Mexico has been positioned as the country with the highest mortality attributed to myocardial infarction among the members of the Organization for Economic Cooperation and Development. This rate responds to multiple factors, including a low rate of reperfusion therapy and the absence of a coordinated system of care. Primary angioplasty is the reperfusion method recommended by the guidelines, but requires multiple conditions that are not reached at all times. Early pharmacological reperfusion of the culprit coronary artery and early coronary angiography (pharmacoinvasive strategy) can be the solution to the logistical problem that primary angioplasty rises. Several studies have demonstrated pharmacoinvasive strategy as effective and safe as primary angioplasty ST-elevation myocardial infarction, which is postulated as the choice to follow in communities where access to PPCI is limited. The Mexico City Government together with the National Institute of Cardiology have developed a pharmaco-invasive reperfusion treatment program to ensure effective and timely reperfusion in STEMI. The model comprises a network of care at all three levels of health, including a system for early pharmacological reperfusion in primary care centers, a digital telemedicine system, an inter-hospital transport network to ensure primary angioplasty or early percutaneous coronary intervention after fibrinolysis and a training program with certification of the health care personal. This program intends to reduce morbidity and mortality associated with myocardial infarction.
México se ha posicionado como el país con mayor mortalidad atribuible al infarto del miocardio entre los países de la Organización de Cooperación y Desarrollo Económico. Esta tasa responde a múltiples factores, incluyendo una baja tasa de reperfusión y la ausencia de un sistema único y coordinado para la atención del infarto. Aun cuando la angioplastia es el método de reperfusión recomendado, requiere un sistema coordinado con personal entrenado y recursos materiales, condiciones que no siempre pueden ser alcanzadas. La reperfusión farmacológica temprana, seguida de angiografía coronaria temprana (estrategia farmacoinvasiva) es la solución al problema logístico que representa la angioplastia primaria. Múltiples estudios han demostrado que la estrategia farmacoinvasiva es tan segura y efectiva como la angioplastia primaria en el infarto agudo del miocardio con elevación del segmento ST, y se plantea como la estrategia de elección en comunidades donde el acceso a angioplastia está limitado por factores económicos, geográficos o socioculturales.
