Improving Access to Psychological Therapies (IAPT) services were set up in the United Kingdom in 2008. Recent service expansion now accommodates patients with long-term conditions (LTC) and medically unexplained symptoms (MUS) through the use of cognitive-behaviour therapy (CBT). A systematic review is yet to be completed to identify specific adaptions that may be effective for improving outcomes. Many countries are building upon this model within the United Kingdom; therefore, the findings can inform developing services internationally.
MethodsElectronic databases were searched and studies were screened against an inclusion/exclusion criteria. Studies evaluating the effectiveness of CBT interventions on mental health outcomes for adults with LTC/MUS within primary care were included. Data were extracted for analysis and a narrative synthesis was conducted. Quality assessments were made using the Effective Public Health Practice Project tool.
ResultsOf 14,380 papers, eight papers were included within the review. Moderate to strong evidence found CBT adaptions were effective in improving outcomes, including the specific focus on the LTC/MUS within treatment, the inclusion of collaborative care or implementing a range of therapeutic skills. Weak methodology was associated with selection bias, lack of blinding and reporting around the validity and reliability of data collection tools.
ConclusionsCBT adaptions may be effective at improving mental health outcomes for those with LTC/MUS in the short term. Due to the small amount of studies included within the review, conclusions remain tentative. It is unclear as to whether interventions can sustain outcomes and provide financial gains in the long term.
En 2008 se establecieron en el Reino Unido servicios de mejora del acceso a las terapias psicológicas (IAPT). La reciente ampliación de los servicios permite ahora atender a los pacientes con afecciones a largo plazo y síntomas médicamente inexplicados mediante el uso de la terapia cognitivo-conductual. Todavía no se ha completado un examen sistemático para identificar adaptaciones específicas que puedan ser eficaces para mejorar los resultados. Muchos países están aprovechando este modelo en el Reino Unido; por consiguiente, los resultados pueden servir de base para el desarrollo de servicios a nivel internacional.
MétodosSe realizaron búsquedas en las bases de datos electrónicas y se examinaron los estudios en función de un criterio de inclusión/exclusión. Se incluyeron estudios que evaluaban la efectividad de las intervenciones de TCC en los resultados de salud mental para adultos con LTC/MUS dentro de la atención primaria. Se extrajeron los datos para el análisis y se realizó una síntesis narrativa. Las evaluaciones de la calidad se realizaron utilizando la herramienta del Proyecto de Práctica de Salud Pública Efectiva.
ResultadosDe 14.380 trabajos, ocho fueron incluidos en la revisión. La evidencia moderada a fuerte encontró que las adaptaciones de la TCC fueron efectivas para mejorar los resultados, incluyendo el enfoque específico en el LTC/MUS dentro del tratamiento, la inclusión de la atención colaborativa o la implementación de una gama de habilidades terapéuticas. La metodología débil se asoció con el sesgo de selección, la falta de cegamiento y la presentación de informes sobre la validez y la fiabilidad de las herramientas de recopilación de datos.
ConclusionesLas adaptaciones de la TCC pueden ser efectivas para mejorar los resultados de salud mental de aquellos con LTC/MUS a corto plazo. Debido a la pequeña cantidad de estudios incluidos en la revisión, las conclusiones siguen siendo tentativas. No está claro si las intervenciones pueden sostener los resultados y proporcionar ganancias financieras a largo plazo.
A long-term condition (LTC) refers to a health condition that cannot be cured with a need for self-management (Department of Health, 2012) such as diabetes, cardiovascular or respiratory disease. Around fifteen million people have one or more LTC in the United Kingdom (UK) and this is expected to rise due to an ageing population and unhealthy lifestyle choices (Department of Health, 2012a). The term medically unexplained symptoms (MUS) refers to physical symptoms which cannot be explained by ‘disease specific, biomedical pathology’ (Department of Health, 2014) causing significant distress and impairing functioning. Symptoms such as tingling, tremors or headaches may be caused by problems in the nervous system, and are often be referred to as a ‘functional neurological disorder’ (NHS, 2018). However, MUS can also be part of a poorly understood syndrome such as chronic fatigue syndrome (CFS), irritable bowel syndrome (IBS) or fibromyalgia. Two thirds of those with LTCs and 70% of those with MUS also have a mental health problem (NHS, 2019) and between 12 and 18% of all national health service (NHS) costs associated with LTCs/MUS are directly linked to poor mental health outcomes (Naylor et al., 2016).
The relationship between physical and mental health is complex and bi-directional; research has found pre-morbid depression to significantly predict the onset of CFS (Moss-Morris & Spence, 2006) alongside anxiety and perfectionism being important predictors of IBS (Spence & Moss-Morris, 2007). Furthermore, untreated symptoms of anxiety and depression post diagnosis can predict particularly poor outcomes around self-management, health behaviours, mortality rates, employability and work attendance (NHS England, 2016). The need for integrated mental and physical health care is driven by this rising comorbidity (Naylor, 2012) including the co-location of services and working collaboratively to treat the ‘whole person’ (National Collaborating Centre for Mental Health, 2018). However, mental and physical health services are rarely joined up, further leading to poor outcomes (NHS England, 2019).
Improving Access to Psychological Therapies (IAPT) services were set up in 2008 to provide evidence based psychological therapies for those suffering from common mental health problems. High (HI) and low intensity (LI) cognitive behavioural therapy (CBT) is offered ranging between 8 and 20 sessions depending on the longevity and complexity of the mental health presentation. IAPT has been increasing access rapidly with 1.6 million people having been referred to the services for support within the past year (NHS Digital, 2019). As part of IAPT expansion, the government published ‘No Health without Mental Health’ (Department of Health, 2011) which identified the need for IAPT services to accommodate patients with LTCs and MUS in the form of poorly understood syndromes who also have associated mental health problems (Department of Health, 2008, 2012). As part of this initiative, the ‘Five Year Forward View’ (Care Quality Commission, 2015) stated that wider investment would support the implementation of new LTC-IAPT sites during 2017/18 across the UK. From 2018/19 integrated services started to support respiratory and cardiac conditions, diabetes and MUS. The primary aim of LTC-IAPT services is to improve mental health outcomes through considering the impact of their LTC on levels of depression and anxiety alongside addressing problematic beliefs and behaviours that may increase the impact of the LTC on the person (National Collaborating Centre for Mental Health, 2018). The services also aim to promote self-management of LTCs and are required to modify the delivery of the intervention, taking into account the patient's LTC. It is recommended that appropriate adaptions to therapeutic sessions should be made alongside the integration of physical health care team involvement to improve outcomes for patients. It is therefore important to assess the evidence around the effectiveness of adapted CBT interventions for this specific population.
