Spontaneous hepatic rupture (SHR) during pregnancy is a rare but well known complication and it usually occurs alongside eclampsia or HELLP syndrome. SHR in uncomplicated pregnancy is extremely rare and can be associated to different undiagnosed pathological conditions. We report the case of a nulliparous woman, 27 weeks pregnant, with a peliosis hepatis, previously unknown, who was admitted to our unit due to SHR and massive hemoperitoneum. The conception was obtained by embryo transfer after multiple attempts of hormone-supported cycles using estrogens and progesterone. After emergency laparotomy the patient was submitted to deliver of the dead foetus and damage control of the hepatic bleeding source. At relaparotomy a right posterior sectionectomy (segments VI and VII) and segmentectomy of segment V were performed. The patient was discharged in good physical conditions after 18 days from admission. If hepatic rupture is suspected in a pregnant patient a collaborative multidisciplinary approach is mandatory. The cornerstones of medical and surgical management are highlighted. At the best of our knowledge this is the first case of SHR in a pregnant woman with peliosis hepatis. A possible correlation of an increased risk for SHR in a pregnant patient who was submitted to several attempts for embryo transfer is discussed. The relevant scientific literature of the possible causative role of the estrogen therapy in inducing politic liver damage is also reviewed.
Spontaneous hepatic rupture (SHR) in pregnancy represents one of the most life-threatening complications and is associated with a high maternal and perinatal mortality. SHR represents one of the most challenging conditions for both diagnosis and treatment.
SHR during pregnancy leading to hepatic intraparenchymal haemorrhage and consequent hepatic rupture most commonly involves the right liver lobe and is usually associated with pre-eclampsia and Hellp (haemolysis, elevated liver enzymes, low platelets) syndrome. The vast majority of cases (more than 80%) are associated with pre-eclampsia and SHR in uncomplicated pregnancies has less commonly been described.1–5 Many different conditions such as adenoma, hepatic lymphoma, hepatocellular carcinoma (HCC), hepatic sarcoidosis and tuberculosis as well as peliosis hepatis (PH) should be considered as conditions potentially inducing intraparenchymal large haematoma which can cause haemoperitoneum due to hepatic rupture and bleeding; these conditions are not necessarily associated with pregnancy and should always be ruled out in the presence of intrahepatic haematoma or overt signs of hepatic rupture during uncomplicated pregnancy.6–9 We present here the case of a 53-year-old woman, 27 weeks pregnant, with a known condition of antiphospholipid syndrome and peliosis hepatis, previously unknown, admitted to our unit due to SHR and massive haemoperitoneum.
Clinical CaseA 53 years old woman was transferred at 9 pm in our emergency department (Level I Hospital) from a Level II Hospital for abdominal pain and hypotension. The woman was 27 weeks pregnant. The conception was done by embryo transfer in a foreign country in Eastern Europe. The medical history of the patient revealed that she was suffering from an-tiphospholipidic syndrome (MTHFR heterozygous mutation, LAC positive), with the presence of anticardiolipin and anti-beta 2 glycoprotein antibodies. She had no history of liver disease and she denied alcohol or drug abuse. To prepare for embryo transfer the patient underwent several cycles of hormonal-supported therapy using estrogens and progesterone from 2005 to 2013. During the first cycle she received leuproreline 1 mg, follitropin alpha 450 IU, menotropin 75 IU day for 15 days. During the next years she received 20 further different cycles lasting 1 and 2 weeks with different protocols of therapy: triptorelin 3.75 mg, estradiol valerate 1 mg, progesterone 200 mg (tablets per os), transdermal estradiol emidrate, and during the last 4 days of each cycle 10 mg of prednisone and antithrombotic prophylaxis by 6,000 IU of subcutaneous injections of nadroparin calcium. At the end of July 2013 she was submitted to a new attempt by embryo transfer with an in-vitro fertilization of three eggs: only one of the three embryos was progressing well and a successful pregnancy was obtained.
At 16 weeks, a doubt of hydatiform mole was considered due to an elevated level of BHGC, which was soon excluded after normalization of the hormonal values.
During the afternoon she was complaining of a continuous and worsening abdominal pain in the right upper quadrant and the patient was evaluated in the Emergency of Level II Hospital: the vital parameters were all normal. Blood tests evidenced haemoglobin (Hb) 9 g/dL and Alanine Transferases of 70mU/L( n.v. 40). Ultrasound (US) showed free abdominal fluid and hepatic haematoma in the right lobe. The foetal heart sound was normal and there were no images suggesting placental abruption. Six hours later the vital signs of the patient worsened with a systolic blood pressure (SBP) falling to 70/50 mmHg, Hb 6 mg/dL, lactate 6 mEq/L; the foetal heart sound was still viable. The patient was transfused with 2 units of red blood cells (RBC) and 2
units of fresh frozen plasma (FFP) and then transferred to our Hospital.