El gobierno de la Ciudad de México en conjunto con el Instituto Nacional de Cardiología ha desarrollado un programa de estrategia farmacoinvasiva para asegurar la reperfusión temprana en el infarto del miocardio. El modelo comprende una red de atención en los 3 niveles, incluyendo un sistema de reperfusión farmacológica en centros de primer contacto, transferencia de electrocardiogramas mediante telemedicina entre el primer nivel y el Instituto Nacional de Cardiología, una red de transporte interhospitalario y un programa de entrenamiento y educación continua. El objetivo de este programa es reducir la morbilidad y la mortalidad asociadas al infarto del miocardio.
Heart disease is Mexico's leading cause of death according to data from the National Institute of Statistics, Geography and Informatics (INEGI), accounting for 18.8% of total deaths, of which, 59% are attributable to myocardial infarction.1 In several studies, reperfusion therapy (fibrinolysis and coronary angioplasty) has consistently demonstrated a decrease in morbidity and mortality associated with myocardial infarction.2 RENASICA III study3 reported a reperfusion rate in Mexico of 52.6%, which correlates with our experience at the Coronary Care Unit of the National Institute of Cardiology.4
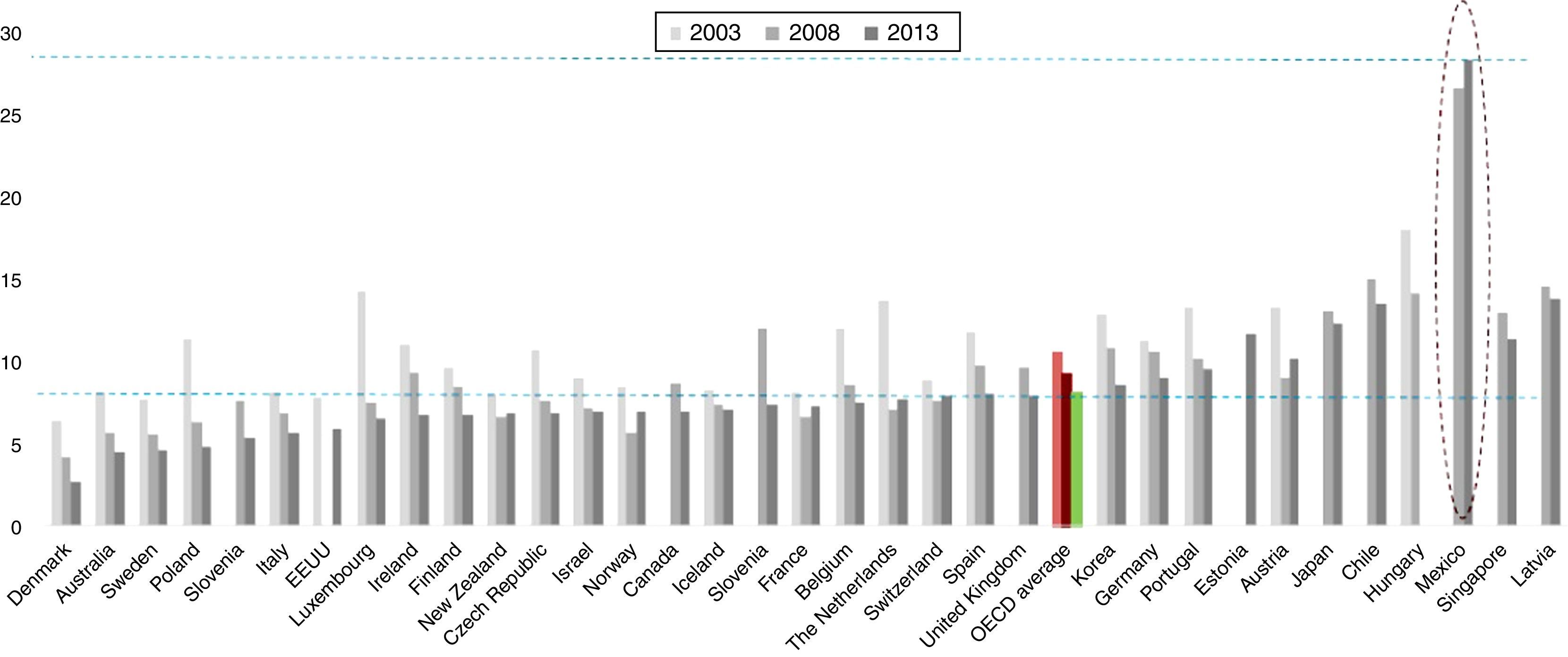
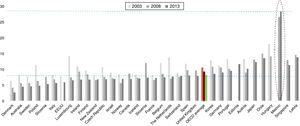
Mexico has been positioned as the country with the highest mortality attributed to myocardial infarction among the members of the Organization for Economic Cooperation and Development (OECD), with a rate of 27.2% compared to the average of 7.9%5 (Fig. 1). This high mortality rate responds to the low rate of reperfusion, the prolonged time for treatment initiation, the absence of a coordinated system of care between primary care physicians and the hospitals that are capable to perform coronary angioplasty, as well as the lack of trained personnel and resources for pharmacological reperfusion in the first level of health care. Based on these reports, one out of two patients with myocardial infarction does not receive any reperfusion therapy, and one out of four patients dies.
30-day myocardial infarction mortality in patients aged 45 and older. Reproduced from Ref. 5.