Previous systematic reviews (SRs) have assessed the efficacy of CBT for those with respiratory disease and have included studies that were conducted outside of UK, primary care settings. These SRs suggest that CBT interventions are somewhat effective in improving mental health outcomes for those with chronic obstructive pulmonary disease (COPD) (Coventry & Gellatly, 2010; Pollok, van Agteren, Esterman, & Carson-Chahhoud, 2019; Smith, Sonego, Ketcheson, & Larson, 2014) and asthma (Kew, Nashed, Dulay, & Yorke, 2016; Pateraki & Morris, 2017; Yorke, Fleming, & Shuldham, 2006), however methodological rigour varied.
It has also been concluded that CBT is effective in improving mental health outcomes for those with diabetes (Kanapathy & Bogle, 2017; Li et al., 2017; Uchendu & Blake, 2016; Wang et al., 2017). However, the reviews did not include any trials conducted within the UK (Uchendu & Blake, 2016; Wang et al., 2017), found research of poor methodological quality (Kanapathy & Bogle, 2017) and did not report upon the setting of the research (Li et al., 2017).
A review completed by Reavell, Hopkinson, Clarkesmith, and Lane (2018) found moderate evidence for improved psychological outcomes for those with cardiovascular disease, however only one study was completed within the UK and the research setting was not reported.
Previous SRs examining the effectiveness of CBT for patients with MUS have found high quality evidence for improved mood amongst patients with fibromyalgia (Bernardy, Klose, Welsch, & Häuser, 2018). However, a meta-analysis assessing the effectiveness of online CBT interventions for patients with IBS found moderate quality evidence to show no significant improvement in psychological outcomes (Hanlon, Hewitt, Bell, Phillips, & Mikocka-Walus, 2018). No significant improvement in outcomes was also found when CBT delivered through a range of modalities was compared to other psychological interventions for those with IBS (Li, Xiong, Zhang, Yu, & Chen, 2014). Furthermore, moderate evidence was found to be inconclusive around the effects of CBT on mental health outcomes for CFS (Price, Mitchell, Tidy, & Hunot, 2008). All of the reviews conducted into CBT for MUS included secondary care and non-UK settings.
The effectiveness of CBT for LTCs/MUS within UK primary care settings has been reviewed within a service evaluation (de Lusignan et al., 2013) which found improvements in anxiety and depression symptoms, but with no improvement in health care costs through outpatient, accident and emergency attendance or admissions. Recommendations from this evaluation indicate the need for improved data quality and increased data collection in this field as the significance of these results were not tested.
AimsThe current review aims to identify how CBT interventions should be adapted for patients living with LTCs and poorly understood syndromes (referred to as MUS) within IAPT services. The review therefore includes studies that assesses the effectiveness of a CBT intervention for LTCs/MUS either completed within IAPT services or trials that recruited their participants through primary care providers within the UK. The LTC-IAPT model is unique to the UK and a review in this area has not previously been completed and therefore the systematic review (SR) aims to address this knowledge gap. This is important for an international audience as many countries are building upon the UK model including Norway, Australia, Stockholm, alongside many other countries within developing plans for IAPT-like services (Clark, 2019). The findings from the current review can therefore inform developing services internationally.
MethodsInclusion/exclusion criteriaStudies meeting the following eligibility criteria were included:
- 1)
Quantitative studies published after the year 2000 to reflect evidence from the same decade as changes in primary mental healthcare provision and the introduction of national institute of health and care and excellence (NICE) guidance.
- 2)
Adults aged 16 and over, due to some adult primary care services working with this age.
- 3)
Patients with respiratory/cardiac disease, diabetes and MUS including IBS, CFS, fibromyalgia and chronic pain were included (fitting with LTC-IAPT criteria).
- 4)
Interventions delivered one to one, (in person or over the telephone) due to this being the main mode of delivery within primary care (Perfect, Jackson, Pybis, & Hill, 2016).
- 5)
Quantitative studies from IAPT services or any trial recruiting participants from primary care settings (e.g., GP referral).
- 6)
Studies including quantitative mental health outcomes; primary physical health outcomes will also be noted.
- 7)
Studies conducted within the UK and written in English.
Studies were excluded if they were qualitative in nature, conducted outside the UK, published before the year 2000, were delivered or recruited outside of a primary care setting (e.g., specialist clinics) and/or did not include mental health outcomes. Any papers including group or online interventions were also excluded, papers including children aged under the age of 16 and did not provide a breakdown of results by age, or those with an LTC/MUS that is not treated by LTC-IAPT were also excluded.
Search strategyThe following databases were searched: MEDLINE, EMBASE, PsycINFO, CINAHL and the Cochrane Library. Reference lists of selected articles were scanned for relevant studies and key authors in the field were contacted. A search for grey literature through online search engines and of the NICE evidence database was completed in order to address publication bias.
Search terms and Boolean phrases were identified (see Appendix A) through a scoping of search terms within relevant articles. The search was last run on 12/05/20 and built-in limiters were used to restrict searches to adult participants, human participants, any journal type, journals published in the English language and published after the year 2000.
