Hepatic cysts encompass a spectrum of clinical etiologies but most are benign, occur rarely, and are usually asymptomatic. Symptomatic cysts may present with abdominal pain, hemorrhage, obstructive jaundice, or a consumptive coagulopathy. The optimal surgical management of hepatic cysts varies depending on the size and location of the lesion, but includes laparoscopic cyst fenestration,1 formal resection, enucleation, as well as liver transplantation.
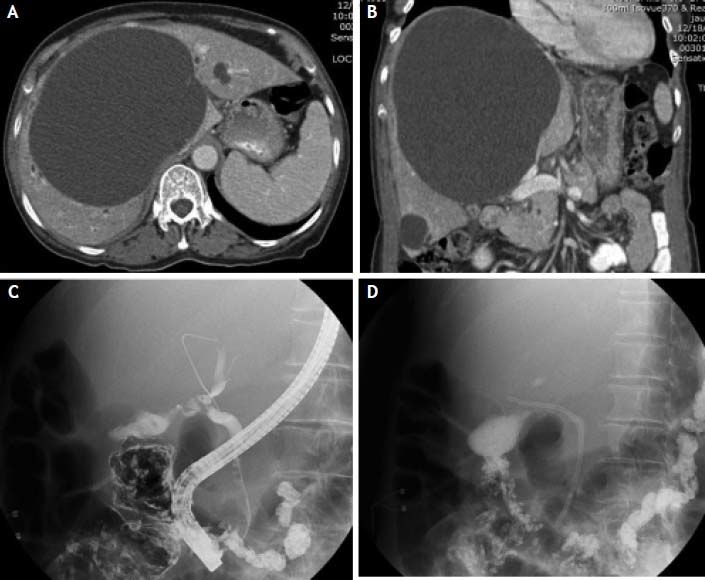
Case ReportA 79-year old Asian woman presented to her naturopathic doctor with a two week history of abdominal pain, jaundice, pruritus, and darkened urine. Her past medical history was significant for known hepatic cysts, noted ten years prior during an echocardiogram. The patient was referred to the emergency department for further evaluation. On physical examination, she was jaundiced, and her abdomen was soft and non-tender with right upper quadrant fullness. Initial laboratory values were notable for an elevated aspartate aminotransferase (AST; U/L) of 1,109, alanine aminotransferase (ALT; U/L) of 1938, alkaline phosphatase (ALP) of 455 U/L, INR of 1.7, and conjugated hyperbilirubinemia of 21 mg/dL. In addition, her hematocrit was noted to be 7 points lower than the previous year’s laboratory results. Liver function tests from the prior decade had been within the normal range, with the exception of a mildly increased ALP level within the 6 months prior to presentation. Other than being immune to hepatitis B, her hepatitis serologies were negative. A computed tomography (CT) scan of the abdomen was significant for a central hypoechoic hepatic cyst measuring 16 × 15 × 16 cm with rare septations (Figures 1A and 1B). The patient underwent an ERCP the following day, with stenting of the obstructed right biliary duct (Figures 1C and 1D). Although her transaminitis improved, her hyperbilirubinemia persisted prompting referral to our institution. Upon arrival, the patient was started on albendazole given the possible echinococcal etiology of the cyst.
A. Initial axial abdominal CT showing a dominant, central hepatic cyst measuring 16 × 15 × 16 cm. B. Initial coronal abdominal CT demonstrating extrinsic hilar compression. C. ERCP demonstrating right hepatic ductal obstruction secondary to extrinsic compression from a large hepatic cyst. D. Subsequent ERCP image following successful placement of right biliary duct Stent.
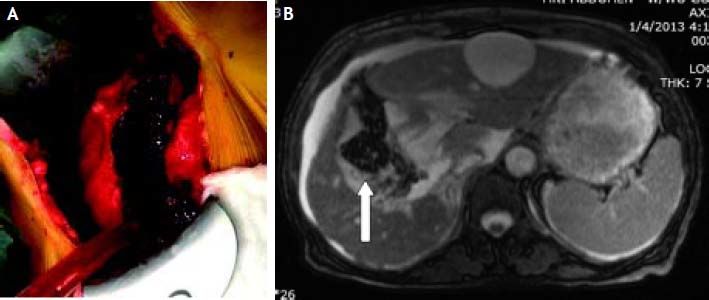
The patient was taken to the operating room and a 6 cm Kocher incision was made overlying the dominant hepatic cyst. Smaller simple cysts were noted throughout the liver. The area surrounding the central hepatic cyst was packed off with hypertonic saline soaked laparotomy pads. The anterior wall of the cyst was unroofed and sent to pathology, and approximately 1,500 cc of brown fluid was evacuated with samples sent for culture (Figure 2A). Hypertonic saline solution was irrigated within the cavity, and allowed to dwell given the concern for echinococcal disease. A cholecystectomy was performed, followed by an omental pedicle placement within the cyst cavity (Figure 2B). Final microbiology showed abundant red blood cells and no parasites or bacteria. Final pathology showed no evidence of malignancy, and was consistent with a hemorrhagic cystic lesion. Prior to discharge home on post-operative day six, the patient underwent repeat ERCP with stent removal. A MRCP was performed two weeks post-operatively and showed patent vasculature and no significant biliary duct dilation. Two months after the operation, her liver function tests had normalized.
DiscussionHepatic cysts may be classified as simple benign non-parasitic cysts, parasitic cysts, or neoplastic cysts.2 A study by Caremani, et al. has estimated the incidence of liver cysts in the general population to be between 1-5%.3 A review by Ishiwika, et al. reported only 19 cases of solitary cysts causing obstructive jaundice. Characteristically, these cysts are large lesions (> 10 cm), predominantly located in segments four and five, and cause intrahepatic biliary duct dilatation with associated elevations in total bilirubin levels.4–6
With regards to management, asymptomatic benign non-parasitic liver cysts do not require surgery.7 For symptomatic benign liver cysts requiring intervention, laparoscopic fenestration has been favored. Martin, et al. noted that laparoscopic deroofing had reduced morbidity (25 vs. 36%) and hospital stays (3 vs. 8 days), compared to open deroofing.1 Due to high recurrence rates, needle aspiration and percutaneous drainage are no longer favored. In selected cases, liver resection and possibly even liver transplantation may be required.
Our patient presented with a dominant central hepatic cyst causing obstructive jaundice. Given the large size of the lesion and the concern for possible echinococcal etiology, an open cyst fenestration was performed. The degree of elevated transaminitis on presentation suggests hepatocellular insult that could have been associated with a component of vascular obstruction caused by the cyst, as well as cholangitis from biliary obstruction. Obstructive jaundice from a liver cyst is rare and appropriate pre-operative laboratory and imaging workup is necessary prior to deciding on surgical management. When choosing surgical approach, the size, location, and potential etiologies of the lesion must be considered carefully.