Abstracts of the 2024 Annual Meeting of the ALEH
Más datosNo
Introduction and ObjectivesTen-year survival after liver transplantation (LT) in PBC is around 80%; disease recurrence (DR) occurs in 17-46%, with patient and graft survival impact. OBJECTIVES: To evaluate the epidemiological profile of patients transplanted due to PBC and recurrence risk factors.
Patients / Materials and MethodsRetrospective cohort analysis from 1997 to 2022. Until 2002, standard immunosuppression (IS) was with cyclosporine (CYA); later tacrolimus (TAC). From 2019, preemptive ursodeoxycholic acid (UDCA) was started in the first 3 months of LT to prevent DR (46.2%).
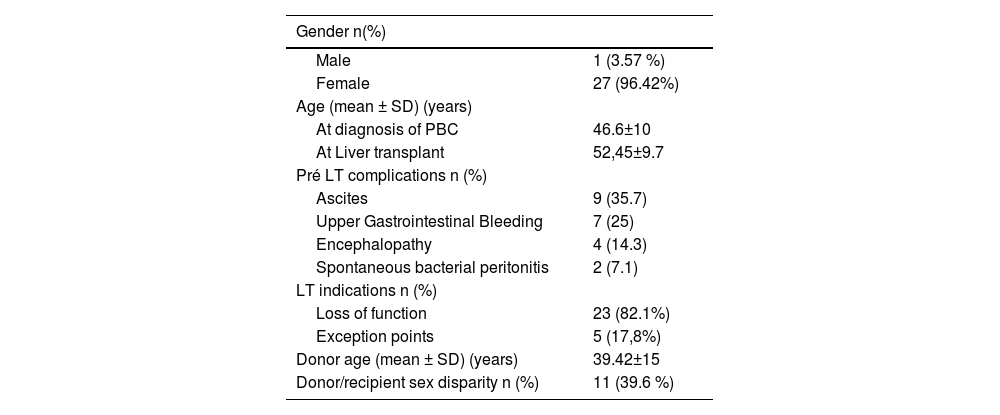
Results and Discussion28 patients were evaluated, 96.4% female with 52.4±9.7years at LT (2 living donor). The pre-LT data are shown in Table 1. Five patients were transplanted due to exception points (3 pruritus, 1 refractory ascites, 1 encephalopathy). After LT, 11 presented acute cellular rejection (ACR) (2 cases during the switch of TAC to CYA to prevent DR) and 4 CMV infection (14.3%). The DR rate was 46.4% in 6.34±5.5 years post-LT, most of them stage I. At relapse, 53.9% were using CYA. Four patients (14.3%) died. The preemptive use of UDCA was associated with a lower risk of recurrence (25 × 71.4%, p=0.047). There was no impact of recurrence on patient survival.
ConclusionsIn literature CYA is associated with a lower risk of DR and greater survival, however, in our cohort, > 50% were using the medication at relapse. Some cases of ACR occurred at the shift of TAC to CYA. It's important to discuss the ideal time to IS conversion, particularly during the first 6 months and to use preemptive UDCA to reduce DR. Although almost 50% of patients relapsed, deaths were not related to recurrence. The preemptive use of UDCA post-LT appears to be associated with lower DR, with no impact on survival, probably due to the short follow-up period.
Table 1: Pre-LT data
| Gender n(%) | |
|---|---|
| Male | 1 (3.57 %) |
| Female | 27 (96.42%) |
| Age (mean ± SD) (years) | |
| At diagnosis of PBC | 46.6±10 |
| At Liver transplant | 52,45±9.7 |
| Pré LT complications n (%) | |
| Ascites | 9 (35.7) |
| Upper Gastrointestinal Bleeding | 7 (25) |
| Encephalopathy | 4 (14.3) |
| Spontaneous bacterial peritonitis | 2 (7.1) |
| LT indications n (%) | |
| Loss of function | 23 (82.1%) |
| Exception points | 5 (17,8%) |
| Donor age (mean ± SD) (years) | 39.42±15 |
| Donor/recipient sex disparity n (%) | 11 (39.6 %) |
Table 2: Post-LT data
| Preemptive UDCA n (%) | 12 (46.2) |
| Acute cellular rejection n (%) | 11 (39.3) |
| Exchange of TAC for CYA | 2 (7.1) |
| Cytomegalovirus | 4 (14.3) |
| PBC recurrence n (%) | 13 (46.4) |
| Use of CYA | 7/13 (5.9) |
| Deaths n (%) | 4 (14.3) |
| Early complications | 2 (7.14) |
| HBV de novo | 1 (3.5) |
| Pancreatic neoplasm | 1 (3.5) |
| 10-year survival | 85% |