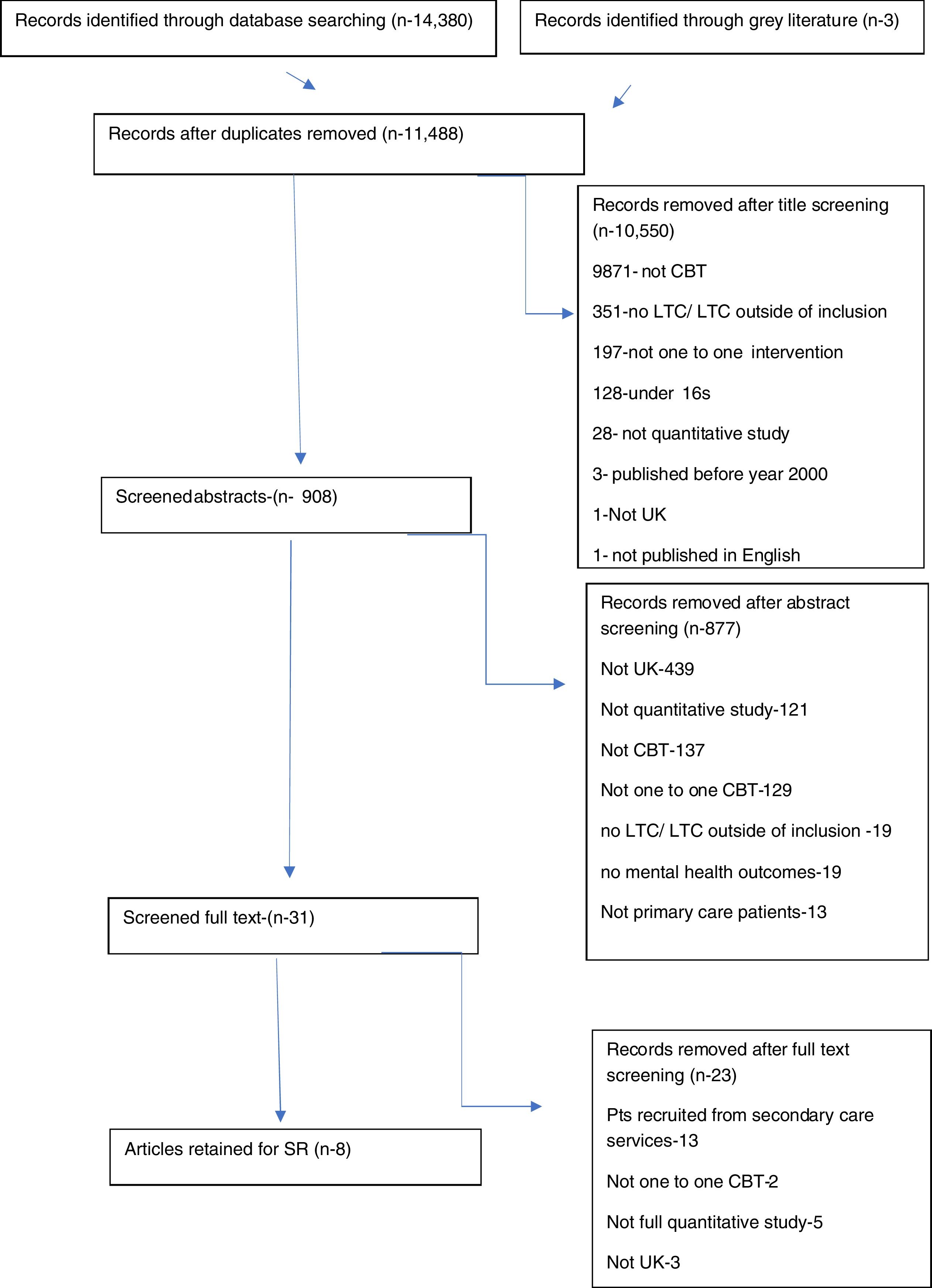
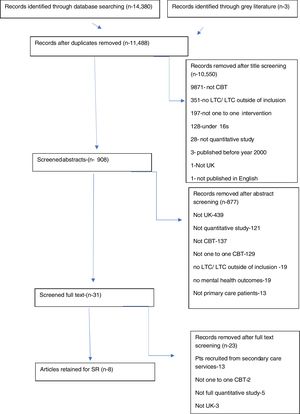
The flow of information throughout the phases of the SR was documented (Fig. 1). Title and abstract screening were completed by the primary reviewer and full texts were double screened. Discrepancies were resolved by a third reviewer and studies were included following a mutual agreement.
Flow chart for search and identification of relevant research, PRISMA flowchart (Moher, 2009).
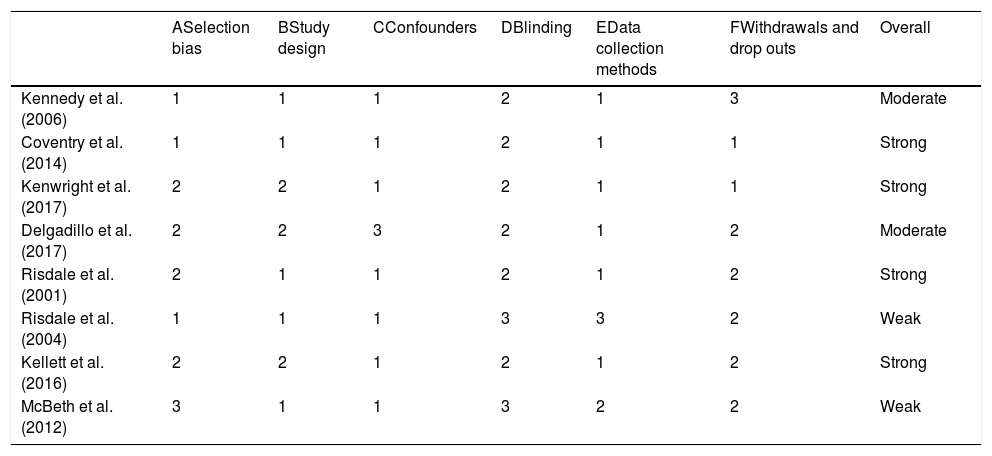
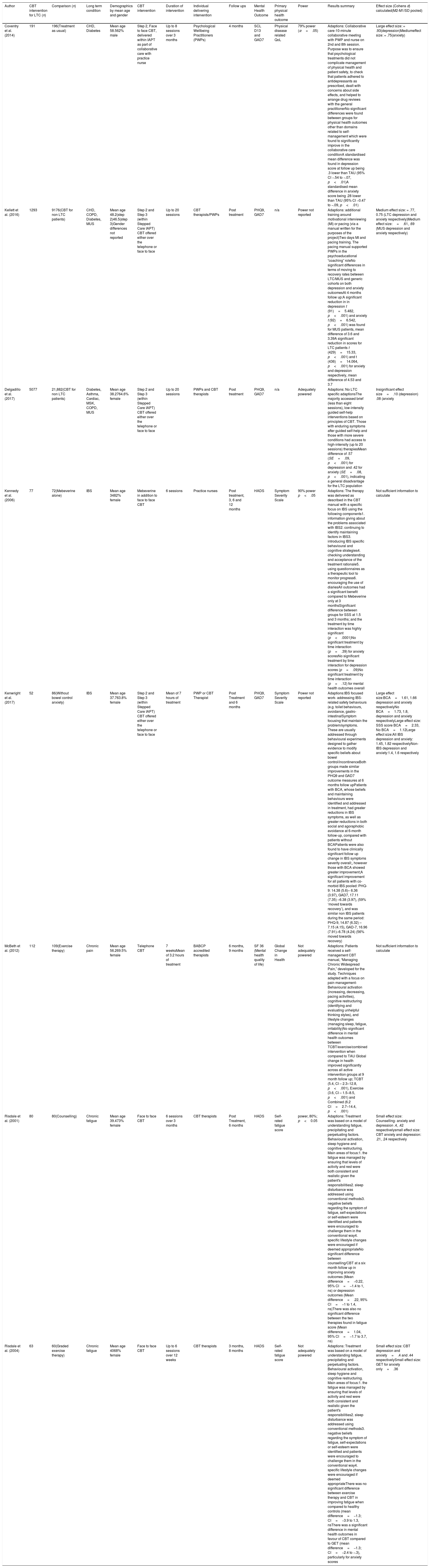
Data was extracted by two independent reviewers based upon the PICO for the review using a standardised data extraction form (Appendix B). See Table 2 for extracted data including standardised difference in mean scores and calculated effect sizes. Quality assessments were made using the effective public health practice project (EPHPP) tool which was developed for the purpose of SRs addressing public health interventions (Thomas, Ciliska, Dobbins, & Micucci, 2004) and holds applicability to designs other than randomised control trials (RCTs) (Armijo-Olivo, Stiles, Hagen, Biondo, & Cummings, 2012). The quality of the studies was rated as weak, moderate or strong by two reviewers. A third reviewer was required to quality assess one publication due to discrepancies between the original reviewers. The quality assessment ratings indicate that, overall, four were rated as methodologically strong, two as moderate and two as weak. The ratings for each study, broken down by category, can be seen in Table 1.
