Introduction. The use of prognostic models for cirrhotic patients admitted to the medical intensive care unit (ICU) is of great importance, since they provide an objective evaluation for a group of patients with high mortality rates and high resource utilization.
Objective. To evaluate the validity and to compare the prognostic predictive value of the CTP, MELD, SOFA and APACHE II scoring systems in cirrhotic patients admitted to the ICU, the CTP and MELD models being exclusive for patients with liver disease.
Material and methods. Commonly used predictors of mortality such as age, sex, CTP, MELD, APACHE II and SOFA were evaluated, and their prognostic value was investigated.
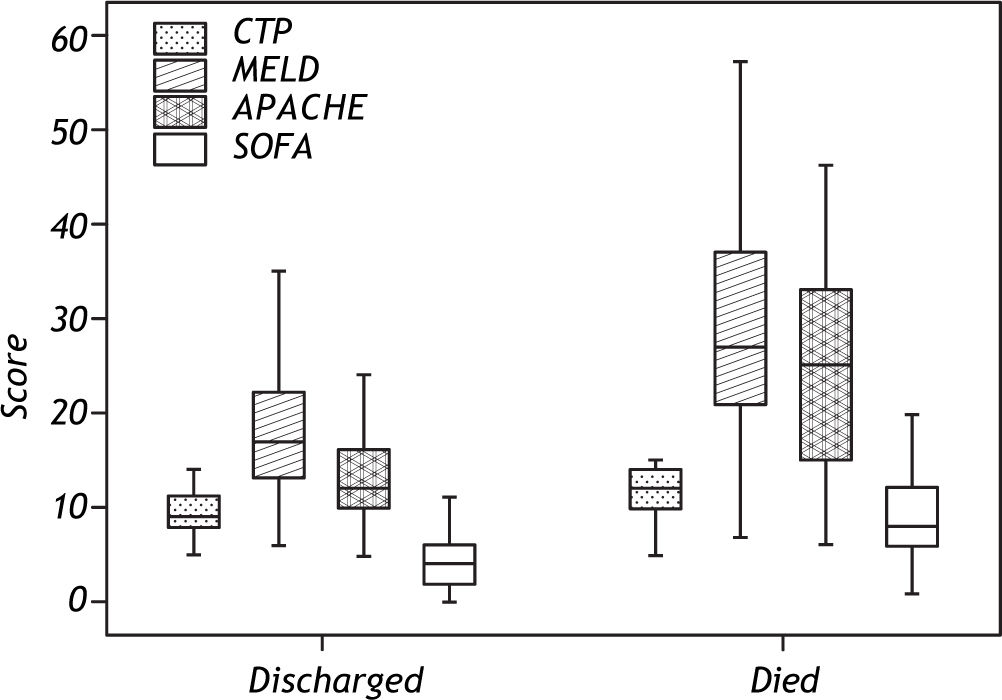
Results. A total of 201 patients were included in this study. Patients who survived had mean CTP score of 9.5 ± 2.4, MELD score 18.1 ± 7.1, APACHE II score of 13.4 ± 4.8 and SOFA score of 4.2 ± 2.6, compared to respective scores of 11.4 ± 2.8, 28.0 ± 11.2, 24.6 ± 10.4 and 8.7 ± 4.0 in patients who died. The difference between groups was statistically significant for each of one of the scoring systems (p < 0.001).
Conclusion. In this study, SOFA was found to be the most powerful predictor of prognosis for cirrhotic patients admitted to the ICU. This was followed by APACHE II, MELD and CTP models, in descending order of strength (AUROC values of 0.847, 0.821, 0.790 and 0.724, respectively).
The use of prognostic models for patients admitted to the intensive care unit (ICU) is of great importance, since they provide an objective evaluation for a group of patients with potentially high mortality rates and cost. The advanced stage of liver failure and the presence of cirrhotic complications contribute to the poor prognosis of cirrhotic pa-tients admitted to the ICU. Mortality rates are also affected by the severity of liver disease and concurrent dysfunction of other organ systems.