The patient was admitted to the emergency department of our Hospital at 9 pm. Her systolic blood pressure was still 70 with a heart rate of 110 bpm despite transfusion of 2 packets of RBC. Arterial blood gases showed a ph of 7.22, with Hb 9.7 g/dL, lactate 14.3. The US performed by the gynaecologist evidenced that the foetal heart sound was absent. The patient was soon intubated and submitted to a CT scan that showed active bleeding from the placenta (Figure 1) and massive haemoperitoneum from a huge hepatic haematoma of the right lobe (Figure 2).
An emergency laparotomy was performed with a midline incision. A large haematoma of the right liver was evident with a large hepatic rupture of the right hepatic lobe. Haemostasis of the liver was achieved by full liver packing: during the same time the gynaecologists opened the uterus to pull out the dead foetus. No evidence of placental abruption or active focal intrauterine bleeding was detected. The haemostasis of the uterus was difficult, and was temporarily obtained by bimanual compression and soon after by haemostatic compression suturing technique (Hayman technique).10
During the procedure the patient received 4 unit of RBC, 3 unit of FFP and 1 pool of platelets. Lactate blood level was still 4.6, and a SBP above 100 mm Hg was achieved by continuous noradrenalin infusion support. After a first attempt to remove the packing due to apparent bleeding control of the several bleeding sources, we decided to redo full liver packing without closing the abdomen. The patient was admitted to the ICU at 2 pm with a packed open abdomen and with the standard Jackson-Pratt drain.
The following day, the patient underwent another CT scan that showed persistent bleeding from the right lobe of the liver. To obtain hemodynamic stability we decided to undertake surgical re-exploration: After liver de-packing, the liver bleeding was still active. To achieve haemostatic control and for debridement of all devascularized hepatic tissue, a right posterior sectionectomy (Segment VI and Segment VII) and segmentectomy of Segment V was performed as the only available surgical option. The abdomen was then closed.
During postoperative course the blood tests normalized and the patient’s condition improved. Drowsiness and confusion appeared at day 3 p.o. Mild hepatic encephalopathy was diagnosed by the neurologist and confirmed by EEG. After a course of treatment with lactulose by enemas and neomycin the patient improved her level of consciousness and completely recovered after 2 weeks. She was discharged 18 days p.o. in good physical condition without post-operative complications.
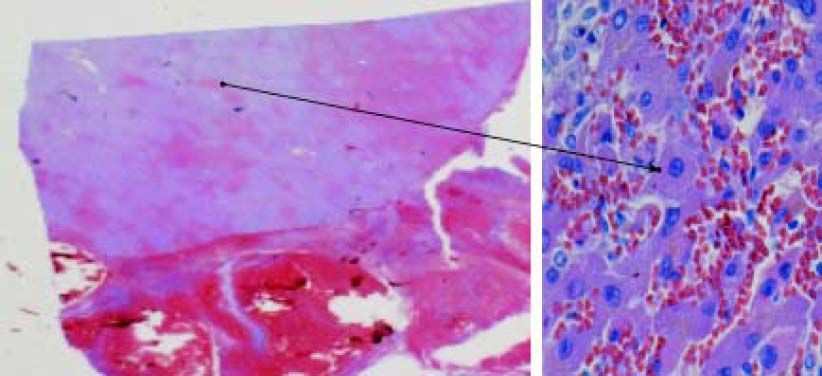
The biopsy specimen demonstrated hepatic parenchyma with widening of sinusoidal bed compatible with Peliosis Hepatis; liver fibrosis was absent (Figure 3).
DiscussionAs first described by Abercrombie in 1844 as a complication of pregnancy SHR is a rare but well-known complication during pregnancy 11 and it usually occurs alongside pre-eclampsia, eclampsia or HELLP syndrome with around 200 cases reported in world literature.6 SHR in uncomplicated pregnancy has also been reported but is extremely rare.12 Various uncommon underlying conditions associated with a spontaneous liver rupture and spontaneous haemorrhage have been described.13–16 These include bleeding from hemangiomata, hepatic metastases from choriocarcinoma, hepatocellular carcinoma, adenoma, trauma, infections (malaria, syphilis, rupture of amoebic abscess), aneurysmata, granulomata from sarcoidosis, the use of cocaine during pregnancy, anabolic steroid therapy, systemic amyloidosis and peliosis hepatis (PH).17–19 As spontaneous liver haemorrhage is associated with significant mortality both for the mother and for the child, a high index of suspicion of SHR should be maintained in all pregnant women with presenting symptoms of abdominal pain, shoulder pain, nausea, vomiting or vaso-vagal symptoms with unexplained tachycardia and hypotension. Upon clinical examination, signs of peritonitis can be present and the foetal heart sound may be weak or absent. SHR should be fully investigated especially in multiparous pregnant women over the age of 30. As with most cases, and in our patient, liver rupture occurs in the third trimester of pregnancy or within the first 24 h postpar-tum. In around 75% of cases SHR is a solitary injury in the right liver lobe, and in 11% of cases in the left liver lobe; in 14% of patients, a bilateral injury of both lobes can be evident.20
Due to its high mortality rate, all patients with suspected HSR should undergo specific diagnostic protocols as soon as possible.