EPHPP ratings by category.
| ASelection bias | BStudy design | CConfounders | DBlinding | EData collection methods | FWithdrawals and drop outs | Overall | |
|---|---|---|---|---|---|---|---|
| Kennedy et al. (2006) | 1 | 1 | 1 | 2 | 1 | 3 | Moderate |
| Coventry et al. (2014) | 1 | 1 | 1 | 2 | 1 | 1 | Strong |
| Kenwright et al. (2017) | 2 | 2 | 1 | 2 | 1 | 1 | Strong |
| Delgadillo et al. (2017) | 2 | 2 | 3 | 2 | 1 | 2 | Moderate |
| Risdale et al. (2001) | 2 | 1 | 1 | 2 | 1 | 2 | Strong |
| Risdale et al. (2004) | 1 | 1 | 1 | 3 | 3 | 2 | Weak |
| Kellett et al. (2016) | 2 | 2 | 1 | 2 | 1 | 2 | Strong |
| McBeth et al. (2012) | 3 | 1 | 1 | 3 | 2 | 2 | Weak |
Note. 1, strong; 2, moderate; 3, weak.
Synthesis of the results for the purpose of meta-analysis was not possible due to heterogeneity across studies (Eysenck, 1995). As such, a narrative synthesis approach was used through structuring the results based on the quality of the research, the PRISM checklist was utilised and guidance provided by the Cochrane Reviewers and Communication Review Group was taken into account (Ryan, 2013).
ResultsThe searches produced a total of 14,380 titles across the databases, three additional papers were identified through hand searching. Fig. 1 provides exclusion details at each stage of the screening process through the Prisma Flowchart.
EPHPP quality assessmentThe observational cohort studies utilised patient records from patients seeking support from primary care services which produced moderate quality for selection bias. All RCTs had recruited patients on a large scale from multiple GP practices across localities, however one of the studies had low take up rates from those identified as eligible. Two studies compared CBT to usual care which makes it difficult for valid inferences to be made about the specific functions of the intervention in improving outcomes (Wampold, 2001). Future studies should aim to replicate the use of electronic registers to as best comprehensively identify those with LTCs/MUS over multiple GP practice locations and use active control groups by comparison.
Quality assessment around blinding is more appropriate for RCTs; there is a need for patients to be aware of the purpose of the study in order for engagement and consent to be given when research is conducted into the effectiveness of psychological interventions. Within observational cohort studies, the referral process into psychological therapy does not allow blinding to take place which may therefore artificially reduce the overall quality rating of these studies.
Study characteristicsOut of the eight studies, five of the papers were RCTs and three were observational cohort studies. Three included patients with more than one LTC/MUS however, the remaining five focused on one MUS including IBS, chronic pain or CFS.
Sample sizes and comparison groups can be seen within Table 2, alongside details around how the CBT interventions were delivered within each study and adaptions made. Seven out of the eight studies reported baseline characteristics by gender; with six of these showing predominantly female sample (63.7–84.7%). All of the studies reported a mean age of their samples ranging from 33.8 to 57.9, only three of the studies reported around ethnicity which indicated a predominantly white British background (70.8–92%). Three of the studies reported on employment status, with a minority being unemployed or long-term sick (8.9–40%). Three were observational cohort studies using data obtained from IAPT services and the five RCTs recruited their participants through GP practices. The studies varied in location throughout the UK including London, South East of England, North Midlands and North of England/Aberdeen.
Main characteristics of studies.
| Author | CBT intervention for LTC (n) | Comparison (n) | Long term condition | Demographics by mean age and gender | CBT intervention | Duration of intervention | Individual delivering intervention | Follow ups | Mental Health Outcome | Primary physical health outcome | Power | Results summary | Effect size (Cohens d) calculated(M2-M1/SD pooled) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coventry et al. (2014) | 191 | 196(Treatment as usual) | CHD, Diabetes | Mean age 58.562% male | Step 2, Face to face CBT, delivered within IAPT as part of collaborative care with practice nurse | Up to 8 sessions over 3 months | Psychological Wellbeing Practitioners (PWPs) | 4 months | SCL D13 and GAD7 | Physical disease related QoL | 79% power (α=.05) | Adaptions: Collaborative care-10-minute collaborative meeting with PWP and nurse on 2nd and 8th session. Purpose was to ensure that psychological treatments did not complicate management of physical health and patient safety, to check that patients adhered to antidepressants as prescribed, dealt with concerns about side effects, and helped to arrange drug reviews with the general practitionerNo significant differences were found between groups for physical health outcomes other than domains related to self-management which were found to significantly improve in the collaborative care conditionA standardised mean difference was found in depression score at follow up being .3 lower than TAU (95% CI −.54 to −.07, p<.01)A standardised mean difference in anxiety score being .28 lower than TAU (95% CI −0.47 to −.09, p<.01) | Large effect size: = .93(depression)Mediumeffect size: = .75(anxiety) |
| Kellett et al. (2016) | 1293 | 9176(CBT for non LTC patients) | CHD, COPD, Diabetes, MUS | Mean age 48.2(step 2)46.5(step 3)Gender differences not reported | Step 2 and Step 3 (within Stepped Care IAPT) CBT offered either over the telephone or face to face | Up to 20 sessions | CBT therapists/PWPs | Post treatment | PHQ9, GAD7 | n/a | Power not reported | Adaptions: additional training around motivational interviewing (MI) or pacing (via a manual written for the purposes of the project)Two days MI and pacing training. The pacing manual supported PWPs in the psychoeducational “coaching” roleNo significant differences in terms of moving to recovery rates between LTC/MUS and generic cohorts on both depression and anxiety outcomesAt 4 months follow up:A significant reduction in in depression t (91)=5.482, p<.001) and anxiety t (92)=6.542, p<.001) was found for MUS patients, mean difference of 3.6 and 3.39A significant reduction in scores for LTC patients t (429)=15.33, p<.001) and t (436)=14.064, p<.001) for anxiety and depression respectively, mean difference of 4.53 and 3.7 | Medium effect size: = .77, 0.75 (LTC depression and anxiety respectively)Medium effect size:=.61, .69 (MUS depression and anxiety respectively) |
| Delgadillo et al. (2017) | 5077 | 21,882(CBT for non LTC patients) | Diabetes, Asthma, Cardiac, MSK, COPD, MUS | Mean age 38.2764.6% female | Step 2 and Step 3 (within Stepped Care IAPT) CBT offered either over the telephone or face to face | Up to 20 sessions | PWPs and CBT therapists | Post treatment | PHQ9, GAD7 | n/a | Adequately powered | Adaptions: No LTC specific adaptionsThe majority accessed brief (less than eight sessions), low-intensity guided self-help interventions based on principles of CBT. Those with enduring symptoms after guided self-help and those with more severe conditions had access to high-intensity (up to 20 sessions) therapiesMean difference of .57 (SE=.09, p<.001) for depression and .42 for anxiety (SE=.08, p<.001), indicating a general disadvantage for the LTC population | Insignificant effect size=.10 (depression) .08 (anxiety |
