Intracardiac thrombosis is a rare manifestation of cardiac involvement in Behçet's disease, and it may be mistaken for a heart tumor. In this letter we present the case of a patient diagnosed with Behçet's disease who was incidentally found to have a mass in the right atrium suspicious of a cardiac tumor. Nevertheless, cardiac magnetic resonance showed a cardiac thrombus. Immunosuppressive therapy and anticoagulation were effective for thrombus resolution.
La trombosis intracardiaca es una manifestación muy rara del compromiso cardiaco en la enfermedad de Behçet, la cual puede confundirse con una masa tumoral. Se presenta el caso de una paciente con esta enfermedad a quien de manera incidental se le detectó una masa intraauricular derecha sugestiva de tumor intracardiaco. Sin embargo los hallazgos de la resonancia magnética cardiaca fueron los de un trombo intracavitario que se resolvió con tratamiento inmunosupresor y terapia anticoagulante.
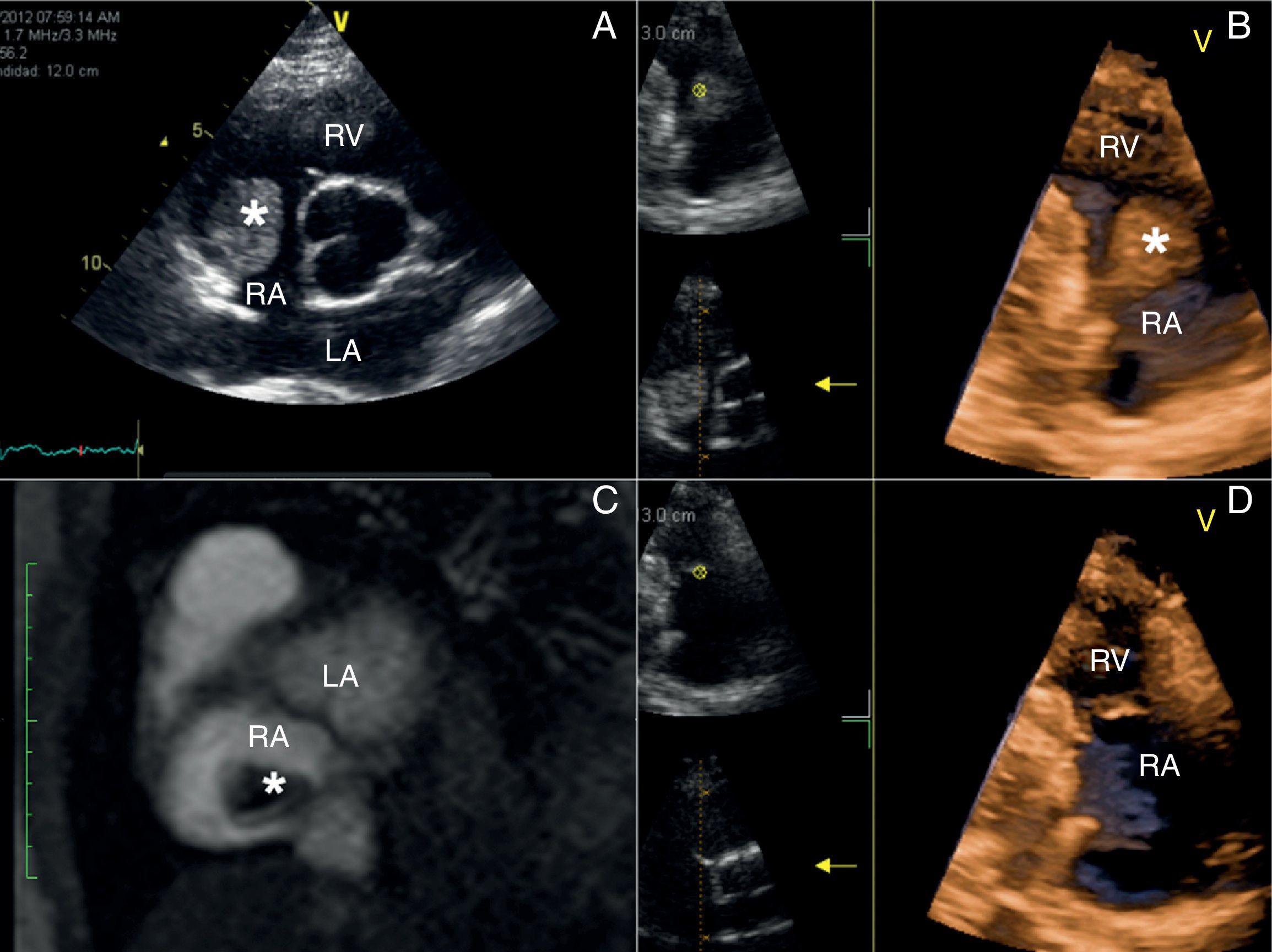
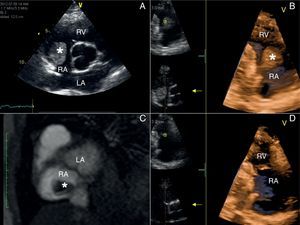
A 51 year-old woman with Behçet's syndrome developed a spontaneous Staphylococcus aureus bacteremia and prolonged fever, which prompted us to perform an echocardiogram in order to rule out infectious endocarditis. No valvular or mural vegetations were noticed on transthoracic (2D and 3D images) or transesophageal echocardiography. However, a round shaped mobile mass with a stalk attached to the posterior wall of the right atrium (Fig. 1A and B) was evident, and raised the possibility of a cardiac tumor. But, as another filiform mobile image was visible in the superior vena cava (not shown), such possibility was questioned, and the patient was anticoagulated and underwent a cardiac magnetic resonance imaging (CMR) for characterizing the pseudotumor. The pregadolinium gradient echo-CMR revealed low signal intensity in the tumor and the contrast-enhanced scan showed lack of enhancement of the tumor mass (Fig. 1C) favoring the diagnosis of a thrombus. Concurrently, a computed pulmonary angiography ruled out both embolism and aneurisms. The fever subsided and the patient's status improved over the days, and then she was discharged on anticoagulant therapy with warfarin. On a new transthoracic echocardiogram, performed 6 months later (Fig. 1D), there was no evidence of the thrombus previously seen in the right atrium, so warfarin was withheld. She has remained stable one year later without symptoms of thrombus recurrence.
