Degenerative aortic valve stenosis (AS) is the most common valvular heart disease. About two-thirds of all valve operations are for aortic valve replacement (AVR). After onset of symptoms (angina, syncope or heart failure) severe aortic stenosis has a poor prognosis with an average survival of two or three years and a high risk of sudden death.1 According to the ACC/AHA and the European Society of Cardiology/European Association for Cardio-Thoracic Surgery Guidelines for management of patients with heart valve disease, surgical aortic valve replacement is an indication class I in symptomatic patients with AS, and for patients with severe AS undergoing CABG or surgery of the aorta or other heart valves, and patients with severe AS and LV systolic dysfunction (ejection fraction<50%).1,2 It is generally accepted that surgical AVR can improve the functional class and prolong survival. Nevertheless, 30% of elderly patients with symptomatic severe aortic valve stenosis do not undergo AVR, attributed to “inoperable” conditions or extremely high surgical risk, such as advanced age, pulmonary, renal, hepatic disease, prior cerebrovascular event, weakness or frailty, that increases the risk of poor outcomes.3 Recently, transcatheter aortic valve implantation (TAVI) has become a treatment option for patients with high or prohibitive surgical risk. The concept of transcatheter valve implantation was evaluated by Andersen in 1992 in a porcine model.4 In 2002 the first TAVI was accomplished by Dr. Alan Cribier, via a transeptal antegrade delivery technique using a balloon-expandable aortic valve.5 After this pioneering procedure, several registries and one multicenter randomized control trial have been published worldwide (Fig. 1).6 We describe the first case of TAVI performed in Mexico using a balloon-expandable Edwards Sapien XT transcatheter heart valve, which means the beginning of the program of TAVI with this kind of valve in our institution.
A 77-year-old woman with severe symptomatic aortic stenosis was referred to our hospital for treatment. She was in NYHA functional class II, with a background of systemic arterial hypertension, hyperuricemia, cervical spine surgery, lumbar spine trauma treated with surgical fixation, fibromyalgia, chronic deep venous insufficiency, and chronic renal failure with a creatinine level of 2.0mg/dL. Furthermore, six months ago, she was diagnosed with a sick sinus syndrome (bradycardia-tachycardia syndrome), and underwent permanent pacemaker implantation.
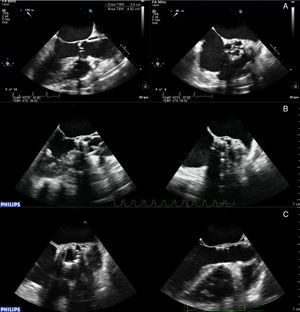
Transesophageal echocardiography (TEE) demonstrated a severe degenerative aortic stenosis with a left ventricular ejection fraction of 40%. The mean aortic pressure gradient was 40mmHg and the calculated aortic valve area was 0.4cm2, which was corroborated with TEE planimetry. The screening showed no significant coronary artery stenosis and mildly calcified aortic annulus diameter of 24.6mm. CT angiography demonstrated a suitable anatomy for a transfemoral approach having moderate aortic tortuosity and mildly calcified femoroiliac arteries with a diameter >6.5mm. She was considered at high risk for surgical treatment by the heart team due to frailty, thoracic deformity (hostile chest), Logistic EuroScore of 15%, and severe comorbidities.
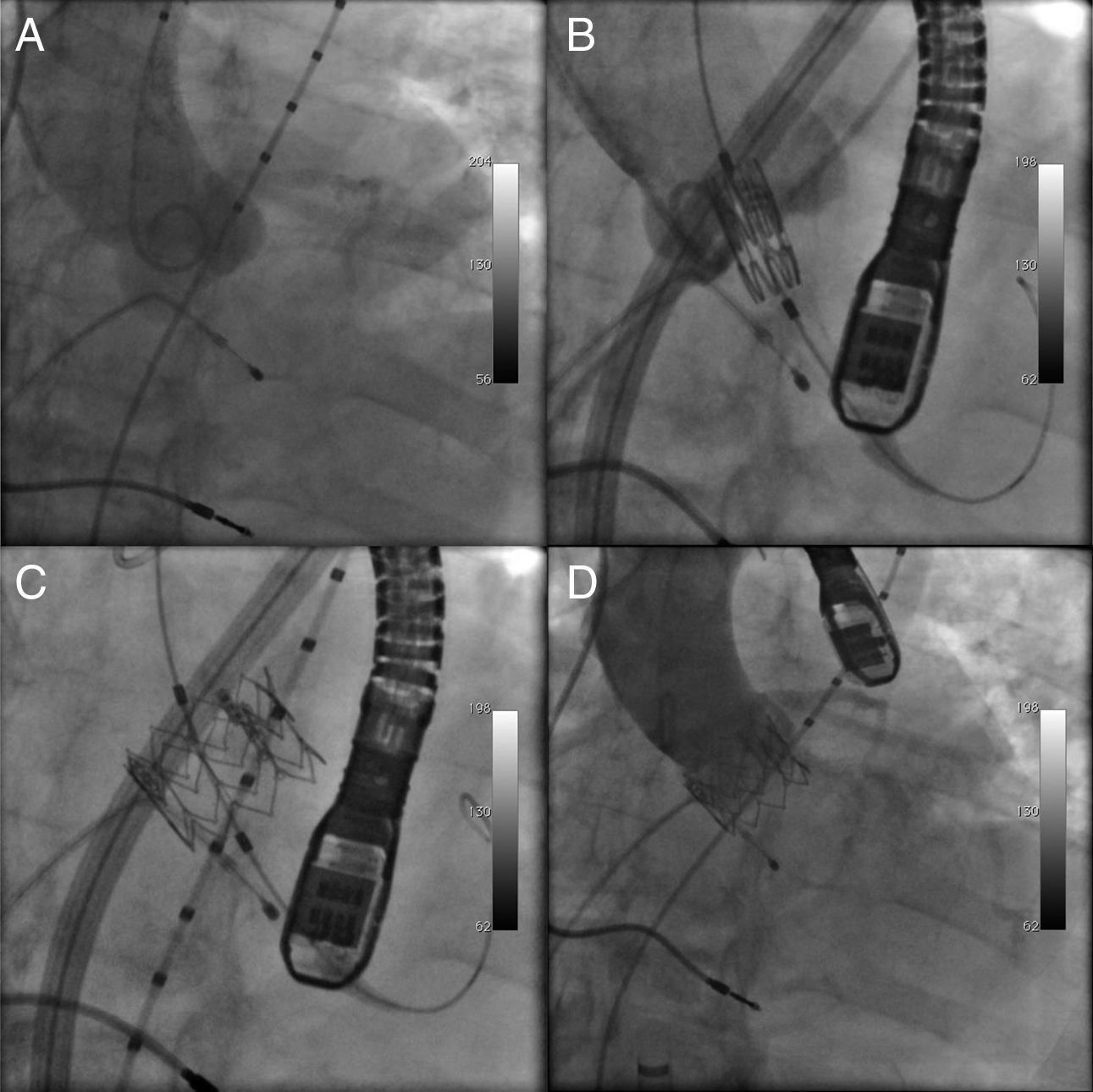
On February 5, 2013, the TAVI procedure was performed using transfemoral approach with surgical back-up under general anesthesia and TEE guidance in a standard catheterization laboratory (Fig. 2). We punctured the left femoral artery and vein and inserted a 6Fr pigtail in the ascending aorta and a 6Fr temporary pacing wire in the right ventricle. Intravenous antibiotics and heparin were administrated as per protocol. The right femoral artery was surgically exposed, punctured and a Novaflex® plus delivery system was deployed. Initial angiography confirmed the optimum view with the alignment of the three aortic leaflets. The aortic