The hemodynamic conditions of the patient determine the algorithm of investigations to be performed. In a haemodynamically stable patient, a fast-US followed by a CT scan (usually without contrast medium) is the most useful investigation. This allows the surgeon to quantify the liver injury, to define the underlying hepatic disorders - at least at the level of diagnostic suspicion - and to plan all possible treatment modalities. If the patient is hemodynamically unstable, after an urgent fast-US showing intra-abdominal blood collection, an urgent laparotomy must be performed. If the rupture occurs during pregnancy, delivery of the foetus should be the first step. A classic Pfanennstiel incision should be avoided, because the full abdomen cannot be visualized unless a second upper abdominal incision is made. A median xyfo-pubic laparotomy is therefore the recommended approach that offers the great advantage of visualizing the entire abdomen, the speed of execution with the possibility to perform temporary clamping of hepatic hilum and damage control of the bleeding source from the hepatic parenchyma by liver packing. In the case of our patient, the intrauterine foetal death was established upon arrival at our emergency department following the first resuscitation. The hemodynamic instability of the patient on arrival was temporarily counterbalanced and this allowed us to perform a fast CT scan without contrast medium for a correct diagnosis.
At laparotomy, the liver parenchyma - unaffected by rupture and by haematoma-appeared macroscopically healthy; this observation posed some concerns about the possibility that the bleeding source could be from an unrecognized intra-hepatic liver neoplasm and this consideration increased our propensity for liver resection. However, final histological diagnosis of the removed hepatic parenchyma evidenced PH.
PH is an abnormality of the reticuloendothelial system of the liver classified as a benign vascular disorder with multiple blood filled lacunar lesions within the hepatic parenchyma (Figure 3) and can occur at any age. Although early onset has been reported, PH usually develops in adults regardless of gender, it is most often asymptomatic and is incidentally found at autopsy. The aetiology of PH is still unknown. The theory that toxic substances may induce peliosis is supported by the finding of increased endothelial cell permeability with numerous red blood cells in the space of Disse. The idiopathic pure hepatic sinusoidal dilatation can be associated with immunological features of antiphospholipid syndrome 21 as in the case of our patient. More commonly, PH can be induced by several diseases such as tuberculosis, malignancy, human immunodeficiency virus infection, organ transplantation and drug administration including anabolic steroid use, azathioprine, corticosteroid, and tamoxifen. Generalized PH leading to liver cirrhosis has also been observed after long-term use of contraceptives.22–24
Patients may be asymptomatic or present cholestasis, hepatomegaly, portal hypertension, ascites, liver failure, and hepatic encephalopathy. Massive intrahepatic haemorrhage and hemoperito-neum can be related to progressive dilatation and the rupture of subcapsular cysts. Surgery should be reserved for those particular cases where haemorrhage is life threatening as in our patient. PH should be distinguished from hepatocellular carcinoma, hyper-vascular metastases, hemangiomata, abscess and pseudo-tumours. Familiarity with the imaging characteristics can suggest earlier diagnosis of PH during a CT scan, and contrast-enhanced CT scans usually show the heterogeneous enhancement of the lesion during the arterial phase and the centripetal progression of contrast enhancement during the portal venous and delayed phase, which is isodense to the adjacent normal parenchyma.25
PH should be considered in the light of a differential diagnosis for all atypical focal hepatic lesions and in the presence of spontaneous hepatic rupture during pregnancy when eclampsia, pre-eclampsia and Hellp syndrome have been excluded. SHR secondary to PH should be also considered in all patients who have received multiple cycles of hormonal-supported therapy using estrogens and progesterone.
Localized PH with a complicated fatal haemorrhage may require hepatic artery catheterization and embolization or partial hepatectomy. Delivery of the foetus and damage control by packing of the liver injury should be the first surgical approach. Partial hepatectomy should be considered as the subsequent surgical procedure when the bleeding source remains uncontrolled or in the presence of any other major complications such as bile collections or hepatic abscess. Total hepatectomy may rarely be required when rupture of liver parenchyma affects more than 75%, or in the presence of major injuries to the suprahepatic veins, or when after hepatic resection the liver remnant is diffusely affected by an advanced stage of peliotic disease. In those cases a temporary veno-venous bypass by centrifugal pump or port-caval shunt followed by super-urgent liver transplantation are the only available option.
If hepatic rupture is suspected in a pregnant patient a collaborative surgical approach between emergency surgeons and gynaecologists is mandatory.20 Pfannenstiel incision should be avoided since it does not allow either for adequate assessment of liver injury or for damage control of liver haemorrhage. Hemodynamic stabilization of the patient is the first priority and can be only obtained by median xyfo-pubic laparotomy since it offers the great advantage of visualizing the entire abdomen, and to proceed simultaneously to delivery of the foetus with the possibility to perform temporary clamping of hepatic hilum and to obtain the damage control of the bleeding source. Liver resection of any necrotic portions of the liver tissue should be postponed after stabilization of the patient.
AcknowledgmentsThe authors thank Ryan Wade and Vittoria Aseni for their assistance in preparing the manuscript.
Conflict of InterestNone.