(A) Two-dimensional echocardiography: parasternal short axis view showing a mass (asterisk) on the posterior wall of the right atrium (RA). (B) Three-dimensional echocardiography: right ventricle (RV) inflow tract view displaying a round shaped mass (asterisk) with a stalk attached to the posterior wall of the RA. (C) Delayed-enhancement cardiovascular magnetic resonance demonstrating the lack of gadolinium contrast uptake (asterisk) as the thombus is avascular. (D) Three-dimensional echocardiography: normal RV inflow tract view without evidence of thrombus after sixth months of anticoagulation therapy. LA: left atrium.
In one of the largest case series published so far, 52 (6%) patients from a cohort of 807 patients with Behçet's disease (BD) had some form of cardiac involvement including pericarditis, endocarditis, myocardial infarction, endomyocardial fibrosis, and aneurysms of the coronary arteries of sinus of Valsalva.1 However, intracardiac thrombosis is a rare finding with only 32 cases reported in the medical literature.1 In an analysis of 25 patients, 56% of them had clinical manifestations like fever, hemoptysis, dyspnea, and cough.2 Cardiac thrombi affected most often the right side (right ventricle, 52%; right atrium, 24%) and were unusual in the left or both chambers (4 and 16% of cases, respectively). Besides, intracardiac thrombi were also associated with thrombosis of the vena cava and pulmonary embolism (28 and 60% of cases, respectively).1,2 The echocardiographic appearance of thrombi may suggest a tumor, and several patients have undergone cardiac surgery but histological examination demonstrated thrombi in all cases.2 CMR is a useful technique for the differential diagnosis between cardiac thrombus and tumor and might be helpful in difficult cases like the one presented here.3 There is no consensus about the optimal treatment of intracardiac thrombosis in BD. Most patients receive immunosuppressive therapy (usually steroids in combination with azathioprine or cyclophosphamide) along with anticoagulation but some have reported the thrombi resolution only with immunosuppression particularly when hemoptysis or pulmonary artery aneurysms preclude the use of anticoagulants.2,4 Complete remission of intracardiac thrombosis has occurred in 75% of cases with corticosteroids and anticoagulation. Even though surgical resection seems an option when thrombi persist despite optimal medical therapy,1 the risk of recurrence and death is an issue.2,5 Finally, although the 5-year survival rate is lower in BD patients with heart involvement (84% vs. 96% in patients without cardiac lesions),1 the type of affectation is heterogeneous and prognosis differs accordingly. Notwithstanding, except for the risk of pulmonary embolism, the long-term prognosis of BD patients with intracardiac thrombi seems to be good as long as they receive only medical management.
Financial supportNone.
Conflict of interestThe authors declare that they have no conflict of interest.