| Kennedy et al. (2006) | 77 | 72(Mebeverine alone) | IBS | Mean age 3482% female | Mebeverine in addition to face to face CBT | 6 sessions | Practice nurses | Post treatment, 3, 6 and 12 months | HADS | Symptom Severity Scale | 90% power p<.05 | Adaptions: The therapy was delivered as described in the CBT manual with a specific focus on IBS using the following components1. information giving about the problems associated with IBS2. continuing to identify maintaining factors in IBS3. introducing IBS specific behavioural and cognitive strategies4. checking understanding and acceptance of the treatment rationale5. using questionnaires as a therapeutic tool to monitor progress6. encouraging the use of diariesAll outcomes had a significant benefit compared to Mebeverine only at 3 monthsSignificant difference between groups for SSS at 1.5 and 3 months; and the treatment by time interaction was highly significant (p<.0001)No significant treatment by time interaction (p=.39) for anxiety scoresNo significant treatment by time interaction for depression scores (p=.09)No significant treatment by time interaction (p=.12) for mental health outcomes overall | Not sufficient information to calculate |
| Kenwright et al. (2017) | 52 | 86(Without bowel control anxiety) | IBS | Mean age 37.763.8% female | Step 2 and Step 3 (within Stepped Care IAPT) CBT offered either over the telephone or face to face | Mean of 7 hours of treatment | PWP or CBT Therapist | Post Treatment and 6 months | PHQ9, GAD7 | Symptom Severity Scale | Power not reported | Adaptions:IBS focused work- addressing IBS-related safety behaviours (e.g. toilet behaviours, avoidance, gastro-intestinalSymptom focusing that maintain the problem/symptoms. These are usually addressed through behavioural experiments designed to gather evidence to modify specific beliefs about bowel control/incontinenceBoth groups made similar improvements in the PHQ9 and GAD7 outcome measures at 6 months follow upPatients with BCA, whose beliefs and maintaining behaviours were identified and addressed in treatment, had greater reductions in IBS symptoms, as well as greater reductions in both social and agoraphobic avoidance at 6-month follow-up, compared with patients without BCAPatients were also found to have clinically significant follow up change in IBS symptoms severity overall;, however those with BCA showed greater improvement;A significant improvement for all patients with co-morbid IBS pooled: PHQ-9: 14.38 (5.6)– 6.36 (3.97), GAD7, 17.11 (7.35) –6.38 (3.97), (59% ‘moved towards recovery’), and was similar non IBS patients during the same period: PHQ-9, 14.87 (6.32) –7.15 (4.15), GAD-7, 16.96 (7.91)–6.78 (4.24) (56% moved towards recovery) | Large effect size:BCA=1.61, 1.66 depression and anxiety respectivelyNo BCA=1.73, 1.8, depression and anxiety respectivelyLarge effect size: SSS score BCA=2.33, No BCA=1.12Large effect size:All IBS depression and anxiety: 1.45, 1.82 respectivelyNon-IBS depression and anxiety:1.4, 1.6 respectively |
| McBeth et al. (2012) | 112 | 109(Exercise therapy) | Chronic pain | Mean age 56.269.5% female | Telephone CBT | 7 weeksMean of 3.2 hours of treatment | BABCP accredited therapists | 6 months, 9 months | SF 36 (Mental health quality of life) | Global Change in Health | Not adequately powered | Adaptions: Patients received a self-management CBT manual, “Managing Chronic Widespread Pain,” developed for the study. Techniques adapted with a focus on pain management- Behavioural activation (increasing, decreasing, pacing activities), cognitive restructuring (identifying and evaluating unhelpful thinking styles), and lifestyle changes (managing sleep, fatigue, irritability)No significant difference in mental health outcomes between TCBT/exercise/combined intervention when compared to TAU Global change in health improved significantly across all active intervention groups at 9 month follow up; TCBT (5.4, CI – 2.3–12.8, p<.001), Exercise (3.6, CI – 1.5–8.5, p<.001) and Combined (6.2 CI=2.7–14.4, p<.001) | Not sufficient information to calculate |
| Risdale et al. (2001) | 80 | 80(Counselling) | Chronic fatigue | Mean age 39.473% female | Face to face CBT | 6 sessions over 3 months | CBT therapists | Post Treatment, 6 months | HADS | Self-rated fatigue score | power, 80%; p<0.05 | Adaptions: Treatment was based on a model of understanding fatigue, precipitating and perpetuating factors. Behavioural activation, sleep hygiene and cognitive restructuring. Main areas of focus:1. the fatigue was managed by ensuring that levels of activity and rest were both consistent and realistic given the patient's responsibilities2. sleep disturbance was addressed using conventional methods3. negative beliefs regarding the symptom of fatigue, self-expectations or self-esteem were identified and patients were encouraged to challenge them in the conventional way4. specific lifestyle changes were encouraged if deemed appropriateNo significant difference between counselling/CBT at a six month follow up in improving anxiety outcomes (Mean difference=−0.22, 95% CI=−1.4 to 1, ns) or depression outcomes (Mean difference=.22, 95% CI=−1 to 1.4, ns)There was also no significant difference between the two therapies found in fatigue score (Mean difference=1.04, 95% CI=−1.7 to 3.7, ns) | Small effect size: Counselling- anxiety and depression .4, .42 respectivelysmall effect size: CBT anxiety and depression: .21, .24 respectively |
| Risdale et al. (2004) | 63 | 60(Graded exercise therapy) | Chronic fatigue | Mean age 4068% female | Face to face CBT | Up to 6 sessions over 12 weeks | CBT therapists | 3 months, 8 months | HADS | Self-rated fatigue score | Not adequately powered | Adaptions: Treatment was based on a model of understanding fatigue, precipitating and perpetuating factors. Behavioural activation, sleep hygiene and cognitive restructuring. Main areas of focus:1. the fatigue was managed by ensuring that levels of activity and rest were both consistent and realistic given the patient's responsibilities2. sleep disturbance was addressed using conventional methods3. negative beliefs regarding the symptom of fatigue, self-expectations or self-esteem were identified and patients were encouraged to challenge them in the conventional way4. specific lifestyle changes were encouraged if deemed appropriateThere was no significant difference between exercise therapy and CBT in improving fatigue when compared to healthy controls (mean difference=−1.3; CI=−3.9 to 1.3, nsThere was a significant difference in mental health outcomes in favour of CBT compared to GET (mean difference=−1.3; CI=−2.4 to −.3), particularly for anxiety scores | Small effect size: CBT depression and anxiety=.4 and .44 respectivelySmall effect size: GET for anxiety only=.36 |
Only three out of the eight studies used high-quality methods to ensure fidelity of the intervention through the use of audiotapes which were reviewed either within supervision or by independent raters (Kennedy et al., 2006; McBeth et al., 2012; Risdale et al., 2001). Other methods included the use of CBT manuals (Coventry et al., 2015; Risdale, Darbishire, & Seed, 2004) and group supervision (Kellett et al., 2016). Delgadillo, Dawson, Gilbody, and Böhnke (2017) did not report on this methodology.
