Transjugular liver biopsy was first reported in 1967. Since then, this technique has been broadly performed in many medical centers around the world. The number of its indications has increased, and by modifying the needles, the quality of the liver tissue sample has improved. The advantage of transjugular biopsy is that it can be performed in patients in whom the use of percutaneous biopsy is contraindicated Indications for transjugular liver biopsy are, precisely, most of the contraindications for percutaneous liver biopsy. This fact increases the number of patients that can benefit from this procedure.
In most cases, the procedure is successfully performed. Minor complications may occur in 1% to 15% and major complications (perforation of the hepatic capsule, cholangitis, and intra-peritoneal bleeding) are observed in 1-3% of the cases. Mortality related to the procedure varies form 0.2 to 0.3%.
It has been reported that diagnosis yielded by transjugular liver biopsy induced changes of treatment in 50% of patients with an acute hepatic illness, in 62% of the patients with a chronic hepatic illness, and in 87% of the patients with liver transplants. In conclusion, transjugular liver biopsy is a useful procedure in the diagnosis of hepatic diseases. Its success rate is high; it is a very safe procedure because complications and mortality are rare; and it is well tolerated by patients.
Liver biopsy is one of the most useful diagnostic procedures for liver diseases. It is also useful to evaluate response to treatment. This procedure was first described in 1883 by Paul Elrich, and later by Menghini in 1958.1
Because of the heterogeneity of hepatic lesions, several ways of access to the liver have been developed, in order to obtain a tissue sample for study. Each of the following approaches offers certain advantages that the other methods do not have: 1) Percutaneous liver biopsy (blind or directed by ultrasonography); 2) Transjugular liver biopsy and 3) Liver biopsy through laparoscopy.
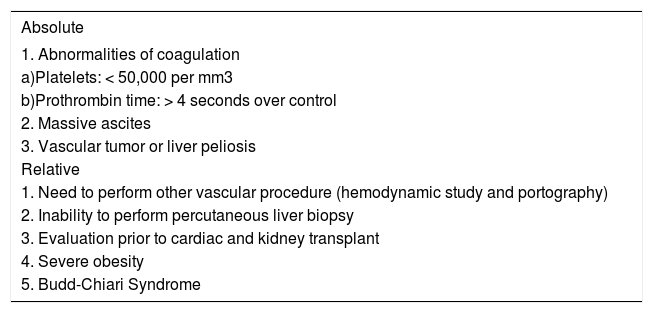
The advantage of transjugular liver biopsy is that it can be performed in patients in whom the use of percutaneous biopsy is contraindicated (Table I). This fact increases the number of patients that can benefit from this procedure.
Indications for transjugular liver biopsy.
| Absolute |
|---|
| 1. Abnormalities of coagulation |
| a)Platelets: < 50,000 per mm3 |
| b)Prothrombin time: > 4 seconds over control |
| 2. Massive ascites |
| 3. Vascular tumor or liver peliosis |
| Relative |
| 1. Need to perform other vascular procedure (hemodynamic study and portography) |
| 2. Inability to perform percutaneous liver biopsy |
| 3. Evaluation prior to cardiac and kidney transplant |
| 4. Severe obesity |
| 5. Budd-Chiari Syndrome |
This review analyzes the current status of transjugular liver biopsy as it relates to its usefulness in diagnosis and treatment of liver diseases.
Transjugular liver biopsyIn 1967, Hanafe and Weiner published the first cases of transjugular liver biopsy. Later, Rosch et al. reported a greater number of patients.2 Since then, this technique has been broadly accepted in many medical centers around the world. The number of its indications has increased, and by modifying the needles, the quality of the liver tissue sample has improved.
Transjugular liver biopsy consists of obtaining liver tissue through a needle that is introduced in the jugular vein, and through it, a long catheter through the superior vena cava, the right atrium, the inferior vena cava and on through one of the hepatic veins, under fluoroscopic control. With the catheter in this position, a biopsy needle, 55 cm long, is introduced down to the hepatic vein, and by transfixion of the venous wall, the needle is introduced into the liver parenchyma, to obtain the liver tissue by aspiration or cut (Figure 1).
Measures of the pressure of the hepatic veins, the inferior vena cava and right atrium may be performed, prior to taking the biopsy. With these values, the hepatic venous pressure gradient (wedge minus free hepatic vein pressure) is calculated, which is equivalent of the pressure in the portal vein. This gradient is useful for the diagnosis and treatment of portal hypertension.
This technique has been extensively accepted in many medical centers and is currently in use at our hospital.3
Indications and contraindicationsIndications for transjugular liver biopsy are, precisely, most of the contraindications for percutaneous liver biopsy (Table I).4-6
Contraindications for transjugular liver biopsy are: 1) Hydatid Cyst, because of an accidental puncture, which may cause anaphylaxis. Other cysts, have the potential risk of causing bleeding after communicating with a vein; 2) obstruction of the main biliary tract, with dilatation of the intrahepatic biliary tree, because of the risk of hemobilia and 3) cardiac anomalies, which may give rise to arrhythmia. 7,8 Right jugular vein thrombosis renders it necessary to puncture the left jugular vein in order to access the liver, thus, representing greater technical difficulties.
