Nowadays, most patients with non-valvular atrial fibrillation (NVAF) patients, receive long-term anticoagulation for prevention of stroke or systemic embolism.1,2 It is important to consider that many of them are elderly and frail patients who may have an increased risk of bleeding.3,4 The use of any anticoagulants increase the risk of bleeding, especially gastrointestinal (GI) bleeding.5,6 Interestingly, direct oral anticoagulants (DOACs) have shown lower risk of major bleeding, compared with traditional vitamin K antagonists (VKA).7 When a GI bleeding appears in subjects under anticoagulation, our first reaction is to consider it as a complication or an adverse effect of anticoagulants. Herein we report four patients in which a lower GI bleeding under DOACs unmasked intestinal disease leading to proper treatment that ultimately permitted the continuation of DOAC.
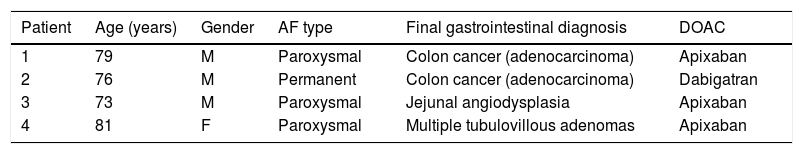
We present the clinical characteristics of the four patients (Table 1) (males=3), under anticoagulation because of NVAF, either paroxysmal (n=3) or chronic, all the patients were older than 70 years, and had not received any previous oral anticoagulation. They presented lower GI bleeding between 1 and 6 months after the start of DOAC treatment, manifested by hematochezia. Only one patient had major bleeding requiring red blood cell transfusion (3 concentrates; 1500mL). All were submitted to upper GI endoscopy and colonoscopy. One case needed a capsule endoscopy, because diagnosis was not obtained after conventional endoscopies. In two cases a colon malignancy was detected and surgical resection was performed without complications; specimen biopsies confirmed the diagnosis of adenocarcinoma. Patient 1 required a left hemicolectomy for a tumor localized at the splenic angle; he received chemotherapy with FOLFOX (Folinic acid, fluorouracil [5-FU], oxaliplatin) and Vectivix (panitumumab); after a two-year follow-up he is free from cancer. Patient 2 developed unexplained anemia, fecal occult blood test was positive, colonoscopy revealed a sigmoid colon neoplasia and a left hemicolectomy was performed. Pathology revealed a localized invasive adenocarcinoma and no further therapy was needed. In case 3 the diagnosis of jejunum angiodysplasia was established with a capsule endoscopy. The female patient had several tubulovillous adenomas; the smaller were resected in the same procedure and the largest, in a second colonoscopy.
Demographic and clinical characteristics of patients with intestinal bleeding associated with direct oral anticoagulants.
| Patient | Age (years) | Gender | AF type | Final gastrointestinal diagnosis | DOAC |
|---|---|---|---|---|---|
| 1 | 79 | M | Paroxysmal | Colon cancer (adenocarcinoma) | Apixaban |
| 2 | 76 | M | Permanent | Colon cancer (adenocarcinoma) | Dabigatran |
| 3 | 73 | M | Paroxysmal | Jejunal angiodysplasia | Apixaban |
| 4 | 81 | F | Paroxysmal | Multiple tubulovillous adenomas | Apixaban |
Occult bleeding has been reported since the beginning of anticoagulant use.8 Clemens et al. first report on the fact that the higher incidence of GI bleeding with the DOACs may also be related to pre-existing malignancies.9 They reported the incidence of GI bleeding with DOACs, compared with warfarin: dabigatran 110mg bid 1.42% versus 1.37%, dabigatran 150mg bid 1.93% versus 1.37%, rivaroxaban 3.52% versus 2.68%, and apixaban 1.93% versus 1.59%. The incidence of GI bleeding cancer related was similar between analyzed DOACs (D110 [0.79%], D150 [0.61%], rivaroxaban [0.83%], and apixaban [0.69%]), interestingly, numerically higher compared with warfarin (0.37%; 0.73%; 0.57%, respectively). Their conclusion that anticoagulant-related GI bleeding may unmask pre-existing malignancies leading to increased detection of GI cancer is similar to what Michaels wrote in 1962: “The probability of uncovering an occult malignancy in a patient with bleeding manifestations during anticoagulants is small. Since the chances of obtaining a cure of cancer depend in part upon early diagnosis, it behoves physicians to follow all possible leads”. We want to stress their conclusion with our two cases of adenocarcinoma. Physicians must be aware of the risk of GI bleeding with DOACs use and look for occult GI bleeding intentionally. Taking into consideration the high prevalence of GI bleeding it could be a good practice to test for occult bleeding before and after start of DOAC treatment.