The baseline characteristics provided by most of the studies lack diversity through the inclusion of predominantly white British women, of working age. The samples may represent a patient group who are more likely to access psychological therapies and not the target population. However, the findings provided by Coventry et al. (2015) was the only piece of research that offered a predominantly male sample (56%) with 74% of the sample being moderately to heavily deprived, further offering insight into this subgroup.
Outcome measuresFour of the eight studies used either the Patient Health Questionnaire 9 (PHQ9) or the Generalised Anxiety Disorder 7 item scale (GAD7) for outcome measures of anxiety and depression. Three of the eight studies used the Hospital Anxiety and Depression scale to assess mental health outcomes. Out of the eight papers, six reported primary physical health outcomes (see Table 2.) Overall, six out of the eight papers reported high levels of validity and reliability for their outcome measures; one study failed to report on the validity/reliability of the Likert scale used to measure fatigue (Risdale et al., 2004) and another discussed the potential for loss of accuracy and reduction in power as a result of their physical health outcome measure used which was a self-rated, global health score (McBeth et al., 2012).
Results of individual studies based upon CBT adaptionsFive out of the eight studies adapted the CBT intervention through utilising materials specific to the patients’ condition and exploring their mental health presentation within the context of their MUS (Kennedy et al., 2006; Kenwright, McDonald, Talbot, & Janjua, 2017; McBeth et al., 2012; Risdale et al., 2001, 2004). Two studies made adaptions through incorporating a collaborative care element to the intervention (Coventry et al., 2015), or providing additional training for practitioners around motivational interviewing (MI), acceptance and commitment therapy (ACT) and pacing techniques (Kellett et al., 2016). One study did not make any adaptions to the intervention and compared the effectiveness of routine CBT for those with LTCs to healthy controls (Delgadillo et al., 2017). Results of individual studies are presented in Table 2, and are discussed below in relation to the methodological strength of the evidence.
Specific focus on MUSFive studies adapted CBT interventions for patients with MUS; through exploring the mental health presentation in the context of their condition. Two of the studies explored CBT for chronic fatigue (Risdale et al., 2001, 2004), two for IBS (Kennedy et al., 2006; Kenwright et al., 2017) and one for chronic pain (McBeth et al., 2012). The studies were mixed in terms of their findings and methodological quality.
Strong evidenceTwo studies were rated as strong methodologically (Kenwright et al., 2017; Risdale et al., 2001). Kenwright et al. (2017) utilised an active control group, through a comparison group of CBT for non-LTC populations within IAPT services. The results provide strong evidence to indicate that CBT is as effective for LTC patients than non-LTC patients with the specific targeting of bowl control anxiety (BCA) for patients with IBS (Kenwright et al., 2017). These results were also sustained at a six-month follow-up, providing evidence to show no significant difference in outcomes between LTC and non-LTC groups when this adaption to the intervention is made (Kenwright et al., 2017) with large effect sizes found.
Significant improvements in physical health outcomes were found through IBS symptom severity, with the largest effect size found when targeting BCA compared to generalised anxiety. This also provides good evidence for improved outcomes for physical symptoms when the nature of the intervention is adapted to target health specific cognitions and behaviours. It was found that 79% of BCA patients were treated with HI interventions and although this group showed the most improved outcomes, there was no significant difference in intervention length between LI and HI interventions. This further indicates that it may be the more appropriately targeted interventions which account for improved outcomes and the longevity of the intervention does not necessarily predict better outcomes (Kenwright et al., 2017).
Risdale et al. (2001) compared the effectiveness of LI CBT to counselling for patients with CFS. The CBT intervention was adapted so that the patient was supported to understand precipitating and perpetuating factors contributing to their fatigue. Treatment had a specific focus on challenging unhelpful cognitions around their fatigue and supporting them to better pace activities to manage their symptoms. Both interventions were found to equally improve outcomes for patients at six-month follow up with small effect sizes. The use of antidepressant medication was recorded at baseline and no difference between intervention groups were found. Risdale et al. (2001) also had the strongest study design with the fidelity of the interventions being measured through the use of audio tapes which were reviewed by independent raters; further enhancing the validity of the results.
Both studies provide strong evidence to suggest that when the patient's MUS is placed at the centre of the formulation and treatment plan, mental health outcomes are found to significantly improve, equal to that of those without LTCs or those with LTCs receiving alternative therapies. It is important to consider that counselling is currently not offered as part of LI therapy within IAPT services (Haake, 2017) as this was found to be equally effective at improving outcomes. Further research should aim to replicate and bring research up to date. These findings cannot be generalised to a range of LTCs due to the current research around MUS only.
Moderate evidenceA trial was conducted by Kennedy et al. (2006), comparing CBT plus medication to medication alone (Mebeverine Hydrochloride) for patients with IBS. The intervention was adapted for patients through information giving about problems associated with IBS, identifying maintenance factors in IBS and introducing IBS specific behavioural and cognitive strategies. Moderate quality evidence found that LI-CBT interventions (6–8 sessions) significantly improved mental and physical health outcomes at follow-up times of three months compared to medication alone when CBT was delivered by practice nurses.
