Abstracts of the 2024 Annual Meeting of the ALEH
Más datosNo
Introduction and ObjectivesIdentifying risk factors for poor outcomes is crucial for defining treatment strategies and allocating resources in COVID-19. The Fibrose-4 score (FIB-4) and D-dimer (DD) have emerged as prognostic markers; however, precise cutoff points and their combined use remain unstudied. Objectives: This study aimed to compare the individual and combined performance of FIB-4 and DD in predicting outcomes among COVID-19 patients.
Patients / Materials and MethodsMaterials and Methods: From March to December/2020, hospitalized COVID-19 patients were evaluated regarding laboratory admission tests, chest CT scan, gender, age, lung involvement, ICU admission, hemodialysis, mechanical ventilation, and mortality. Optimal FIB-4 and DD cutoffs to predict in-hospital mortality, aiming to maximize sensitivity and specificity, were established. A sequential diagnostic strategy using both markers was subsequently evaluated.
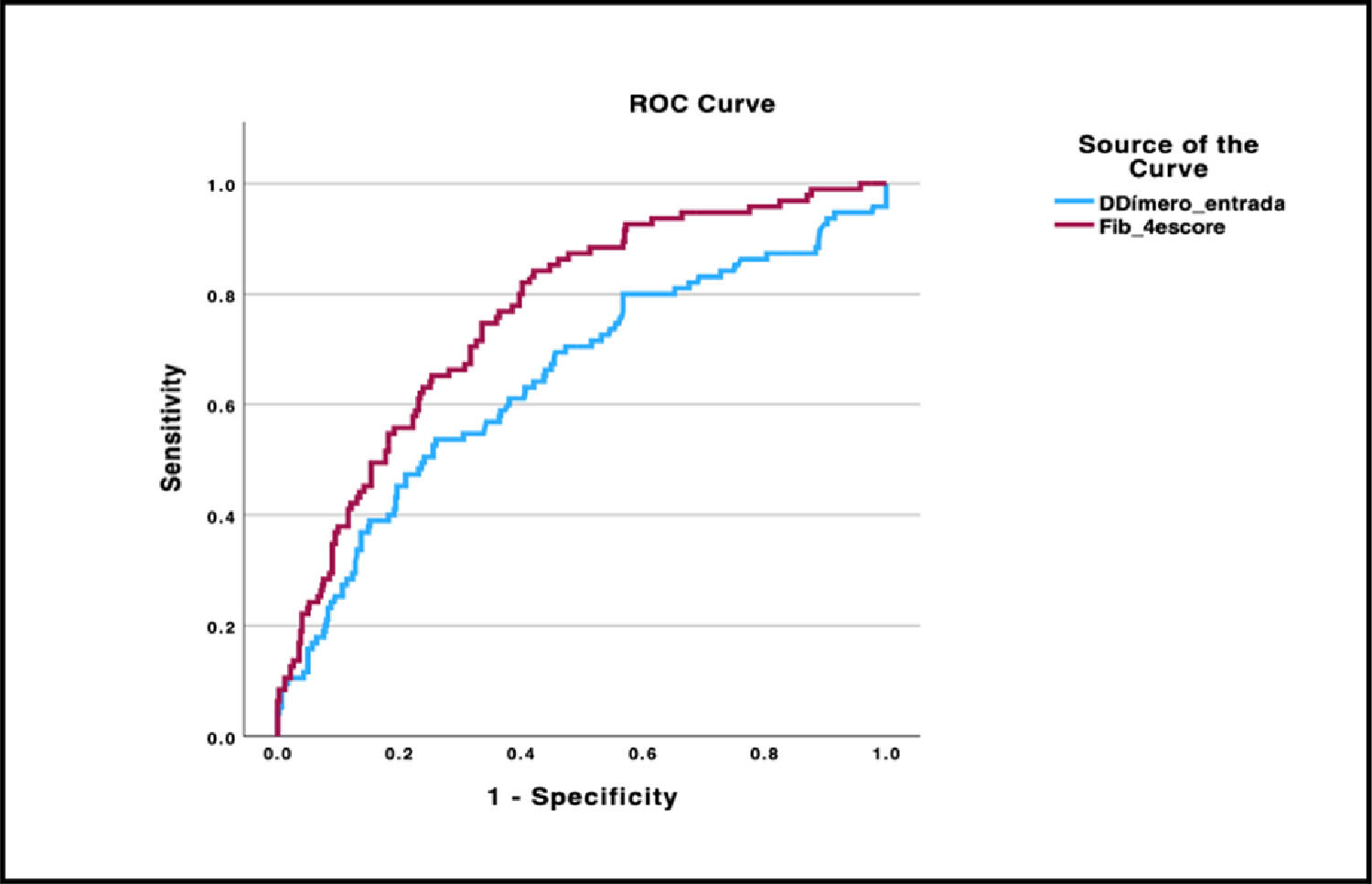
Results and DiscussionResults and Discussion: Among 518 patients (61±16 years, 64% men), the in-hospital mortality rate was 18%. FIB-4 showed superior performance in predicting mortality compared to DD (AUROC 0.76 vs. 0.65, p=0.003) and was chosen as the first step in sequential analysis. Mortality was higher in patients with FIB-4≥1.76 vs. FIB-4<1.76 (26% vs. 5%, p<0.001) and DD≥2000 ng/mL FEU vs. DD<2000 ng/mL FEU (38% vs. 16%, p<0.001). FIB-4 was used as a screening test, with a cutoff point of 1.76 (90% sensitivity in ROC curve analysis), followed by DD measurement with a cutoff value of 2000 ng/mL FEU (specificity of 90%). Through this approach, a subgroup of patients with a higher mortality rate was identified, compared to the use of FIB-4 alone (48% vs. 26%, p<0.001), missing the identification of only 4.7% of deaths.
ConclusionsThe sequential use of FIB-4 and DD represents a comprehensive strategy to identify high-risk COVID-19 patients at hospital admission, potentially minimizing unnecessary DD assessments in patients initially classified by FIB-4 as low-risk for adverse outcomes.
Analyze of the performance of FIB-4 and DD in predicting in-hospital mortality through ROC curve analysis
Comparison of primary and secondary outcomes of patients with low and high FIB-4
Comparison of primary and secondary outcomes of patients with low and high DD
Hospital mortality rates according to FIB-4 and DD levels