European guidelines for the treatment of ST-elevation myocardial infarction (STEMI) recommend primary angioplasty as the preferred reperfusion therapy provided it can be performed expeditiously (i.e. within guideline mandated times), by an experienced team and regardless of whether the patient presents to a primary percutaneous coronary intervention (PPCI) capable hospital.6 In equal conditions, PPCI has proven to be better than fibrinolysis, mainly in the rate of reinfarction and recurrent ischemia7; however, it must be considered that in Keeley's meta-analysis8 this results where obtain only in experience centers and this study did not perform a routinary angiography after fibrinolytic therapy. In addition, adjunctive therapy of acute coronary syndromes did not include the use of potent antiplatelet agents such as clopidogrel, prasugrel or ticagrelor, as well as newer anti-thrombinic therapy such as enoxaparin or bivalirudin, which have shown to decrease negative cardiovascular outcomes, and are now part of the standard therapy.6
It must be emphasized that reperfusion with PPCI requires a coordinated system care and transport logistics which involves physicians, nursing staff, paramedic personnel and material resources; conditions that even in first world countries are not reached at all times.9
In the 2002 CAPTIM trial,10 total ischemic time (or time to reperfusion) was identified as a crucial factor in the benefit obtained by reperfusion when comparing PPCI versus fibrinolysis. While the CAPTIM trial failed to show a benefit in mortality for patients who were reperfused by prehospital fibrinolysis versus those taken to PPCI, the results of a subsequent sub-analysis11 demonstrated that patients reperfused with very early fibrinolysis (<2h) had a strong tendency to decrease mortality versus PPCI. Since its publication, this study has suggested that early pharmacological reperfusion of the culprit coronary artery and then a routine invasive strategy (coronary angiography) to assess coronary anatomy and ensure vessel patency can be the solution to the logistical problem that PPCI raises.
Pharmaco-invasive reperfusion strategyIn 2003, Daureman and Sobel were the first to describe a combined approach that could exploit the widespread availability of fibrinolysis and its early administration, to restore at least some degree of myocardial blood flow, coupled with the complete restoration of the culprit coronary artery that can be obtained with subsequent angioplasty. They called this strategy “pharmaco-invasive recanalization” and they suggested avoiding the term “facilitated angioplasty” since the purpose of fibrinolysis was not properly to “facilitate” angioplasty, but to restore anterograde flow of the culprit coronary artery.12
The first prospective clinical study that evaluated the pharmaco-invasive strategy was the GRACIA-2 trial,13 published in 2007. In this randomized clinical trial developed in Spain, a total of 212 patients with STEMI were assigned to receive reperfusion therapy with tenecteplase followed by angioplasty with stent placement in the first 3–12h versus PPCI with stent placement combining the use of abciximab within the first 3h. Primary endpoints were epicardial flow (TIMI) and the degree of myocardial perfusion (TMP), as well as infarct size and ventricular function at 6 weeks. The pharmaco-invasive strategy resulted in an increased frequency of complete epicardial reperfusion (21% vs. 6%); other outcomes including infarct size, left ventricular ejection fraction (LVEF), major bleeding, and the composite of death, reinfarction, stroke or repeat revascularization were similar in both groups at 6 months. The trial concluded that pharmaco-invasive strategy seems to produce earlier and better myocardial perfusion than PPCI. Additionally, the study suggested that the time after fibrinolysis and before coronary angiography could be safely extended for a few hours.
The TRANSFER AMI study14 included 1059 high-risk STEMI patients who were treated in hospitals without catheterization laboratory and received fibrinolytic treatment with tenecteplase. Patients were randomized between immediate transfer for percutaneous coronary intervention within 6h after fibrinolysis, or standard treatment (including rescue PCI, if required or delayed angiography). The average time for percutaneous coronary intervention after fibrinolysis was 3h in the immediate transfer group vs. 33h in the standard treatment group. The final composite outcome of death, reinfarction, heart failure, cardiogenic shock or recurrent ischemia, occurred less frequently in urgent coronary angiography group (11% vs. 17.2%). This benefit was primarily attributable to reduced reinfarction and recurrent ischemia. The incidence of bleeding was similar in both groups.
The NORDISTEMI study15 included 276 patients with STEMI treated with pharmacological reperfusion with tenecteplase in which the transfer to a center with cardiac catheterization laboratory would be more than 90min. Patients were randomized to immediate transfer for percutaneous angioplasty, and to conservative strategy and elective angiography. The primary end point of death, reinfarction, stroke or recurrent ischemia at one year, showed no difference between the groups (20.9% vs. 27.3%). However, combined outcome of reinfarction, death or stroke was lower in the immediate angioplasty group (6.0% vs. 15.9%).