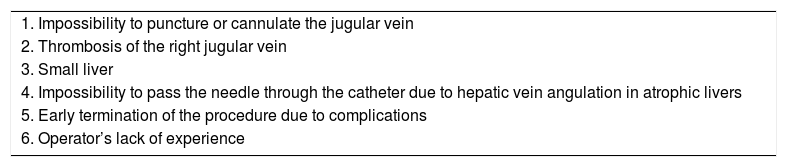
Success and failure of the techniqueIn most cases, the procedure is successfully performed. However, in a small number of cases (4 to 8%) the procedure cannot be done because of the various factors described on Table II. Some of these factors are operator’s experience depending, while others are inherent to the patient’s anatomy.9
Causes of procedure failing.
| 1. Impossibility to puncture or cannulate the jugular vein |
| 2. Thrombosis of the right jugular vein |
| 3. Small liver |
| 4. Impossibility to pass the needle through the catheter due to hepatic vein angulation in atrophic livers |
| 5. Early termination of the procedure due to complications |
| 6. Operator’s lack of experience |
The size of the tissue sample is important for an adequate pathologic interpretation. In the transjugular liver biopsy the tissue sample size may vary, depending on the technique used (aspiration or cutting) and the characteristics of the hepatic lesion (cirrhosis or non-cirrhosis). Oftentimes, samples obtained by aspiration are small and fragmented. A tissue sample is considered adequate when it contains at least between 6 and 8 portal triads, particularly in chronic hepatic lesions.2
The operator’s experience seems to be an important factor in obtaining a tissue sample that is adequate for pathologic interpretation. It has been reported that when the operator has performed over 20 biopsies, 93% of the samples obtained are adequate for diagnosis. When operator’s experience is greater than 100 performed biopsies success rate is 97.1%.10
McAffe compared transjugular liver biopsy to percutaneous biopsy and found that samples obtained through the transjugular technique were of a smaller size (0.8 + 0.4 v. s. 2.2 + 0.8 cm). However, transjugular biopsies were adequate for diagnosis in 69% of the times, marginal in 23%, and inadequate in 8%, while with the percutaneous technique the frequencies were 87%, 10%, and 3% respectively. None of the differences between values from both techniques was statistically significant.11 These results were corroborated by another study.12
The pathologist’s experience is a key factor to diagnose marginal size samples. It has been found there is a learning curve after which results of the pathologic interpretation improve. Recently designed needles permit obtaining samples, by cutting, in order to improve their sizes, particularly in patients with hepatic cirrhosis, where the use of aspiration needles have some limitations.13-16 When samples for diagnosis of cirrhosis are inadequate, the use of hepatic venous pressure gradient may be useful to diagnose cirrhosis in up to 97% of the cases.17
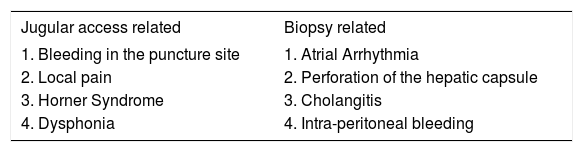
ComplicationsThe procedure is not free of complications. In general, these may be divided into minor and major complications. Minor complications may occur in 1% to 15%. They are: bleeding from the vein puncture site, hematoma, localized pain, and less frequently, Horner Syndrome, paresthesia, dysphonia and cardiac atrial arrhythmia caused by catheter manipulation on the right atrium, which ceases spontaneously in most cases.7,10-12,18 Major complications are observed in 1-3% of the cases. They are: perforation of the hepatic capsule, cholangitis, and intra-peritoneal bleeding (Table III). The later is probably the most severe of complications, and it occurs in 0.2 to 0.4% of the cases.7,11 Mortality related to the procedure varies form 0.2 to 0.3%.7,10,11,19
Clinical impactWhen a liver biopsy is prescribed, the following factors must be taken into account: a) risks for the patient, b) potential benefits in regards to diagnosis, and c) the impact on the therapeutic decisions. In a previously published study, 1500 patients subjected to transjugular liver biopsy were evaluated. The biopsy was useful in confirming the diagnosis in 61% of the cases, and it had an influence on the treatment prescribed in 16%.10 Papatheodoridis reported that diagnosis yielded by transjugular liver biopsy induced changes of treatment in 50% of patients with an acute hepatic illness, in 62% of the patients with a chronic hepatic illness, and in 87% of the patients with liver transplants.18 The impact on the treatment modifications was more conclusive in patients with an acute hepatic illness or with a transplant, than those with a chronic hepatic disease. 20,21 In the later, it was more useful to establish the illness stage. McAffe reported the impact of transjugular liver biopsy on diagnosis on a study of 124 biopsies. 11 Transjugular liver biopsy confirmed the diagnosis in 55% of the patients, established a new diagnosis in 12%, and induced changes of the therapeutic management of 22% of the cases.
ConclusionsTransjugular liver biopsy is a useful procedure in the diagnosis of hepatic diseases. Its success rate is high; it is a very safe procedure because complications and mortality are rare; and it is well tolerated by patients. This procedure complements percutaneous liver biopsy because it makes it possible to take biopsies from patients where the use of this pathway is contraindicated. It also has the advantage of allowing a hemodynamic study to diagnose portal hypertension and to evaluate its pharmacologic treatment.
The disadvantages it may have are: 1) it is a complex procedure that requires specialized equipment and trained personnel, 2) greater costs than those of a percutaneous liver biopsy, and 3) tissue samples are smaller than with percutaneous liver biopsy, in patients with hepatic cirrhosis. However, the recent design of new needles, which have a cutting mechanism, has enhanced the size of samples obtained.
Disadvantages can be minimized when transjugular liver biopsy is performed at referred specialized medical centers, allowing this technique to be applied more extensively. In the era of organ transplants, transjugular liver biopsy is significantly useful in diagnosis and in pre and post operatory evaluation.