Many prognostic models have been developed to determine prognoses of hospitalized patients and thus help intelligently guide management. Of the models in use, the CTP and MELD scores have been designed exclusively for patients with liver disease, while the APACHE II and SOFA scores are valid for use in different patient groups admitted to the ICU.1
AimThe aim of this study was to determine the best prognostic model for cirrhotic patients admitted to the ICU by comparing the four most relevant models; Child-Pugh, MELD, APACHE II and SOFA.
Material and MethodsThis prospective study was undertaken in the Medical Intensive Care Unit of the Faculty of Medicine at Çukurova University between January 2007 and January 2010, and included cirrhotic patients who were admitted during the study period. In all of the patients enrolled a diagnosis of cirrhosis was confirmed either histologically or by resorting to clinical and laboratory findings.
Etiology of cirrhosis, presence of cirrhotic complications (esophagus variceal bleeding, hepatic encephalopathy, spontaneous bacterial peritonitis, and hepatorenal syndrome) and duration of ICU stay were recorded for each patient.
CTP, MELD, APACHE II and SOFA scores, as well as the Glasgow coma scale, were calculated for all patients taking into consideration the worst value for each parameter within the first 24 h after admission to the ICU. The MELD score was obtained using the UNOS formula, where bilirubin and creatinine (Cr) values of < 1 were still input as 1. The maximal Cr value was set as 4, even for patients on dialysis.2
The statistical prognostic values of patients’ age and sex, as well as SOFA, APACHE II, MELD and CTP scores were compared.
The area under the Receiver Operating Characteristic curve (AUROC) was calculated for each of the prognostic models, which was used to determine the model with the most significant prognostic power.
Statistical analysisData analysis was performed using Statistical Package for social sciences (SPSS) version 15. Comparison of non-continuous variables between groups was done using the Chi-square test, while continuous variables were compared using the Mann-Whitney U test was used for comparison continuous variables, followed by ROC analysis. Bonferroni correction was applied in cases of multiple testing and p-value of < 0.017 (0.05/3) was considered statistically significant.
ResultsA total of 201 patients with a mean age of 56.8 ± 14.1 were enrolled in the study, 130 (64.7%) of which were male. The mean age of patients who were discharged was 56.7 ± 14.7, compared to a mean age of 57.1 ± 13.3 in patients who died. There was no difference between patients who were discharged and those who died with regard to age or sex (p > 0.05).
The causes of cirrhosis in decreasing order of frequency were HBV (35.8%), cryptogenic (22.2%), HCV (18.2%) and alcohol (11.1%). No link was established between etiology of cirrhosis and prognosis (p > 0.05).
Hepatic encephalopathy and esophageal bleeding were the most commonly encountered cirrhotic complications at 60.2 and 46.8%, respectively. These were followed by HRS at 11.4% and hepatoma at 8%. The most frequently encountered infections were urinary tract infections (26.1%), SBP (14.1%), lung infections (12.6%) and sepsis (6%). Of all the patients followed in the ICU, 11.4% required mechanical ventilation, and overall mortality was 41.8%.
The presence of HE, HRS, sepsis and respiratory failure requiring mechanical ventilation were each independently found to be associated with poor prognosis (p < 0.005). A similar correlation could not be established in association with the presence esopha-geal variceal bleeding (EVB), hepatoma or an infection (p > 0.05). All patients who developed HRS during the study period died (Table 1). The mean duration of ICU stay for all patients, as well as mean CTP, MELD, APACHE II and SOFA scores have been summarized in table 2.
