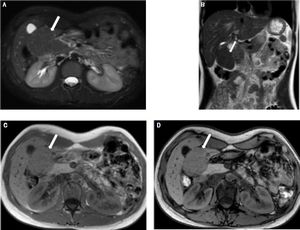
A 25 year old healthy female presented with a two month history of nausea, epigastric pain that worsened after eating and diarrhea. Complete blood count and biochemistry panel results were unremarkable and liver serology was negative. Abdominal ultrasonography (US) showed a solid lesion in the right upper quadrant, suspicious for a gastric mass. Liver protocol multiphase computed tomography (CT) followed, which showed an eccentric lesion attached to hepatic segment 2, measuring 4.8 cm at its widest dimension. The lesion demonstrated peripheral nodular enhancement and a central focal hypodensity. Several days later, dedicated liver magnetic resonance imaging (MRI) was performed. At MRI, the lesion was hypointense on T2-weighted images and showed no signal dropout on opposed-phase T1-weighted gradient-recalled echo (GRE) images (Figure 1). The central vascular scar was clearly visible on Gadolinium-enhanced T1-weighted images and showed enhancement during the venous phase (Figure 2). After the injection of a hepatocyte-specific agent (gadobenate dimeglumine, Gd-BOPTA; Multi-Hance®, Bracco Imaging, Brescia, Italy), the lesion appeared to be hyperintense to adjacent liver parenchyma during the hepatobiliary phase at 40 min (Figure 3). All said features are compatible with the diagnosis of FNH. Of note, the lesion shifted position between the dynamic MR scan and the hepatobiliary scan: It is seen under the right hepatic lobe on the dynamic scan (Figures 1-3). The patient was then allowed to stretch before commencing with the hepatobiliary phase scan, where the lesion is seen to the left of the midline. The pedicle is clearly visible, too (thin arrows on figure 3). Based on these imaging findings, the diagnosis of pedunculated FNH was made.
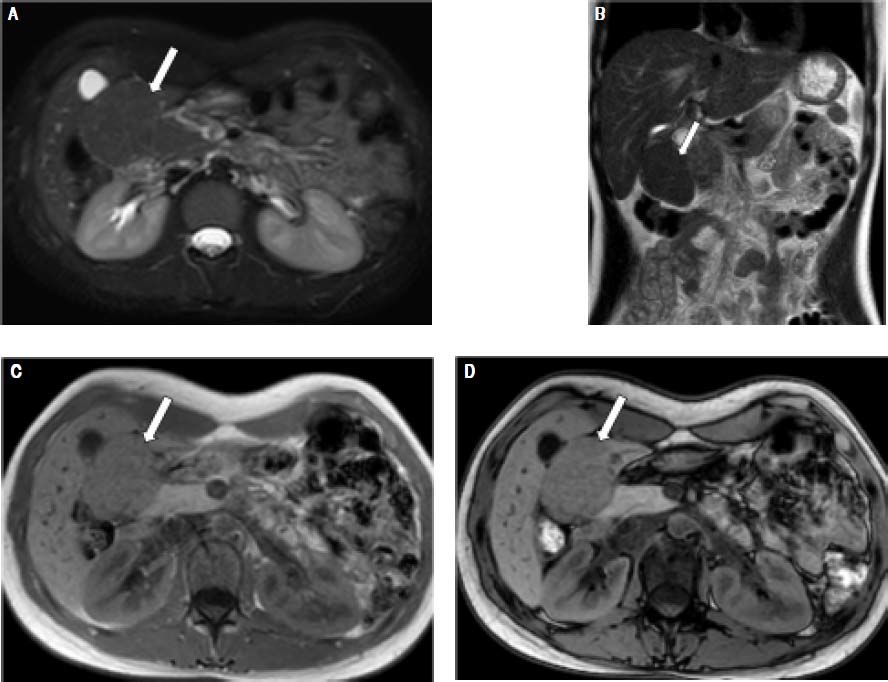
A 25-year-old female with focal nodular hyperplasia (FNH). Axial (A) T2-weighted MR image (with fat suppression) and coronal (B) T2-weighted MR image (without fat suppression) show an exophytic isointense right sub-hepatic mass (arrow) compressing the galbladder. Axial in-phase (C) and opposed-phase (D) T1-weighted GRE images show no fat component in the lesion.
