Abstracts of the 2024 Annual Meeting of the ALEH
Más datosNo
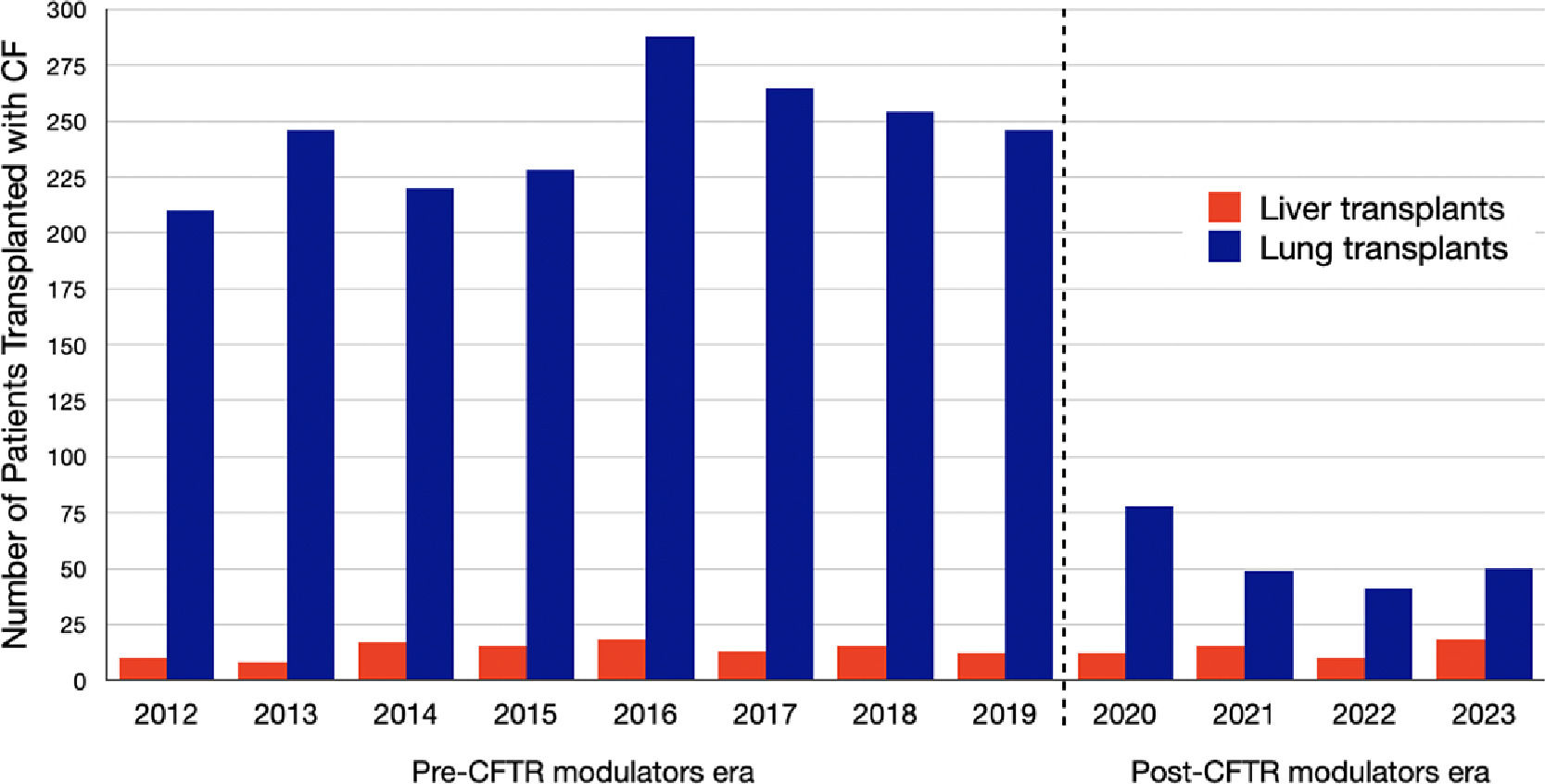
Introduction and ObjectivesThe impact of cystic fibrosis (CF) transmembrane conductance regulator (CFTR) modulators on the natural history of liver disease is unknown. The objective of this study is to assess changes in the rates of liver transplantation compared to lung transplantation since the approval of the new CFTR modulators in October 2019.
Patients / Materials and MethodsPatients with CF (PwCF) who were listed for liver or lung transplantation were identified in the OPTN/UNOS database. We compared outcomes between the pre- and post-CFTR modulators eras, 2012-2019 and 2020-2022, respectively.
Results and DiscussionBetween 2012-2023, 95,254 liver and 28,715 lung transplants were performed, including 138 (0.09%) and 2,129 (7.4%) transplants in PwCF, respectively. The rate of death on the waitlist was not significantly different between eras in either group. For liver transplantation, the median percentage of CF-related listings per year was similar between the two eras 0.13% (0.11-0.17%) in 2012-2019 vs. 0.12% (0.11-0.13%, p=0.18) in 2020-2023. Similarly, the median percentage of CF-related liver transplants per year was 0.14% (0.12-0.20%) vs. 0.14% (0.11-0.16%, p=0.450) (see figure). For lung transplantation waitlist additions per year decreased from 7.58% (6.72-8.17%) to 1.11% (0.95-1.52%) per year from the pre- to the post-modulator era (p<0.001). The median percentage of CF-related transplants per year was 11.18% (10.42-11.94%) in pre-modulator era vs 1.64% (1.56-2.23%) in the post-modulator era (p<0.001).
ConclusionsWe describe stable liver transplant activity for PwCF in the post-modulator era compared to the pre-modulator era, while the need for lung transplantation declined after the introduction of highly-active CFTR modulators. Long-term data is required to determine the role of CFTR modulators on modifying the need of liver transplantation in PwCF.