Comparison of complication rates in patients who died or were discharged from the intensive care unit (Chi-square test is used).
| Complication | Discharged | Died | p-value | All patients |
|---|---|---|---|---|
| (n = 117) | (n = 84) | (n = 201) | ||
| • Hepatoma | ||||
| Present | 6 | 10 | 0.111 | 16 (8%) |
| Absent | 110 | 73 | 183 (92%) | |
| • HE | ||||
| Present | 57 | 63 | <0.001 | 120 (60.2%) |
| Absent | 59 | 20 | 79 (39.8%) | |
| • EVB | ||||
| Present | 56 | 38 | 0.774 | 94 (46.8%) |
| Absent | 60 | 45 | 105 (53.2%) | |
| • HRS | ||||
| Present | 0 | 23 | <0.001 | 23 (11.4%) |
| Absent | 116 | 60 | 176 (88.6%) | |
| • SBP | ||||
| Present | 12 | 16 | 0.097 | 28 (14.1%) |
| Absent | 103 | 66 | 169 (85.9%) | |
| • UTI | ||||
| Present | 30 | 22 | 0.999 | 52 (26.1%) |
| Absent | 85 | 60 | 145 (73.9%) | |
| • Sepsis | ||||
| Present | 2 | 10 | <0.05 | 12 (6%) |
| Absent | 113 | 72 | 185 (94%) | |
| • Pneumonia | ||||
| Present | 10 | 15 | 0.054 | 25 (12.6%) |
| Absent | 104 | 67 | 171 (87.4%) | |
| • Need for MV | ||||
| Present | 5 | 18 | <0.001 | 23 (11.4%) |
| Absent | 110 | 64 | 174 (88.3%) |
HE: hepatic encephalopahy. EVB: esophageal variceal bleeding. HRS: hepatorenal syndrome. SBP: spontaneous bacterial peritonitis. UTI: urinary tract infection. MV: mechanical ventilation.
Comparison of prognostic model scores and duration of ICU stay in patients who died or were discharged from the ICU (Mann-Whitney U test is used).
| Prognostic models | All patients | Discharged | Died | U | p-value |
|---|---|---|---|---|---|
| CTP score | 10.3 ± 2.7 | 9.5 ± 2.4 | 11.4 ± 2.8 | 2738.000 | < 0.001 |
| MELD score | 22.3 ± 10.3 | 18.1 ± 7.1 | 28.0 ± 11.2 | 2215.500 | < 0.001 |
| APACHE II score | 18.1 ± 9.4 | 13.4 ± 4.8 | 24.6 ± 10.4 | 1273.500 | < 0.001 |
| SOFA score | 6.1 ± 3.9 | 4.2 ± 2.6 | 8.7 ± 4.0 | 1756.000 | < 0.001 |
| Duration of ICU (hour) | 148.8 ± 100.8 | 134.4 ± 110.4 | 160.8 ± 153.6 | 4495.500 | 0.802 |
ICU: Intensive Care Unit. CTP: Child-Turcot-Pugh. MELD: model for end-stage liver disease. APACHE II: acute pysiology and chronic health evaluation II. SOFA: sequential organ failure assesment.
Stage stratification according to CTP score revealed 9.7% of the patients being in CTP stage A, 30.1% in CTP stage B and 60.2% in CTP stage C, with respective mortality rates of 15.8, 30.5 and 50.8%. A statistically significant link between CTP score and prognosis was established (p < 0.001).
The CTP, MELD, SOFA and APACHE II scores of patients who died were compared with those who were discharged from the ICU (Table 2; Figure 1). Patients who survived had mean scores of 9.5 ± 2.4 for CTP, 18.1 ± 7.1 for MELD, 13.4 ± 4.8 for APACHE II and 4.2 ± 2.6 for SOFA, compared to respective scores of 11.4 ± 2.8, 28.0 ± 11.2, 24.6 ± 10.4 and 8.7 ± 4.0 in those who died. The difference was statistically significant for each of the prognostic models (p < 0.001).
AUROC values for the SOFA, APACHE II, MELD and CTP scores were 0.84, 0.82, 0.78 and 0.72, in descending order (Table 3 and Figure 2). Sensitivity, specificity and accuracy of each scoring system in predicting mortality was calculated (Table 4).
Area under the curve of prognostic model scores.
| Test result variable | Area | P value | 95% Confidence Interval |
|---|---|---|---|
| APACHE II | 0.82 | < 0.001 | 0.750 - 0.872 |
| SOFA | 0.84 | < 0.001 | 0.778 - 0.894 |
| MELD | 0.78 | < 0.001 | 0.714 - 0.843 |
| CHILD | 0.72 | < 0.001 | 0.704 - 0.810 |
APACHE II: acute physiology and chronic health evaluation. SOFA: sequential organ failure assessment. MELD: model for end-stage liver disease. CTP: Child-Turcotte-Pugh.