Finally, STREAM trial16 included 1892 patients with STEMI who presented in the first 3h after the onset of symptoms that could not undergo PPCI within an hour after first medical contact. Patients were randomized to either, pharmaco-invasive strategy (fibrinolysis with tenecteplase and then angiography in the next 6 to 24h) or PPCI. The average first medical contact time was 60min, and the difference between the time from onset of symptoms to the administration of tenecteplase or angioplasty was 78min. There were no differences in the primary endpoint of death, reinfarction, heart failure or cardiogenic shock at 30 days. The researchers found an excess of intracranial bleeding in patients older than 75 years when it had achieved about 20% of recruitment. This led to an adjustment protocol to decrease to 50% of tenecteplase dose in patients older than 75 years; with this adjustment, the final rate of bleeding was similar between groups. Rescue angioplasty was required in 36% of patients randomized to tenecteplase group. After a year of patient follow up,17 the STREAM trial showed that overall mortality (6.7% vs. 5.9%) and cardiac mortality (4% vs. 4.1%) were similar between the patients treated with PPCI or pharmaco-invasive strategy.
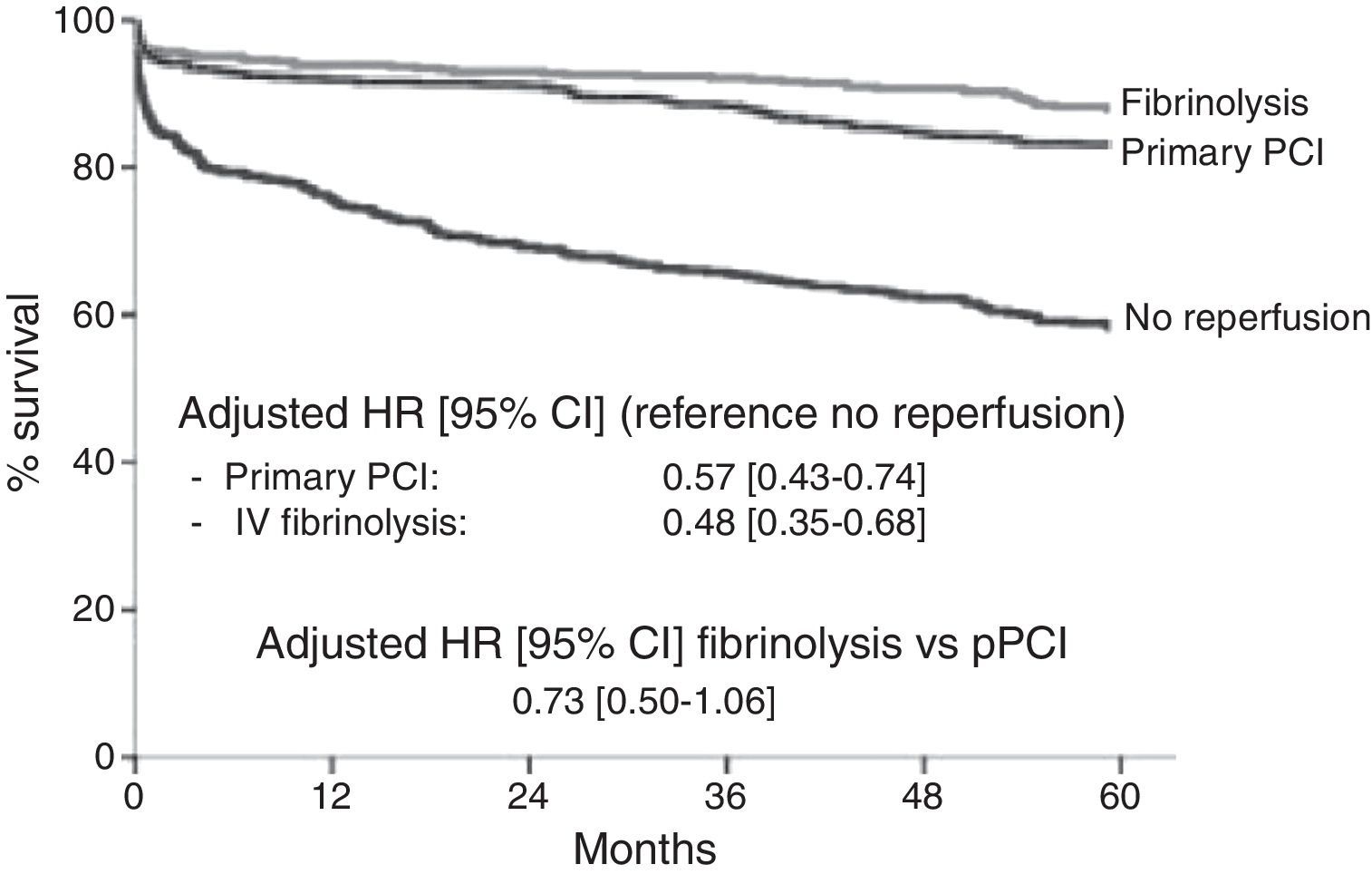
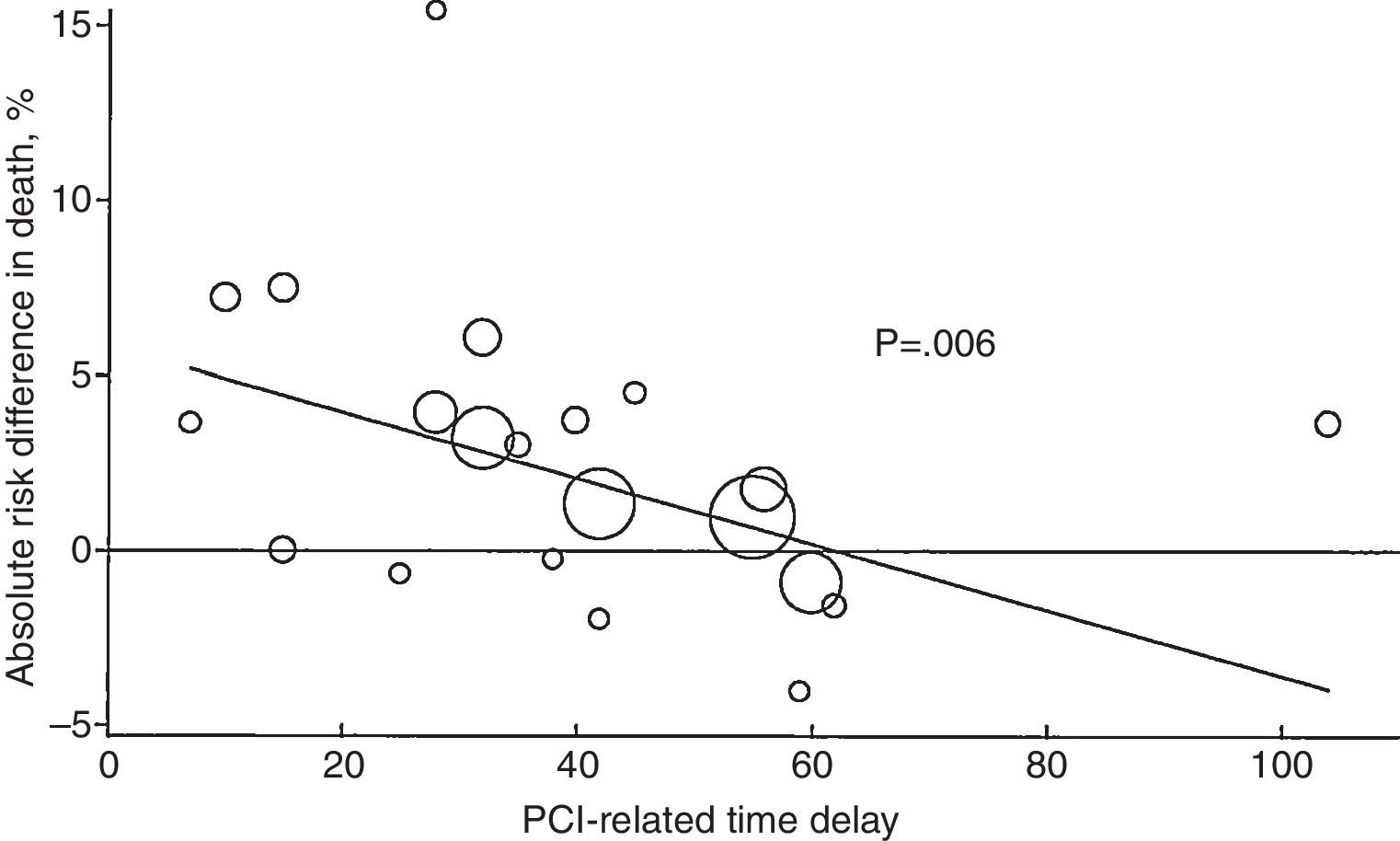
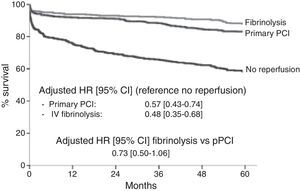
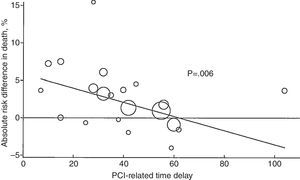
A real-world study in France (FAST-MI) reported mortality rates comparing the pharmaco-invasive strategy versus PPCI, and demonstrated better crude mortality rates for the first strategy, and reported similar results between the both of them after the propensity score analysis9 (Fig. 2). The mortality benefit associated with PPCI may be lost if door-to-balloon time is delayed by >1h compared to fibrinolytic therapy door-to-needle time18 (Fig. 3).