The study remained adequately powered, despite its high dropout/withdrawal rate, however insufficient data was reported to calculate effect sizes of the improved outcomes. No significant improvement in mental or physical health outcomes was found over a twelve-month follow-up period, other than one variable around the impact of living with IBS. The treatment as usual comparison group weakens the quality of the research as it cannot be inferred that the intrinsic components of the CBT intervention predicted improved outcomes at three months. The reduced outcomes at twelve months may therefore be due to the loss of therapeutic effect. The intervention was delivered by practice nurses who had attended a twelve-day training course with no previous experience of CBT; this indicates the need for future research to identify long term outcomes mental health professionals are delivering an intervention in comparison to an active control group. Kennedy et al. (2006) provide moderate evidence to suggest that CBT interventions that are specifically adapted for IBS patients can improve mental health outcomes through LI CBT interventions, only in the short-term.
Weak evidenceTwo studies within the review were rated as weak methodologically; both of which examined the effectiveness of LI-CBT in improving mental and physical health outcomes compared to graded exercise therapy (GET) for patients with MUS (McBeth et al., 2012; Risdale et al., 2004). Both studies adapted their interventions to place the condition at the centre of the interventions. McBeth et al. (2012) developed a workbook ‘Managing Chronic Widespread Pain’ with behavioural and cognitive techniques adapted to focus on pain management. Risdale et al. (2004) ensured patients understood their difficulties based on a model of understanding fatigue and precipitating/perpetuating factors.
Risdale et al. (2004) found an improvement in anxiety levels for CBT in comparison to an exercise group for patients with CFS, however McBeth et al. (2012) found no significant difference in mental health scores between telephone CBT compared to GET. Physical health outcomes improved significantly across all active intervention groups for both studies. The results suggest that functional improvements may occur without the need for a change in cognitions which is targeted by CBT (Deale, Chalder, & Marks, 1997), however the calculated effect sizes were small (Risdale et al., 2004) or not enough information was provided to calculate (McBeth et al., 2012). Both studies were also under powered to demonstrate equivalence of CBT and GET.
Both studies lacked strength methodologically due to data selection bias with an uptake of less than 60% (McBeth et al., 2012) or failure to describe the validity or reliability of the data collection tools used (Risdale et al., 2001). Furthermore, both trials demonstrated a lack of blinding. The weak methodology, lack of power and lack of/small effect sizes prevent valid conclusions being drawn from these findings and future RCTs should aim to strengthen these areas of the research.
Overall, the findings from moderate/high quality studies have found initial support to show that adapted interventions with a specific focus on the patients MUS improve mental health outcomes in the short term. However, future research should aim to provide long term follow ups and conclusions remain tentative.
Collaborative careCoventry et al. (2015) provides strong evidence to show that LI-CBT interventions (eight sessions) with the inclusion of two joint appointments with practice nurses (collaborative care) significantly improved mental health outcomes for patients with LTCs. The purpose of the joint appointments was to ensure that psychological treatments did not complicate management of physical health and patient safety, to check that patients adhered to antidepressants as prescribed, to deal with concerns about side effects, and help to arrange drug reviews with the general practitioner. The research had a comparison group of usual care, which was defined as GP support, prescription of antidepressants or standard referrals to IAPT services. Improved mental health outcomes were found for the collaborative care group at follow-up times of four months with large effect sizes for depression outcomes and medium for anxiety outcomes (see Table 1). Baseline characteristics identified that half of the sample were taking psychotropic medication. The results indicated that collaborative care with psychological therapy with or without drugs was more effective than usual care; further strengthening the findings. Significant improvements in physical health outcomes relating to self-management were also found.
The type of support received within the usual care group was not recorded, therefore it is unclear as to what proportion of this group received an active intervention within IAPT. Future research should aim to clarify control groups for valid inferences to be made (Wampold, 2001). In addition to this, the short follow-up period of 4 months, makes it unclear as to whether outcomes would remain improved in the long term. The findings from this research provide initial evidence to show that LTC-IAPT services can make adaptions to support working with this population through working collaboratively with multi-disciplinary colleagues.
Additional trainingA study conducted by Kellett et al. (2016) examined the effectiveness of CBT for patients with coronary heart disease (CHD), COPD, diabetes and MUS. The study utilised an active control group of healthy controls accessing CBT within IAPT services. Adaptions to the intervention included the use of MI, pacing and ACT through additional training given to practitioners in these techniques (Kellett et al., 2016). The results provide strong evidence to indicate that CBT is as effective for LTC patients than non-LTC patients when these adaptions are made to the intervention.
The effectiveness of the intervention based on treatment intensity found no significant difference in ‘moving to recovery rates’ for depression between LI (31.67%) or HI (32.23%) interventions (Kellett et al., 2016). The results from this study indicate that IAPT services are capable of adapting CBT interventions to support the needs of LTC/MUS patients through providing additional training to staff with a moderate effect size found. The results also identify that no significant difference was found between LI and HI CBT outcomes, (Kellett et al., 2016) further suggesting that effective treatment can be provided over short periods of time and at a reduced cost to services.
No adaptionsDelgadillo et al. (2017) conducted a naturalistic cohort study and provided moderate evidence to indicate standard CBT interventions within IAPT services are insufficient to support patients with multimorbidity. Significantly worse mental health outcomes post therapy was found for patients with a range of LTCs and MUS compared to non-LTC patients when receiving ‘routinely delivered psychological care.’ Over a third of LTC/MUS patients showed reliable improvement in mental health outcomes, which is below the national target and those accessing HI interventions were associated with significantly worse, post treatment outcomes for patients living with COPD and diabetes. It is of note that reliable improvement was associated with receiving an LI intervention, further suggesting that LI-CBT can be somewhat effective in improving outcomes in absence of any adaptions.
The use of psychotropic medication was recorded at baseline, with findings suggesting no significant difference in outcomes dependant on medication use. The researchers do not describe important differences between LTC and non-LTC groups at baseline, however it is stated that potentially confounding variables are controlled for within the seemingly unrelated regressions (SUR) model, resulting in a very small effect sizes (Cohen's d – .1 and .08) for depression and anxiety respectively. The naturalistic cohort design therefore impacted on the methodological quality of the study and research should aim to better report confounding variables between groups to better understand important differences.
Delgadillo et al. (2017) provides moderate evidence to suggest when CBT interventions are delivered in the absence of any appropriate adaptions, the results are less favourable compared to non-LTC patients.
DiscussionMain findingsOverall, the findings provide support for the service evaluation conducted by de Lusignan et al. (2013) who found that CBT improved mental health outcomes for those with LTCs and MUS within UK, primary care settings and contributes to the findings around particular adaptions needed when working with this population.