Sensitivity, specificity and accuracy of prognostic models based on cut-off values determined by receiver operating characteristic (ROC) curve analysis.
| Prognostic model | Cut-off value | Sensitivity (%) | Specificity (%) | Accuracy |
|---|---|---|---|---|
| CTP | 10.5 | 69 | 67 | 0.68 |
| MELD | 19.5 | 79.5 | 64 | 0.79 |
| APACHE II | 15.5 | 76 | 74 | 0.75 |
| SOFA | 5.5 | 81 | 65 | 0.74 |
CTP: Child-Turcot-Pugh. MELD: model for end-stage liver disease. APACHE II: acute pysiology and chronic healt evaluation II. SOFA: sequential organ failure assesment.
With this study we managed to demonstrate that the SOFA model is the best prognostic indicator for cirrhotic patients requiring admission into the ICU. This was followed by the APACHE II, MELD and CTP models in descending order (AUROC values: 0.847, 0.821, 0.790 and 0.724).
CTP score, which was initially termed Child-Tur-cotte score, originally designed for predicting the outcome after surgery for portal hypertension (por-tocaval shunting and trans-section of the esophagus) in patients with cirrhosis, has been used for more than two decades for determining prognosis in cirrhotic patients.3 According to the CTP classification, 9.7% of our patients were in CTP stage A, 30.1% were in CTP stage B and 60.2% were in CTP stage C. Most of the cirrhotic patients (82.1%) had decompensated disease admission to the ICU. Mortality rates for each of the three stages were 15.8, 30.5 and 50.8%, respectively. The relationship between a higher CTP score and mortality was statistically significant, while also conveying a higher rate of ci-rrhotic complications.
Despite involving numerous subjective parameters and its limited scope of definition, CTP is still the most commonly used scoring system in the determination of prognosis in cirrhotic patients. In one such study by Botta, et al., 1-year mortality rates of patients with CTP A, B and C were 12, 25 and 44%, respectively.4 Ho, et al. reported on mortality rates of 20, 41.9 and 81.6% in ascending order of CTP class.5 Similar findings were also reported by Wehler, et al.6 Furthermore, a metaa-nalysis on 118 studies clearly established that higher CTP scores and the presence of more complications were associated with higher mortality rates.3
On the other hand, some investigators have suggested that the CTP score had many short-comings when used to determine post-operative mortality in cirrhotic patients.7,8 This has been attributed to the use of subjective parameters such as the presence of ascites and encephalopathy as well as it being deficient with regard to other conditions that may be encountered in ICU patients, unrelated to cirrhosis. Although CTP scores may correctly indicate severity of disease, CTP remains a poor prognostic model in cirrhotic patients with multiorgan failure as well as a poor predictor of mortality.7,9,10
MELD score was superior to CTP score. The MELD score includes parameters such was bilirubin, creatinine and INR, making it more objective and easily reproducible.4,11,12 Previous studies have demonstrated the accuracy of the MELD score in predicting prognosis.4,13 In a study by Papeatheodo-ridis, et al., on decompensated cirrhotic patients’ while both the MELD and CTP scores accurately predicted survival at 3 and 6 months, MELD score was found to be slightly superior at predicting survival at 12 and 24 months.14 Sumskiene, et al., also demonstrated that MELD score was better than CTP score at predicting short-term prognosis. However, for the long term, both models had similar predictive value for survival.15 Similarly, Botta, et al. demonstrated that as a prognostic model, the MELD score was superior to the CTP score at predicting 1-year survival in cirrhotic patients, while also establishing a correlation between MELD score and declining liver function.4
Despite being superior to CTP score in predicting prognosis, the MELD score involves many different variables and requires several logarithmic calculations, thus making it more complex and difficult to calculate at the bedside.16 Furthermore, although the MELD score utilizes objective data, creatinine in particular may be affected by several conditions (infection, hydration, and drugs), and any variations in creatinine levels may result in dramatic changes in MELD score. A major drawback of the MELD score is that it does not include a parameter related to portal hypertension, which may result in a deceivingly low score in patients with complications of hypertension and decompensated cirrhosis.15 In a study by Yoo, et al., a correlation between MELD score and cirrhotic complications such as hepatic en-cephalopathy and ascites could not be established.16