Results of the French FAST-MI registry showing five-year cumulative survival in patients with ST-segment-elevation myocardial infarction according to reperfusion therapy. CI indicates confidence interval; HR, hazard ratio; PCI, percutaneous coronary intervention; and PPCI, primary percutaneous coronary intervention. Reproduced from Ref. 9.
Absolute risk reduction in 4- to 6-week mortality rates with primary PCI as a function of PCI-related time delay. Circle sizes reflect the sample size of the individual study. Values >0 represent benefit and values <0 represent harm. Solid line, weighted meta-regression. Reproduced from Ref. 18.
Over this solid framework of evidence, we can affirm that pharmaco-invasive strategy is as effective and safe as angioplasty in treating STEMI.
With this background set up, pharmaco-invasive strategy is postulated as the choice to follow in communities, regions and countries where access to PPCI is limited by economic, geographical or sociocultural factors.
Pharmaco-invasive reperfusion strategy in developing countriesDifferent communities and regions have established programs that coordinate logistical services, pre-hospital emergencies facilities, tele-medicine, inter-hospital coordination and decision making technologies to improve the management and prognosis of patients with STEMI. In 2013 Solla et al. reported the experience of implementing a regional system of care for patients with STEMI in Bahia, Brazil,19 reaching a reperfusion rate of 75.6% in patients presenting within 12h of symptom onset. The study identified the key factors for the success of the coordinated program: the opportune recording of the initial ECG and diagnosis of STEMI (independently or aided by a tertiary care center), the coordination of inter-hospital transport to achieve the best reperfusion strategy, and identification of the hospitals with primary angioplasty 24h a day to complete the pharmaco-invasive strategy with coronary angiography and angioplasty as instructed by the algorithm developed locally.
In 2014 Dharma and colleagues shared the experience of the implementation of a networked system of cardiovascular care in Jakarta, Indonesia.20 Interventions included a community education program in basic life support, placement of automated external defibrillators (AED) in strategic locations, designing and using a system of pre-hospital electrocardiograms, a transfer protocol and specific in-hospital practices to reduce delays in reperfusion. After a year of program implementation, researchers reported an increase in interhospital referrals of patients with STEMI (greater awareness of medical personnel about STEMI), greater number of angioplasties (83% vs. 73%, p=0.005) and more patients reaching a door-to-needle time under 30min (84.5% vs. 80.2%, p<0.001). However, there was no difference in the door-to-balloon time, the rate of patients who presented outside the time window, neither in-hospital mortality in 2011 compared to 2008–2010. The authors concluded that then following points may be improved in the future:
- •
Deficiencies in pre-hospital flowcharts assigned to emergency transportation personnel
- •
Pre-hospital electrocardiograms
- •
Continuing education of staff involved at any level of the system
Finally, the STEMI-INDIA group, in the region of Tamil Nadu, published their experience by organizing the health system in a number of networks where rural hospitals were grouped by geo-location around “hub” hospitals, with the intention to reduce treatment delays and improve the rate of reperfusion and myocardial infarction outcomes. The results showed a reduction in the time of first medical contact to reperfusion, and promoted the formation of a coalition that included the regional government, the emergency ambulance service and a non-profit national association (STEMI-INDIA) with the goal of advice and coordinate the efforts of all parties involved.21
The experience shared by the authors of these three systems, recently introduced in these three developing countries, emphasizes the importance of several issues:
- •
The important role of medical services in pre-hospital emergency care facilities as a crucial tool to begin the attention flow chart
- •
The need for interventions dedicated to improve STEMI quality care including time of first medical contact, door-to-ECG time, ECG-onset of reperfusion time, as well as transfer times, and not just the door-to-balloon time
- •
A strong legislative and financial government support
- •
The need for continuing education and certification
- •
The need to allow feedback in the short, intermediate and long term, as this information will be used as representative markers to adjust policies.