Moderate evidence suggests that those with an LTC/MUS have worse outcomes post intervention compared to healthy controls when CBT is delivered as ‘routine’ (Delgadillo et al., 2017). Strong evidence within three studies found a significant improvement in outcomes through the targeting of LTC specific anxiety symptoms (Kenwright et al., 2017), involvement of collaborative care with nurses (Coventry et al., 2015) and the inclusion of MI, pacing and ACT (Kellett et al., 2016). All three of the above studies which were rated strong methodologically had medium-large effect sizes. This highlights the importance of providing LTC specific training to place the LTC at the centre of the intervention, working collaboratively with health professionals involved in the patient's care, alongside enhancing skills through the teaching of complimentary therapeutic models.
Strong evidence was also provided by Risdale et al. (2001) suggesting that LI, talking therapies are generally effective in improving outcomes as no significant difference was found between counselling and CBT, however small effect sizes were found for both intervention groups. This is consistent with findings provided by Li et al. (2014) who found no significant difference in outcomes for CBT compared to other psychological interventions when delivered to patients with IBS outside of the UK. Research should aim to assess common factors as potential moderating factors within interventions for those with LTC/MUS, as choice of therapies potentially be driven by accessibility and cost.
It is of interest that the two papers with a focus of IBS within the review found moderate-strong evidence for CBT in improving mental health outcomes (Kennedy et al., 2006; Kenwright et al., 2017) when particular focus of the intervention is around IBS related cognitions and behaviours, including the targeting of bowel control anxiety. These findings are not consistent with a previous SR conducted outside of the UK who did not find any significant improvement in outcomes when CBT was delivered online for this population (Hanlon et al., 2018).
Methodological issues were largely identified across the studies in relation to study design and blinding. The most appropriate methodology came from RCTs that blinded research members and participants during the allocation and baseline assessment phases. There was a general lack of reporting around moderating factors which should be further explored within RCTs to identify mechanisms that lead to improved outcomes. Despite the lack of control associated with observational cohort studies, they are deemed appropriate pieces of research to consult in the field of psychological interventions. Studies followed up patients in the short term, with only one piece of research providing a 12-month follow up (Kennedy et al., 2006), not allowing meaningful conclusions to be drawn about the sustainability of improved outcomes. Out of the eight studies only three reported to be adequately powered (Delgadillo et al., 2017; Kennedy et al., 2006; Risdale et al., 2001) and only three of the eight studies ensured high levels of fidelity. Improving the quality of methodology alongside standardising the delivery of interventions, outcome measures and LTC/MUS populations would further support the use of a meta-analysis.
Only four of the studies had identified and reported around medication use within the outcomes (Coventry et al., 2015; Delgadillo et al., 2017; Kennedy et al., 2006; Risdale et al., 2001). This lack of reporting affects the reliability of the findings as medication use is likely to be high amongst samples with physical and mental health comorbidity and can further impact upon outcomes.
The eight studies were conducted in various locations across the country which supports the generalisability of the findings across the UK. However, the samples were predominantly white British women of working-class age who do not represent the target population; with 58% of those with LTCs/MUS being over the age of 60 and those amongst the poorest social class having a 60% higher prevalence of multimorbidity (DoH, 2012). Strong evidence was provided by Coventry et al. (2015) to show that CBT with collaborative care was effective for an older, predominantly male sample (mean age; 58.9) who were moderately-heavily deprived. However, there is a need for these results need to be replicated to improve generalisability.
Seven out of the eight studies utilised mental health practitioners to deliver the intervention, however Kennedy et al. (2006) utilised practice nurses with no prior CBT experience. This was also the only piece of research to include a twelve-month follow-up and found outcomes were not sustained. Future research could therefore identify if findings are replicated when interventions are delivered by trained IAPT staff.
Clinical implicationsIAPT services are increasingly becoming integrated into physical healthcare services with around a third of clinical commissioning groups increasing access to therapy for people with LTCs (Clark, 2019). The findings of the review provide initial support for the expansion of LTC-IAPT sites to provide appropriately adapted CBT interventions.
There is strong evidence that LI-CBT interventions that are appropriately adapted are effective at improving outcomes in the short term, which could be implemented at a reduced cost to the NHS with the need for a less qualified workforce. It is expected that a reduced number of LI practitioners will be recruited (30%), compared to standard IAPT services, (National Collaborating Centre for Mental Health, 2018). However, the current SR indicates a need for a greater number of LI staff, with LTC specific training to support working with complexity within brief interventions. This further supports the qualitative findings from McCrae, Correa, and Chan (2015) which highlighted training needs for IAPT workers in this specialist field and noted limited confidence amongst therapists when working with physical health.
Research implicationsFuture research should aim to compare the effectiveness of CBT interventions within LTC-IAPT services for specific conditions; as at present only a small amount of research is highlighting adaptions made for particular MUS which enables comparability. It is also important to identify if the outcomes are sustainable in the long term as most commonly studies followed up between four and eight months and initial evidence found outcomes are not sustainable after a twelve-month period (Kennedy et al., 2006). It is important to further explore this due to the lifelong nature of LTCs, and the potential gain for the individual and the NHS.
LimitationsMany of the papers were completed within IAPT services with a range of interventions including EMDR, interpersonal therapy, counselling and mindfulness being offered as HI interventions (Delgadillo et al., 2017; Kellett et al., 2016; Kenwright et al., 2017). The results did not offer a comparison of outcomes across interventions which makes it difficult to make inferences about the effectiveness of HI-CBT specifically.
Studies were excluded if they were published before the year 2000 as NICE guidelines that were introduced within this decade alongside studies conducted outside of the UK which may both hold value in their applicability to primary care settings. Therefore, relevant studies may have been excluded from the review due to the strict inclusion criteria. The breadth of conditions listed within the search terms generated large amount of studies to be reviewed, which ensured a comprehensive search of literature within these inclusions. A narrative synthesis was adopted due to the methodological heterogeneity of studies within the review; however, this holds challenges in maintaining transparency around the interpretation of data and conclusions drawn (Campbell, Katikireddi, Sowden, & Thomson, 2019). To improve transparency, effect sizes from all studies are reported within Table 2 and it is acknowledged that some studies do not provide enough information to calculate effects sizes (McBeth et al., 2012; Kennedy et al., 2006). The review also examined the evidence for CBT amongst two populations (MUS and LTCs) which may have impacted on the specificity of the findings, and due to the heterogeneity, it is not possible to compare and contrast the findings between conditions.
ConclusionsMethodological quality of studies were mixed, however there is preliminary evidence for the implementation of CBT within LTC-IAPT to improve outcomes. Recommended adaptions include the specific focus of the condition within the intervention, the use of complementary therapeutic models and working collaboratively with health professionals. However future research should aim to strengthen and replicate these findings across a range of LTCs and MUS as conclusions remain tentative.
Conflict of interestThe primary author is employed by the National Health Service and works within primary mental health care.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.