In our study, hepatic encephalopathy, GI bleeding and infections were the most common reasons for admission to the ICU in cirrhotic patients with complicated advanced liver disease. In what might be considered another disadvantage of the MELD score, this model is clearly insufficient at predicting outcome in cirrhotic patients who develop esophagus variceal bleeding, spontaneous bacterial peritonitis and hepatic encephalopathy.17,18
APACHE II score is one of the most widely used prognostic models in ICU patients. The validity of the APACHE II model in predicting prognosis in critical cirrhotic patients admitted to the ICU has been demonstrated in several studies.5,6,19,20 In a study by Ho, et al., on 135 patients with complicated cirrhosis who required intensive care, higher CTP and APACHE II scores were both found to be correlated with increased mortality, the APACHE II score being of better prognostic value (AUROC values 0.833 vs. 0.75).5 In another study by Arabi, et al., a statistically significant relationship between APACHE II score and prognosis was established in 129 cirr-hotic patients admitted to the ICU.21
Results of our study have shown the SOFA score to be the best prognostic model, among the scoring systems studied, at predicting prognosis in cirrhotic patients admitted to the ICU. Other studies have demonstrated that the SOFA score is not only useful in grading organ dysfunction in cases with sepsis, trauma or after surgery, but that it is also the best prognostic indicator that could be used for cirrhotic patients.6,12,22 In a study on 160 patients with cirrhosis admitted to the ICU, Tsai, et al. demonstrated that the SOFA score was better than the CTP score in predicting mortality.22 Chen, et al. reported a mortality rate of 68.6% among 102 cirrhotic patients admitted to the ICU. They also reported the SOFA score to be an excellent predictor of prognosis in comparison to the CTP score.7 In another study, Cholongitas, et al. compared the prognostic value of SOFA, APACHE II, MELD and CTP scores while evaluating 6-week mortality of 312 cirrhotic patients admitted to the ICU. They reported the SOFA model to be the best, and the CTP score the worst indicator. Furthermore, the MELD score was found to be superior to the APACHE scores (AUROC values for SOFA, MELD, APACHE II and CTP were 0.83, 0.81, 0.78 and 0.72, respectively). Six-week mortality rate was calculated at 65.1%.12 In yet another study, Wehler, et al. enrolled 143 cirrhotic patients who were admitted to the ICU. They demonstrated that the SOFA score had an excellent predictive value in determining short-term prognosis, and was superior to both the APACHE II and CTP scores (AUROC values for SOFA, APACHE II and CTP were 0.94, 0.79 and 0.74, respectively). They also reported on an ICU mortality rate of 36%, overall hospital mortality rate of 46% and 6-month mortality rate of 56%.6
The SOFA score is an excellent model in that it provides an easy to apply scoring system which may be used to provide objective information to patients and their relatives regarding the prognosis of the disease, as well as helping in making clinical decisions regarding management. Despite all its merits, the SOFA score is not without its limitations. It utilizes variables from the Glasgow coma scale used to evaluate neurological dysfunction, and the subjective nature of these parameters may result in random errors of evaluation, particularly since cognitive abilities of ICU patients are frequently altered by used of sedatives and analgesics.6
In conclusion, all of the scoring systems in use today may be helpful in determining prognosis of ci-rrhotic patients admitted to the intensive care unit. In terms of prognostic value, the SOFA and APACHE II score are superior to the MELD and CTP scores. As such, the SOFA and APACHE II scales should perhaps be the preferred model of choice and have shown the SOFA score to be the best prognostic model.
Conflict of InterestThere is no financial support.
Authors declare no conflict of interest related to this article.