Currently, there is no universal STEMI reperfusion program in México. Great achievements have been accomplished thanks to the “Código Infarto” initiative, a prompt STEMI recognition and treatment strategy sponsored by the Mexican Society of Interventional Cardiology (SOCIME) and Mexican Institute of Social Security (IMSS). Since its implementation, this initiative has successfully established STEMI management programs in several states of México. However, a universal reperfusion strategy is still lacking, especially for those who are not under a program of social security and those who live in sub-urban and rural areas of the country (at least 25% of the total population22).
Only 15% of the hospitals in México have a catheterization laboratory, and not all are available 24h a day, seven days a week. The number of coronary revascularization procedures is the lowest among the OECD countries (6 procedures per 100,000 populations per year), ten times below the next country on the list (Chile, 62 procedures per 100,000 populations per year) and 36.5 times below the average. Given these data and the scientific evidence presented above, the pharmaco-invasive strategy is the most suitable strategy for STEMI reperfusion treatment in our country, especially if full coverage is planned, including those patients in non-urban and difficult access areas.
Mexico City and the metropolitan area of the Valley of Mexico is a megalopolis of 20.1 million inhabitants, immersed in critical transportation and mobility problems. Land access to certain areas of the city can be extremely difficult in peak traffic hours when road conditions are chaotic, a situation that complicates patient transporting to a primary-PCI capable hospital. The Mexico City Government in joint effort with the National Institute of Cardiology has developed a pharmaco-invasive reperfusion treatment program to ensure effective and timely reperfusion in STEMI. This pilot model comprises a network of care at all three levels of health, and includes the following:
- •
A system of early pharmacological reperfusion treatment in the primary care centers.
- •
A telemedicine system with electrocardiogram digital transfer between primary care and the National Institute of Cardiology in order to help primary care physician to decide if the first strategy for reperfusion would be fibrinolytics or primary-PCI according to the scenario.
- •
An inter-hospital transport network to ensure primary-PCI or early percutaneous coronary intervention after fibrinolysis in one of the coronary-catheterization capable centers.
- •
A training program and the certification of the health care personal (physicians and nurses) for the treatment of STEMI.
With the previous strategy, it is expected to prioritize early diagnosis and effective pharmacological reperfusion, and ensure the presence of qualified personal for reperfusion therapy at optimal times in critical scenarios. Also the National Institute of cardiology will coordinate the transfer protocol to a highly level facility (either to primary angioplasty or pharmaco-invasive reperfusion strategy).
