Abstracts of the 2021 Annual meeting of the ALEH (Asociación Latinoamericana para el Estudio del Hígado)
Más datosAcute decompensation (AD) of cirrhosis is associated with systemic inflammation and increased circulating cytokines. The use of inflammatory markers, such as calprotectin, could provide information on the role of the immune response in the prognosis of cirrhosis.
AimsTo evaluate serum calprotectin levels in patients hospitalized complications of cirrhosis.
MethodsThis prospective cohort study included 200 adult subjects hospitalized for complications of cirrhosis who were followed for up to 30 days after admission. Twenty healthy subjects and 20 patients with stable cirrhosis were evaluated as controls. Serum calprotectin was measured by the ELISA.
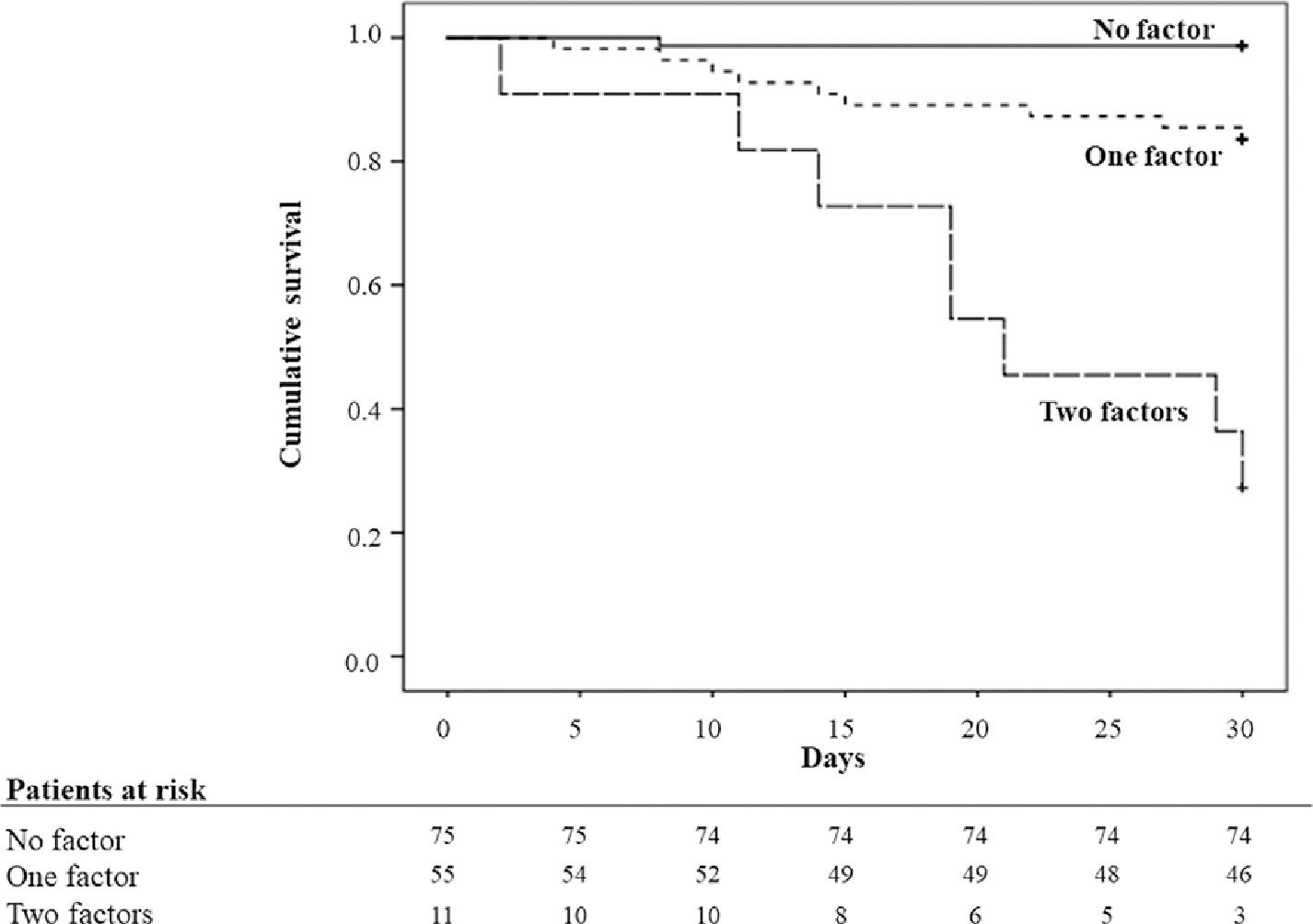
ResultsSerum calprotectin levels were higher among the two groups of cirrhosis patients when compared to healthy controls. Greater median values of calprotectin were observed among patients with Child-Pugh C, ACLF, infection, ascites and hepatic encephalopathy. Concentrations of calprotectin were not related to the presence of ACLF, infection or to 30-days survival. However, when considered only patients with AD without ACLF (n = 144), higher values of calprotectin and CLIF-C ADs were associated with the lower survival in the univariate and multivariate Cox analyzes. The Kaplan-Meier survival probability was 98.7% in subjects with none of the factors (CLIF-C ADs <60 and calprotectin < 580 ng/mL), 83.6% in subjects with one of the factor (CLIF-C ADs ≥ 60 and calprotectin < 580 ng/mL or CLIF-C ADs < 60 and calprotectin ≥ 580 ng/mL) and 27.3% in subjects with both factors (CLIF-C ADs ≥ 60 and calprotectin ≥ 580 ng/mL), in which p = 0.002 between the first and second groups, and p < 0.001 between the first and third, and between the second and third groups (Figure).
ConclusionsThe combination of the serum calprotectin and CLIF-C ADs may be useful in clinical practice to identifying patients with acute decompensation of cirrhosis and a very low 30-day survival rate.