosis in about 80.6% giving sensitivity of 55% and specificity of 92% with the help of all the variables included in the study (Table III).
Univariate analysis to show fibrosis amongst variables.
| Variables | Fibrosis present | Fibrosis absent | t value | Significance & p value |
|---|---|---|---|---|
| N | 11 (30.5 %) | 25 (69.4 %) | ||
| Age (years) | 51.9 ± 12.5 | 50.4 ± 8.5 | 0.72 | NS, p = 0.4 |
| BMI > 30% | 23.7 ± 3.2 | 25.5 ± 4.4 | 0.18 | NS, p = 1.4 |
| Hypercholesterolemia | 192 ± 65 | 180 ± 34 | 0.60 | NS, p = 0.56 |
| AST | 44.7 ± 25.5 | 38.2 ± 25.5 | 0.49 | NS, p = 0.70 |
| ALT | 52.6 ± 44.6 | 40.9 ± 44.6 | 0.44 | NS, p = 0.80 |
| AST: ALT > 1 | 1.06 ± 0.5 | 0.95 ± 0.3 | 0.76 | NS, p = 0.46 |
Statistical test: student’s unpaired t test
p = 0.05 was taken as significance level.
NS = Not significant.
Multiple logistic regression analysis for fibrosis.
| Variables | B | S.E. | Wald | p value |
|---|---|---|---|---|
| Age (years) | - 0.014 | 0.047 | 0.087 | 0.77 |
| BMI > 30% | 0.146 | 0.139 | 1.12 | 0.29 |
| Hypercholesterolemia | 0.013 | 0.013 | 1.05 | 0.31 |
| AST | 0.186 | 0.079 | 5.57 | 0.02 |
| ALT | - 0.164 | 0.066 | 6.62 | 0.01 |
| AST: ALT > 1 | -9.64 | 3.97 | 5.91 | 0.02 |
Statistical significance: Student’s unpaired t test
p = 0.05 was taken as significance test
NASH is the hepatic manifestation of insulin resistance. It is often the first clinical indication of type 2 diabetes mellitus.7 The incidence of diabetes mellitus in patients of NASH varies from 21 to 75%.2 This in contrast with another report from India where they have concluded that diabetes, obesity and hyperlipidemia are not common findings with NASH.9 Editorial comments on this article suggested that the country with growing incidence of diabetes mellitus is expected to have, diabetes as an important risk factor for non-alcoholic fatty liver disease.10
Normally insulin promotes glycogen synthesis and inhibits gluconeogenesis as well as mitochondrial fatty acid oxidation. Insulin resistance is associated with increased lipid oxidation and decreased carbohydrate oxidation leading to an oxidative stress followed by accumulation of fat in the hepatocytes.1 Most of the patients with simple steatosis follow an indolent clinical course, where as those with steatohepatitis with or without fibrosis or cirrhosis are most likely to develop clinically significant complications of liver disease.11,12 Age, sex, hypercholesterolemia and obesity are considered to be risk factors for fibrosis in patients of NASH.13-16 However diabetes mellitus is independent risk factor for NASH having similar predisposing conditions.17,18 A number of studies have shown clinical predictors of fibrosis in cases of NASH but the same has not been studied well in cases of NASH associated with diabetes mellitus.1,6,10,16 Out of 36 patients of NASH with diabetes, fibrosis was present on histology in 11 (30.5%) and absent in 25 (69.4%) cases. Age, sex, BMI, hypercholesterolemia, AST, ALT and AST: ALT ratio was the variables compared between the patients with or without fibrosis. Mean age of our patients was 50.8 years. The role of female gender has been more variable in reported series with some showing aggressive course.14 It is also suspected that there is an even distribution of NASH among men and women although there may be gender variation among the specific classes. 6 We have not found significant difference between females and males with respect to fibrosis. Obesity and hypercholesterolemia are two factors associated with both NASH and diabetes mellitus. It has been shown in the several studies that both these are the risk factors in the progression of the disease.15,16 However these two variables were not significantly correlated with fibrosis in our patients.
Other reported predictors of fibrosis in cases of NASH are raised liver enzymes and ratio of AST: ALT greater than one.19-21 However liver enzymes are insensitive and cannot be used reliably to confirm the diagnosis or stage the extent of fibrosis. Significant liver disease can exist with liver enzymes in normal range.22 Angulo P et al12 have shown by multivariate analysis that older age, obesity, diabetes and AST: ALT ratio > 1 were significant predictors of sever liver fibrosis in patients of NASH. Shimada M et al23 have studied 81 patients of NASH and shown that low platelet count and high AST: ALT ratio and presence of mallory bodies were predictors of sever liver fibrosis. In our 36 cases though sample size was small, univariate and multiple correlation co-efficiant analysis did not show significant association of fibrosis with elevation in AST, ALT, and AST: ALT > 1. Only more powerful statistical method, multiple regression and logistic regression analysis (MLR) have detected statistical significance for AST ALT elevation and AST: ALT ratio between fibrosis and no fibrosis cases.
In conclusion though various risk factors are common for NASH as well as diabetes there is no accurate noninvasive method available that can determine risk of fibrosis in patients of NASH with diabetes. The elevated levels of transaminases are non-specific and may not indicate progression of the disease. Hence still today liver biopsy remains gold standard in staging and predicting progression in patient with NASH.
Acknowledgement: We are thankful to Mr Anil S Arekar for carrying out statistical analysis for this study.