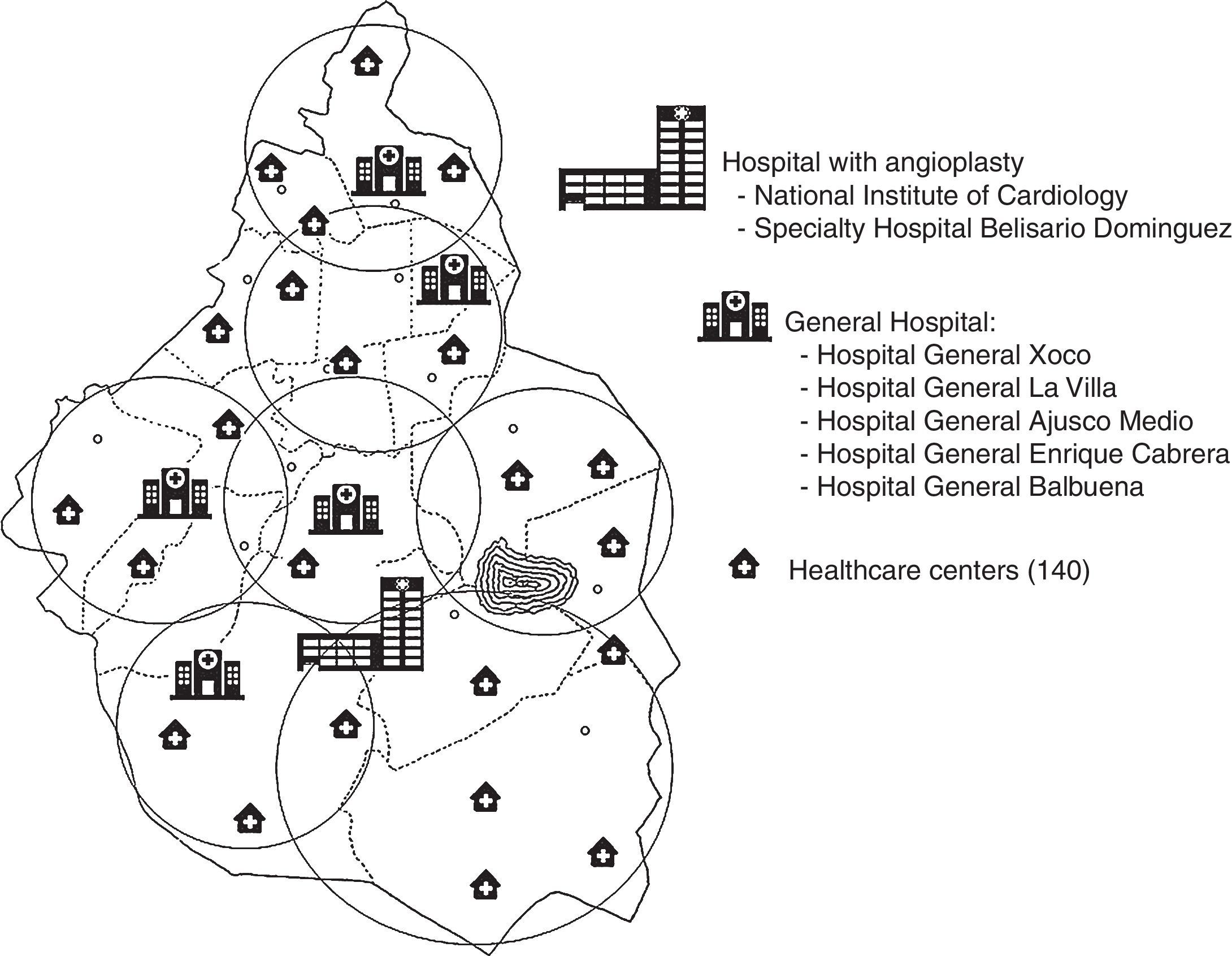
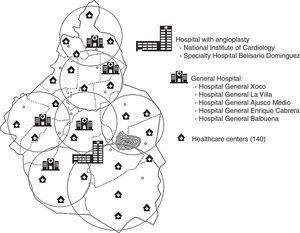
A telemedicine system with electrocardiogram transfer between primary care and the National Institute of Cardiology was established in order to aid primary care physicians to decide if first reperfusion strategy should be fibrinolytics or primary-PCI, according to individual scenario. A geo-location reference based system comprising 140 primary care centers, 5 general hospitals and 2 specialty hospitals where coronary angiography is performed (Fig. 4) is intended to be available in the near future to assist patient management logistics.
Final messageThe authors of this manuscript strongly believe that pharmacoinvasive strategy is the therapeutic of choice for STEMI in México, based on social, economic and health-care driven factors. The joint program between the Government of Mexico City and the National Institute of Cardiology binds the efforts to guarantee an early and safe reperfusion therapy. The program intends to reduce morbidity and mortality associated with myocardial infarction, and strong emphasis is made for other regions to adopt local strategies that allow timely reperfusion and improve the prognosis of STEMI in México.
FundingNo endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.