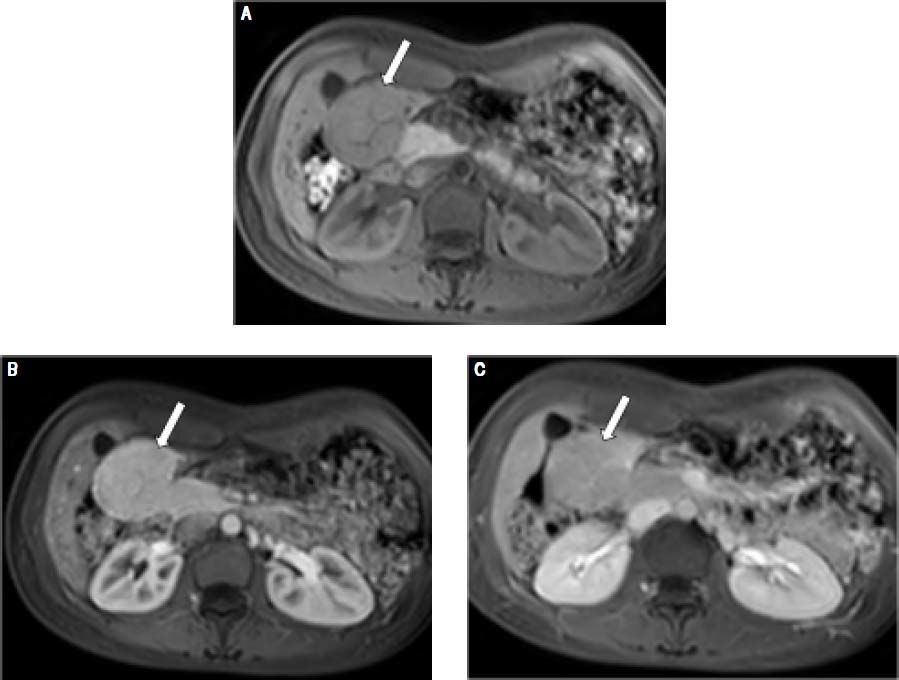
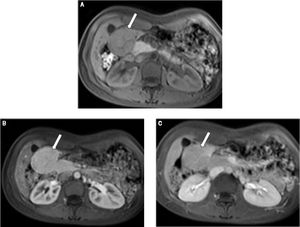
A 25-year-old female with focal nodular hyperplasia (FNH). Axial T1-weighted images prior to gadolinium injection (A) and after injection, at the arterial phase (B) and venous phase (C) show an exophytic right sub-hepatic hypervasular lesion (arrow). The mass shows homogeneous enhancement during the arterial phase and is slightly hyperintense on the portal venous phase image. Central scar is clearly visible and enhances at the venous phase. These features are compatible with diagnosis of FNH.
A 25 year old female with a known pedunculated focal nodular hyperplasia (FNH) underwent gadobenate dimeglumine (Gd-BOPTA; IMultilHance) enhanced IMR examination. Coronal T1-weighted images at the venous phase (A) and during the hepatobiliary phase (B and C). The mass is slightly hypointense on the portal venous phase image and is definitely hyperintense to adjacent liver parenchyma during the hepatobiliary phase at 40 min. Note that the lesion shifted position between the dynamic MR scan and the hepatobiliary scan: It is seen under the right hepatic lobe on the dynamic scan (A) and to the left of the midline on the hepatobiliary scan (B and C). The pedicle is clearly visible (thin arrows). These imaging findings are compatible with the diagnosis of pedunculated FNH.
Focal nodular hyperplasia (FNH) of the liver is a focus of regenerative (i.e., non-neoplastic) hepatic tissue that develops around anomalous arteries.1 It is the second most common benign hepatic tumor after hemangioma.2 Most affected individuals are women of childbearing age.3–5 Pedunculated FNH, however, is a rare entity. So rare, in fact, that an extensive search of the medical literature yielded a mere handful of case reports. The lesion is located in the extrahepatic region and connected to the liver by a thin stalk. This imaging finding is essential for the correct diagnosis. Hepatocyte-specific agent-enhanced delayed T1-weighted GRE affords a confident diagnosis of FNH. Most importantly, it allows distinguishing between FNH and hepatocellular adenoma (HCA),6,7 the other likely hepatic lesion in women of childbearing age, which can be pedunculated as well.8 Unequivocal diagnosis at MRI obviates the need for lesion biopsy, which carries a considerable risk of hemorrhage in the case of HCA.9,10
FNH is usually asymptomatic, wherefore it is often found incidentally on imaging. As it carries no malignant potential, management is conservative, namely, with clinical and imaging follow-up. Possible symptomatic complications of exophytic FNH include compression of surrounding vessels, gastric outlet obstruction and an increased risk of trauma-related hemorrhage. In the case of pedunculated FNH, pedicle torsion should also be taken into consideration. Torsion may in turn lead to infarction. Treatment is reserved only for symptomatic cases and consists of either surgical resection or embolization of the feeding vessel.
DisclosureNone.