valve was crossed with a hydrophilic wire with the support of a 5Fr Amplatz left one catheter and was subsequently exchanged for a previously preformed an Amplatz super stiff guidewire (Boston Scientific, MA). Predilatation of the aortic valve was done with a 20mm Edwards balloon catheter (Edwards Lifesciences, Irvine, CA, USA) and rapid ventricular pacing. After predilatation a 26mm Edwards Sapien XT prosthesis (Edwards Lifesciences, Irvine, CA, USA) was brought into its position by using a dynamic expansion mechanism of the delivery system, and was successfully implanted. The control aortography and TEE demonstrated a well positioned aortic valve prosthesis with a mild perivalvular leak. The patient remained hemodynamically stable throughout the procedure and was taken to the cardiac surgery intensive care unit extubated and in stable condition. TEE performed after the procedure revealed a mean pressure gradient of 5mmHg, and adequate left ventricular function. After two days in the critical care unit, she was discharged from the hospital three days later. At two months of follow-up the patient persisted without of any cardiovascular event and in NYHA class I. Transthoracic echocardiography confirmed an aortic valve area of 1.7cm2, with a mean pressure gradient of 5mmHg.
TAVI has emerged as a highly effective procedure for aortic valve stenosis in patients with high surgical risk or “inoperable” state.7–10 Until now, two different TAVI systems are widely used, the balloon-expandable Edwards Sapien transcatheter heart valve (Edwards Lifesciences, Irvine, CA, USA) and the self-expandable Medtronic CoreValve (Medtronic, Minneapolis, MN, USA).6 After the innovative procedure of Dr. Cribier, several registries and one randomized trial have demonstrated that TAVI is feasible and safe for patients with severe aortic valve stenosis and high or prohibitive surgical risk.6–10
Several series and registries have reported a technical success of 95% and 30-day survival over 90%, using a balloon-expandable Edwards Sapien transcatheter heart valve (Edwards Lifesciences, Irvine, CA, USA).6
According to the study PARTNER trial (Placement of AoRTic TraNscathetER valves Trial), which is the only randomized trial, global mortality at one year of follow-up on inoperable patients was higher in the group that received standard treatment as compared with TAVI (50.7% vs. 30.7%, p<0.001). Major stroke and vascular complications rates were higher in the TAVI group at 30-day.7 Overall mortality was significantly reduced at two years with TAVI (43.3% vs. 68.0%, p<0.001). During the two years of follow-up, 83.1% with TAVI were in functional class NYHA I–II compared with 42.5% of standard treatment.8
In high-risk patients, the PARTNER trial reported an early mortality of 3.4% with TAVI and 6.5% with surgery (p=0.07). Vascular complications were higher in the TAVI group and major bleeding and new-onset atrial fibrillation in the surgical group.9 Two-year mortality was similar between the groups (33.9% TAVI vs. 35.0% surgery, p=0.78). The high risk of stroke with TAVI in the early phase was reduced over time. However, the association of paravalvular regurgitation with increased late mortality was documented.10
TAVI has proven to improve symptoms, reduce valvular gradient, and the death rate in inoperable patients. In selected patients at high surgical risk, TAVI is an alternative to surgery.
We are sure that the refinement of the technique and technological development will reduce the complications related with this procedure.
TAVI has emerged as a real alternative for patients with high surgical risk or unsuitable for surgery. We reported the first case in Mexico of this relative new technique using a balloon-expandable Edwards Sapien XT transcatheter heart valve, which is widely used in highly qualified centers only.
FinancingNo type of support was received to perform this article.
Conflicts of interestThe authors declare having no conflicts of interest.